
ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
A. Preamble
This is a legal contract between You and Us subject to the receipt of full
premium, Disclosure to Information Norm including the information
provided by You in the Proposal Form and the terms, conditions and
exclusions of this Policy.
If any Claim arising as a result of a Disease/Illness or Injury that
occurred during the Policy Period becomes payable, then We shall
paythebenetsinaccordancewithterms,conditionsandexclusions
of the Policy subject to availability of Sum Insured and Cumulative
Bonus (if any). All limits mentioned in the Policy Schedule are
applicable for each Policy Year of coverage.
B Denitions
B.I StandardDenitions
1. Accidentmeans a sudden, unforeseen and involuntary event caused
by external, visible and violent means.
2. AnyoneIllness means continuous Period of illness and it includes
relapse within 45 days from the date of last consultation with the
Hospital/Nursing Home where the treatment was taken.
3. AYUSH Hospital is a healthcare facility wherein medical/ surgical/
para-surgical treatment procedures and interventions are carried out
by AYUSH Medical Practitioner(s) comprising any of the following:
1. Central or State Government AYUSH Hospital; or
2. Teaching hospitals attached to AYUSH College recognized by the
Central Government / Central Council of Indian Medicine / Central
Council for Homeopathy; or
3. AYUSH Hospital, standalone or co-located with In-patient
healthcare facility of any recognized system of medicine, registered
with the local authorities, wherever applicable, and is under the
supervisionofaqualiedregistered AYUSH Medical Practitioner
and must comply with all the following criterion:
i) HavingatleastveIn-patientbeds;
ii) HavingqualiedAYUSHMedicalPractitionerinchargeroundthe
clock;
iii) Having dedicated AYUSH therapy sections as required and/or
has equipped operation theatre where surgical procedures are
to be carried out;
iv) Maintaining daily record of the patients and making them
accessible to the insurance company’s authorized
representative.
4. Cashless Facility means a facility extended by the insurer to the
insured where the payments, of the costs of treatment undergone by
the insured in accordance with the Policy terms and conditions, are
directly made to the network provider by the insurer to the extent pre-
authorization approved.
5. Co-payment means a cost-sharing requirement under a health
insurance policy that provides that the policyholder/insured will bear a
specied percentage of the admissible claim amount. A co-payment
does not reduce the Sum Insured.
6. ConditionPrecedent means a policy term or condition upon which the
Insurer’s Liability under the Policy is conditional upon.
7. CongenitalAnomaly refers to a condition(s) which is present since
birth, and which is abnormal with reference to form, structure or
position.
a. Internal Congenital Anomaly - which is not in the visible and
accessible parts of the body is called Internal Congenital Anomaly
b. ExternalCongenitalAnomaly- Congenital Anomaly which is in the
visible and accessible parts of the body.
8. CriticalIllnessmeans the following:
a) CancerofSpeciedSeverity
A malignant tumor characterized by the uncontrolled growth &
spread of malignant cells with invasion & destruction of normal
tissues. This diagnosis must be supported by histological evidence
of malignancy. The term cancer includes leukemia, lymphoma and
sarcoma.
The following are excluded –
i. All tumors which are histologically described as carcinoma in
situ, benign, pre-malignant, borderline malignant, low malignant
potential, neoplasm of unknown behavior, or non-invasive,
including but not limited to: Carcinoma in situ of breasts, Cervical
dysplasia CIN-1, CIN -2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. Alltumorsoftheprostateunlesshistologicallyclassiedashaving
a Gleason score greater than 6 or having progressed to at least
clinicalTNMclassicationT2N0M0
v. All Thyroid cancers histologically classied as T1N0M0 (TNM
Classication)orbelow;
vi. Chronic lymphocytic leukemia less than RAI stage 3
vii. Non-invasive papillary cancer of the bladder histologically
describedasTaN0M0orofalesserclassication,
viii.All Gastro-Intestinal Stromal Tumors histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of
lessthanorequalto5/50HPFs;
ix. All tumors in the presence of HIV infection.
b) MyocardialInfarction(FirstHeartAttackofSpecicSeverity)
I Therstoccurrenceofheartattackormyocardialinfarction,which
means the death of a portion of the heart muscle as a result of
inadequate blood supply to the relevant area. The diagnosis for
this will be evidenced by all of the following criteria:
i. a history of typical clinical symptoms consistent with the diagnosis
of Acute Myocardial Infarction (for e.g. typical chest pain)
ii. new characteristic electrocardiogram changes
iii. elevation of infarction specic enzymes, Troponins or other
specicbiochemicalmarkers.
II The following are excluded:
i. Other acute Coronary Syndromes
ii. Any type of angina pectoris.
iii. A rise in cardiac biomarkers or Troponin T or I in absence
of overt ischemic heart disease OR following an intra-arterial
cardiac procedure.
c) OpenChestCABG
I The actual undergoing of heart surgery to correct blockage or
narrowing in one or more coronary artery (s), by coronary artery
bypass grafting done via a sternotomy (cutting through the breast
bone) or minimally invasive keyhole coronary artery bypass
procedures. The diagnosis must be supported by a coronary
angiographyandtherealizationofsurgeryhastobeconrmedby
a cardiologist.
II The following are excluded:
a. Angioplasty and/or any other intra-arterial procedures
d) OpenHeartReplacementorRepairofHeartValves
The actual undergoing of open-heart valve surgery is to replace or repair
one or more heart valves, as a consequence of defects in,
abnormalities of, or disease-affected cardiac valve(s). The diagnosis
of the valve abnormality must be supported by an echocardiography
and the realization of surgery has to be conrmed by a specialist
medical practitioner. Catheter based techniques including but not
PolicyContract
Plans:Protect|Advantage
MANIPALCIGNAPROHEALTHPRIME

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
limited to, balloon valvotomy/ valvuloplasty are excluded.
e) ComaofSpeciedSeverity
1. A state of unconsciousness with no reaction or response to
external stimuli or internal needs.
This diagnosis must be supported by evidence of all of the following:
i. no response to external stimuli continuously for at least 96 hours;
ii. life support measures are necessary to sustain life; and
iii. permanentneurologicaldecitwhichmustbeassessedatleast30
days after the onset of the coma.
2. The condition has to be conrmed by a specialist medical
practitioner. Coma resulting directly from alcohol or drug abuse is
excluded.
f) KidneyFailureRequiringRegularDialysis
End stage renal disease presenting as chronic irreversible failure
of both kidneys to function, as a result of which either regular
renal dialysis (hemodialysis or peritoneal dialysis) is instituted or
renaltransplantationiscarriedout.Diagnosishastobeconrmed
by a specialist medical practitioner.
g) StrokeResultinginPermanentSymptoms
Any cerebrovascular incident producing permanent neurological
sequelae. This includes infarction of brain tissue, thrombosis in
an intracranial vessel, hemorrhage and embolization from an
extracranialsource.Diagnosishastobeconrmedbyaspecialist
medical practitioner and evidenced by typical clinical symptoms
aswellastypicalndingsinCTscanorMRIofthebrain.Evidence
ofpermanentneurologicaldecitlastingforatleast3monthshas
to be produced.
The following are excluded:
1. Transient ischemic attacks (TIA)
2. Traumatic injury of the brain
3. Vascular disease affecting only the eye or optic nerve or
vestibular functions.
h) MajorOrgan/BoneMarrowTransplant
The actual undergoing of a transplant of:
1. One of the following human organs: heart, lung, liver, kidney,
pancreas, that resulted from irreversible end-stage failure of the
relevant organ, or
2. Human bone marrow using hematopoietic stem cells. The
undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
i. Other stem-cell transplants
ii. Where only islets of langerhans are transplanted
i) PermanentParalysisofLimbs
Total and irreversible loss of use of two or more limbs as a result of
injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be permanent
with no hope of recovery and must be present for more than 3 months.
j) MotorNeuronDiseasewithPermanentSymptoms
Motor neuron disease diagnosed by a specialist medical practitioner
as spinal muscular atrophy, progressive bulbar palsy, amyotrophic
lateral sclerosis or primary lateral sclerosis. There must be progressive
degeneration of corticospinal tracts and anterior horn cells or bulbar
efferent neurons. There must be current signicant and permanent
functional neurological impairment with objective evidence of motor
dysfunction that has persisted for a continuous period of at least 3
months.
k)MultipleSclerosiswithPersistingSymptoms
I. TheunequivocaldiagnosisofDeniteMultipleSclerosisconrmed
and evidenced by all of the following:
i. investigationsincludingtypicalMRIndingswhichunequivocally
conrmthediagnosistobemultiplesclerosisand
ii. there must be current clinical impairment of motor or sensory
function, which must have persisted for a continuous period of
at least 6 months.
II. Other causes of neurological damage such as SLE and HIV are
excluded.
9. CumulativeBonus
Cumulative Bonus means any increase in the Sum Insured granted by
the insurer without an associated increase in premium.
10. DayCareCentre - A day care centre means any institution established
for day care treatment of illness and / or injuries or a medical set -up
within a hospital and which has been registered with the local authorities,
wherever applicable, and is under the supervision of a registered and
qualied medical practitioner AND must comply with all minimum
criteria as under:-
a. hasqualiednursingstaffunderitsemployment
b. hasqualiedmedicalpractitioner(s)incharge
c. has a fully equipped operation theatre of its own where surgical
procedures are carried out
d. maintains daily records of patients and will make these accessible
to the Insurance Company’s authorized personnel.
11. Day Care Treatment means medical treatment, and/or surgical
procedure which is:
i) Undertaken under General or Local Anesthesia in a hospital/day
care centre in less than 24 hours because of technological
advancement, and
ii) Which would have otherwise required a Hospitalization of more
than 24 hours.
Treatment normally taken on an out-patient basis is not included in the
scopeofthisdenition.
12. Deductible means a cost-sharing requirement under a health
insurance policy that provides that the Insurer will not be liable for a
specied rupee amount in case of indemnity policies and for a
speciednumberofdays/hoursincaseofhospitalcashpolicies,which
willapplybeforeanybenetsarepayablebytheinsurer.Adeductible
does not reduce the sum insured.
13. Dental Treatment - Dental treatment means a treatment related to
teeth or structures supporting teeth including examinations, llings
(where appropriate), crowns, extractions and surgery excluding any
form of cosmetic surgery/implants.
14. DisclosuretoInformationNorm means the Policy shall be void and
all premium paid hereon shall be forfeited to the Company, in the event
of misrepresentation, mis-description or non-disclosure of any material
fact.
15. DomiciliaryHospitalization means medical treatment for an illness/
disease/injury which in the normal course would require care and
treatment at a hospital but is actually taken while conned at home
under any of the following circumstances:
a) the condition of the patient is such that he/she is not in a condition
to be removed to a hospital, or
b) the patient takes treatment at home on account of non-availability
of room in a hospital.
16. Emergency Care means management for a severe illness or injury
which results in symptoms which occur suddenly and unexpectedly,
and requires immediate care by a medical practitioner to prevent death
or serious long term impairment of the insured person’s health
17. GracePeriodmeansthespeciedperiodoftimeimmediatelyfollowing
the premium due date during which a payment can be made to renew
or continue a policy in force without loss of continuity benets such
as waiting periods and coverage of pre-existing diseases. Coverage is
not available for the period for which no premium is received.
18. Hospitalmeans any institution established for In-patient care and day
care treatment of illness and/or injuries and which has been registered
as a hospital with the local authorities, under the Clinical Establishments
(Registration and Regulation) Act, 2010 or under the enactments
specied under the Schedule of Section 56 (1) of the said Act OR

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
complies with all minimum criteria as under:
i. hasqualiednursingstaffunderitsemploymentroundtheclock;
ii. has at least 10 In-patient beds, in towns having a population of
less than 10,00,000 and at least 15 In-patient beds in all other
places;
iii. hasqualiedmedicalpractitioner(s)inchargeroundtheclock;
iv. has a fully equipped operation theatre of its own where surgical
procedures are carried out
v. maintains daily records of patients and makes these accessible to
the Insurance company’s authorized personnel.
19. Hospitalization or Hospitalized means admission in a hospital for
a minimum period of 24 consecutive In-patient Care hours except for
speciedprocedures/treatments,wheresuchadmissioncouldbefora
period of less than 24 consecutive hours.
20. Illness means a sickness or disease or pathological condition leading
to the impairment of normal physiological function and requires medical
treatment.
a) Acutecondition- Acute condition is a disease, illness or injury that
is likely to respond quickly to treatment which aims to return the
person to his or her state of health immediately before suffering
the disease/illness/injury which leads to full recovery
b) Chroniccondition-Achronic condition isdenedasa disease,
illness, or injury that has one or more of the following characteristics:
1. it needs ongoing or long-term monitoring through consultations,
examinations, check-ups, and /or tests
2. it needs ongoing or long-term control or relief of symptoms
3. it requires rehabilitation for the patient or for the patient to be
specially trained to cope with it
4. itcontinuesindenitely
5. it recurs or is likely to recur
21. Injury means accidental physical bodily harm excluding illness or
disease solely and directly caused by external, violent and visible and
evidentmeanswhichisveriedandcertiedbyaMedicalPractitioner.
22. In-patientCare means treatment for which the Insured Person has to
stay in a hospital for more than 24 hours for a covered event.
23. IntensiveCare Unit means an identied section, ward or wing of a
Hospital which is under the constant supervision of a dedicated
medical practitioner (s), and which is specially equipped for the
continuous monitoring and treatment of patients who are in a critical
condition, or require life support facilities and where the level of care
and supervision is considerably more sophisticated and intensive than
in the ordinary and other wards.
24. Maternityexpenses means:
i. Medical treatment expenses traceable to childbirth (including
complicated deliveries and caesarean sections incurred during
Hospitalization);
ii. Expenses towards lawful medical termination of pregnancy during
the Policy Period
25. Medical Advice means any consultation or advice from a Medical
Practitioner including the issue of any prescription or follow-up
prescription.
26. Medical Expenses means those expenses that an Insured Person
has necessarily and actually incurred for medical treatment on account
of Illness or Accident on the advice of a Medical Practitioner, as long as
these are no more than would have been payable if the Insured Person
had not been insured and no more than other hospitals or doctors in
the same locality would have charged for the same medical treatment.
27. Medically Necessary Treatment means any treatment, tests,
medication, or stay in Hospital or part of a stay in Hospital which
i. Is required for the medical management of the Illness or injury
suffered by the Insured;
ii. Must not exceed the level of care necessary to provide safe,
adequate and appropriate medical care in scope, duration or
intensity.
iii. Must have been prescribed by a Medical Practitioner.
iv. Must conform to the professional standards widely accepted in
international medical practice or by the medical community in
India.
28. Medical Practitioner A Medical practitioner means a person who
holds a valid registration from the medical council of any state or
Medical Council of India or Council for Indian Medicine or for
Homeopathy set up by Government of India or a State Government
and is and is thereby entitled to practice medicine within its jurisdiction;
and is acting within the scope and jurisdiction of license.
29. NewBornBaby means baby born during the Policy Period and is Aged
upto90days
30. NetworkProvider means hospitals or health care provider enlisted by
an insurer, TPA or jointly by an insurer and TPA to provide medical
services to an insured by a cashless facility.
31. Non-NetworkProviderAny hospital, day care centre or other provider
that is not part of the network.
32. Notication of Claim Notication of claim means the process of
intimating a claim to the insurer or TPA through any of the recognized
modes of communication.
33. Migration means, the right accorded to health insurance policyholders
(including all members under family cover and members of group
Health insurance policy), to transfer the credit gained for pre-existing
conditions and time bound exclusions, with the same insurer.
34. OPDTreatment is one in which the Insured visits a clinic / hospital
or associated facility like a consultation room for diagnosis and
treatment based on the advice of a Medical Practitioner. The Insured is
not admitted as a day care or In-patient.
35. Pre-existingDisease means any condition, ailment, injury or disease
a. That is/are diagnosed by a physician within 48 months prior to the
effective date of the policy issued by the insurer or
b. For which medical advice or treatment was recommended by, or
received from, a physician within 48 months prior to the effective
date of the policy issued by the insurer or its reinstatement.
36. Pre-hospitalizationMedicalExpenses
Pre-hospitalization Medical Expenses means medical expenses
incurredduringpredenednumberofdaysprecedingtheHospitalization
of the Insured Person, provided that:
- Such Medical Expenses are incurred for the same condition for
which the Insured Person’s Hospitalization was required, and
- The In-patient Hospitalization claim for such Hospitalization is
admissible by the Insurance Company.
37. Post-hospitalizationMedicalExpenses
Post-hospitalization Medical Expenses means medical expenses
incurred during predened number of days immediately after the
insured person is discharged from the hospital provided that:
i. Such Medical Expenses are for the same condition for which the
insured person’s Hospitalization was required, and
ii. The In-patient Hospitalization claim for such Hospitalization is
admissible by the insurance company.
38. Portability means the right accorded to an individual health insurance
policyholder (including all members under family cover), to transfer the
credit gained for pre-existing conditions and time bound exclusions,
from one insurer to another insurer.
39. QualiedNurse means a person who holds a valid registration from
the Nursing Council of India or the Nursing Council of any state in
India.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
40. ReasonableandCustomaryChargesmeans the charges for services
orsupplies,whicharethestandardchargesforthespecic provider
and consistent with the prevailing charges in the geographical area for
identical or similar services, taking into account the nature of the illness
/ injury involved.
41. Renewal means the terms on which the contract of insurance can be
renewed on mutual consent with a provision of grace period for treating
the renewal continuous for the purpose of gaining credit for pre-existing
diseases, time-bound exclusions and for all waiting periods.
42. Room Rent - Room Rent means the amount charged by a Hospital
towards Room and Boarding expenses and shall include the associated
medical expenses.
43. Surgery or Surgical Procedure means manual and / or operative
procedure (s) required for treatment of an illness or injury, correction
of deformities and defects, diagnosis and cure of diseases, relief from
suffering and prolongation of life, performed in a hospital or day care
centre by a medical practitioner
44. Unproven/Experimental treatment means the treatment including
drug experimental therapy which is not based on established medical
practice in India, is treatment experimental or unproven.
B.II SpecicDenitions
1. Age or Aged is the age at last birthday, and which means completed
years as at the date of Inception of the Policy.
2. Ambulance means a road vehicle operated by a licensed/authorized
service provider and equipped for the transport and paramedical
treatment of the person requiring medical attention.
3. Annexure means a document attached and marked as Annexure to
this Policy
4. Associated Medical Expenses. shall include Room Rent, nursing
charges, operation theatre charges, fees of Medical Practitioner/
surgeon/ anesthetist/ Specialist, excluding cost of pharmacy and
consumables, cost of implants and medical devices, cost of diagnostics
conducted within the same Hospital where the Insured Person has
been admitted. It shall not be applicable for Hospitalization in ICU.
Associated Medical Expenses shall be applicable for covered
expenses, incurred in Hospitals which follow differential billing based
on the room category.
5. AYUSH treatment refers to the medical and /or hospitalization
treatments given under Ayurveda, Yoga and Naturopathy, Unani,
Siddha and Homeopathy Systems.
6. InceptionDatemeanstheInceptiondateofthisPolicyasspeciedin
the Policy Schedule
7. CosmeticSurgerymeansSurgeryorMedicalTreatmentthatmodies,
improves, restores or maintains normal appearance of a physical
feature, irregularity, or defect.
8. CoveredRelationshipsshallinclude spouse, children, brother and
sister of the Policyholder who are children of same parents, father,
mother, grandparents, grandchildren, parent in laws, son in law,
daughter in law, uncle, aunt, niece and nephew.
9. DependentChild A dependent child refers to a child (natural or legally
adopted),whoisnanciallydependentonthePolicyHolder,doesnot
have his / her independent source of income, is up to the age of 25
years.
10. Emergency shall mean a serious medical condition or symptom
resulting from injury or sickness which arises suddenly and
unexpectedly, and requires immediate care and treatment by a medical
practitioner, generally received within 24 hours of onset to avoid
jeopardy to life or serious long term impairment of the insured person’s
health, until stabilization at which time this medical condition or
symptom is not considered an emergency anymore.
11. Family Floater means a Policy described as such in the Policy
Schedule where under You and Your Dependents named in the Policy
Schedule are insured under this Policy as at the Inception Date. The
Sum Insured for a Family Floater means the sum shown in the Policy
Schedule which represents Our maximum liability for any and all claims
made by You and/or all of Your Dependents during each Policy Period.
12. HighDependencyUnit/ward is a specially staffed and equipped area
of a hospital that provides a level of care intermediate between
intensive care and the general ward care
13. Indian Resident - An individual will be considered to be resident of
India, if he is in India for a period or periods amounting in all to one
hundred and eighty-two days or more, in the immediate preceding 365
days.
14. In-patientmeans an Insured Person who is admitted to hospital and
stays for at least 24 consecutive hours for the sole purpose of receiving
treatment.
15. InsuredPerson means the person(s) named in the Policy Schedule,
who is / are covered under this Policy, for whom the insurance is
proposed and the appropriate premium paid.
16. IUI - Intrauterine insemination (IUI) is a fertility treatment where sperm
are placed directly into a woman’s uterus
17. IVF - In vitro fertilization (IVF) is a type of assistive reproductive
technology (ART). It involves retrieving eggs from a woman’s ovaries
and fertilizing them with sperm.
18. MaternitySumInsuredmeansthesumspeciedinthePolicySchedule
againstthebenet
19. Policymeans this Terms & Conditions document, the Proposal Form,
PolicySchedule,Add-OnBenetDetails(ifapplicable)andAnnexures
which form part of the Policy contract including endorsements, as
amended from time to time which form part of the Policy Contract and
shall be read together.
20. PolicyPeriod means the period between the inception date and the
expirydateofthepolicyasspeciedinthePolicyScheduleorthedate
of cancellation of this policy, whichever is earlier.
21. PolicyYear means a period of 12 consecutive months within the Policy
Period commencing from the Policy Anniversary/Commencement
Date.
22. PolicySchedule means Schedule attached to and forming part of this
Policy mentioning the details of the Policy Holder, Insured Persons, the
Sum Insured, the period and the limits to which benets under
the Policy are subject to, Premium Paid (including taxes), including any
annexures and/or endorsements, made to or on it from time to time,
and if more than one, then the latest in time.
23. Restored Sum Insured means the amount restored in accordance
with Section D.I.8 of this Policy
24. SinglePrivateRoommeans a single Hospital room with any rating
and of most economical category available at the time of hospitalization
with/without air-conditioning facility where a single patient is
accommodated and which has an attached toilet (lavatory and bath).
The room should have the provision for accommodating an attendant.
This excludes a suite or higher category.
25. Sum Insured means, subject to terms, conditions and exclusions of
this Policy, the amount representing Our maximum liability for any or all
claimsduringthePolicyPeriodspeciedinthePolicySchedule
separately in respect of that Insured Person.
i. In case where the Policy Period is 2/3 years, the Sum Insured
speciedonthePolicyisthelimitfortherstPolicyYear.These

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
limitswilllapseattheendoftherstyearandthefreshlimitsupto
the full Sum Insured as opted will be available for the second/third
year.
ii. In the event of a claim being admitted under this Policy, the Sum
Insured for the remaining Policy Period shall stand correspondingly
reduced by the amount of claim paid (including ’taxes’) or admitted
and shall be reckoned accordingly.
26. ThirdPartyAdministrator(TPA) means a company registered with
the Authority, and engaged by Us, for a fee or, by whatever name called
and as may be mentioned in the health services agreement, for
providing health services as mentioned under TPA Regulations.
27. We/Our/Us/Insurer means ManipalCigna Health Insurance Company
Limited
28. You/Your/Policy Holder means the person named in the Policy
Schedule as the policyholder and who has concluded this Policy with
Us.
C Benetscoveredunderthepolicy
C.I Basiccovers
C.I.1 In-patientHospitalization
We will cover Medical Expenses of an Insured Person in case of
Medically Necessary Hospitalization arising from a Disease/ Illness
or Injury provided such Medically Necessary Hospitalization is for
more than 24 consecutive hours provided that the admission date of
the Hospitalization due to Disease/ Illness or Injury is within the Policy
Year. We will pay Medical Expenses as shown in the Policy Schedule
for:
a. Reasonable and Customary Charges for Room Rent for
accommodation in Hospital room up to Category as specied in
the Policy Schedule.
b. Intensive Care Unit charges for accommodation in ICU ,
c. Operation theatre charges,
d. Fees of Medical Practitioner/ Surgeon ,
e. Anesthetist,
f. QualiedNurses,
g. Specialists,
h. Cost of diagnostic tests,
i. Medicines,
j. Drugs and consumables, blood, oxygen, surgical appliances and
prosthetic devices recommended by the attending Medical
Practitioner and that are used intra operatively during a Surgical
Procedure.
Room category coverage under each plan will be covered up to
SinglePrivateACRoomorasspeciedinthePolicySchedule,subject
to maximum of Sum Insured Opted. For ICU accommodation, we will
coveruptoSumInsuredoptedorasspeciedinthePolicySchedule.
If the Insured Person is admitted in a room category that is higher
than the one that is specied in the Policy Schedule, then the
Policyholder/Insured Person shall bear a ratable proportion of the total
Associated Medical Expenses (including surcharge or taxes thereon)
in the proportion of the difference between the room rent of the entitled
room category to the room rent actually incurred.
Under In-patient Hospitalization expenses, when availed under In-
patient care, we will cover the expenses towards articial life
maintenance, including life support machine use, even where such
treatment will not result in recovery or restoration of the previous state
of health under any circumstances unless in a vegetative state, as
certiedbythetreatingMedicalPractitioner.
The following procedures will be covered (wherever medically
indicated) either as In-patient or as part of Day Care Treatment in
a hospital up to the limit as per the plan and sum insured opted and as
speciedinthePolicyScheduleinaPolicyYear.:
a. Uterine Artery Embolization and HIFU (High intensity focused
ultrasound)
b. Balloon Sinuplasty
c. Deep Brain stimulation
d. Oral chemotherapy
e. Immunotherapy - Monoclonal Antibody to be given as injection
f. Intra vitreal injections
g. Robotic surgeries
h. Stereotactic radio surgeries
i. Bronchial Thermoplasty
j. Vaporization of the prostrate (Green laser treatment or holmium
laser treatment)
k. IONM - (Intra Operative Neuro Monitoring)
l. Stem cell therapy: Hematopoietic stem cells for bone marrow
transplant for hematological conditions to be covered.
Medical Expenses incurred towards Medically Necessary Treatment of
the Insured Person for In-patient Hospitalization due to a condition
caused by or associated with Human Immunodeciency Virus (HIV)
or HIV related Illnesses, including Acquired Immune Deciency
Syndrome (AIDS) or AIDS Related Complex (ARC) and/or any mutant
derivative or variations thereof, sexually transmitted diseases (STD), in
respect of an Insured Person, will be covered up to the Sum Insured
optedandasspecied in thePolicySchedulein a PolicyYear.The
necessity of the Hospitalization is to be certied by an authorized
Medical Practitioner.
Medical Expenses incurred towards Medically Necessary treatment
taken during In-patient Hospitalization of the Insured Person, arising
out of a condition caused by or associated to a Mental illness, or a
medical condition impacting mental health will be covered up to the
suminsuredoptedandasspeciedinthePolicyScheduleinaPolicy
Year. For the below mentioned ICD Codes, the Insured Person should
have been continuously covered under this Policy for at least 24
monthsbeforeavailingthisbenet.
ICD 10
CODES
DISEASES
F05 Delirium due to known physiological condition
F06 Other mental disorders due to known physiological
condition
F07 Personality and behavioural disorders due to known
physiological condition
F10 Alcohol related disorders
F20 Schizophrenia
F23 Brief psychotic disorders
F25 Schizoaffective disorders
F29 Unspeciedpsychosisnotduetoasubstanceorknown
physiological condition
F31 Bipolar disorder
F32 Depressive episode
F39 Unspeciedmood[affective]disorder
F40 Phobic Anxiety disorders
F41 Other Anxiety disorders
F42 Obsessive-compulsive disorder
F44 Dissociative and conversion disorders
F45 Somatoform disorders
F48 Other nonpsychotic mental disorders
F60 Specicpersonalitydisorders
F84 Pervasive developmental disorders
F90 Attention-decithyperactivitydisorders
F99 Mentaldisorder,nototherwisespecied
AllClaimsunderthisbenetcanbemadeasper theprocessdenedunder
Section G.I.4 and G.I.5.
C.I.2 Pre-hospitalization
We will, on a reimbursement basis cover Medical Expenses of an
Insured Person which are incurred due to a Disease/ Illness or Injury

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
that occurs during the Policy Year immediately prior to the Insured
Person’s date of Hospitalization up to the limits as specied in the
Policy Schedule, provided that a Claim has been admitted under
In-patientbenetunderSectionD.I.1andisrelatedtothesameillness/
condition.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5 and G.I.9.
C.I.3 Post-hospitalization
We will, on a reimbursement basis cover Medical Expenses of an
Insured Person which are incurred due to a Disease/ Illness or Injury
that occurs during the Policy Year immediately post discharge of the
InsuredPersonfromthe Hospital uptothelimits as speciedinthe
Policy Schedule, provided that a Claim has been admitted under
In-patientbenetunderSectionD.I.1andisrelatedtothesameillness/
condition.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5 and G.I.9.
C.I.4 DayCareTreatment
We will cover payment of Medical Expenses of an Insured Person in
case of Medically Necessary Day Care Treatment or Surgery that
requires less than 24 hours of Hospitalization due to advancement in
technology and which is undertaken in a Hospital/ Nursing Home/ Day
Care Centre on the recommendation of a Medical Practitioner, up to
theSumInsuredasspeciedinthePolicySchedule,providedthat:
a. The Day Care Treatment is Medically Necessary and follows the
written advice of a Medical Practitioner.
b. The Medical Expenses incurred are Reasonable and Customary
Charges for any procedure where such procedure is undertaken
by an Insured Person as Day Care Treatment.
c. We will not cover any OPD Treatment and Diagnostic Service
underthisbenet.
Coverage will also include pre-post hospitalization expenses as per the
limitsapplicableandspeciedunderthePlanopted.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.5 DomiciliaryHospitalization
We will cover Medical Expenses of an Insured Person, up to limits
speciedaspertheoptedplan,whicharetowardsaDisease/Illnessor
Injury which in the normal course would otherwise have been covered
for Hospitalization under the policy but is taken at home on the advice
of the attending Medical Practitioner, under the following circumstances:
i. The condition of the Insured Person does not allow a Hospital
transfer; or
ii. A Hospital bed was unavailable;
Provided that, the treatment of the Insured Person continues for at
least 3 days, in which case the reasonable cost of any Medically
Necessary treatment for the entire period shall be payable.
a) We will pay for Pre-hospitalization, Post-hospitalization Medical
Expensesupto30dayseach.
b) Restoration of Sum Insured shall not be available under this
benet
c) We shall not be liable under this Policy for any Claim in connection
with or in respect of the following:
i. Asthma, COPD, bronchitis, tonsillitis and upper and lower
respiratory tract infection including laryngitis and pharyngitis,
coughandcold,inuenza,
ii. Arthritis, gout and rheumatism including the rheumatism of
bones, joints and also rheumatic heart disease,
iii. Chronic nephritis and nephritic syndrome,
iv. All types of Diarrhea and dysenteries, including gastroenteritis,
v. Diabetes mellitus and Diabetes Insipidus,
vi. Epilepsy / Seizure disorder,
vii. Hypertension,
viii. Pyrexia of unknown origin.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5.
C.I.6 RoadAmbulance
We will provide for reimbursement of Reasonable and Customary
expenses up to Sum Insured as specied in the Policy Schedule
that are incurred towards road transportation of an Insured Person by a
registered Healthcare or Ambulance Service Provider to a nearest
Hospital for treatment of an Illness or Injury covered under the Policy in
case of an Emergency, necessitating the Insured Person’s admission
to the nearest Hospital. The necessity of use of an Ambulance must be
certiedbythetreatingMedicalPractitioner.
a. Reasonable and Customary expenses shall include:
(i) Costs towards transferring the Insured Person from one
Hospital to another Hospital or diagnostic centre for advanced
diagnostic treatment where such facility is not available at the
existing Hospital; or
(ii) When the Insured Person requires to be moved to a better
Hospital facility due to lack of super specialty treatment in the
existing Hospital.
b. Payment under this cover is subject to a claim being admissible
under Section D.I.1 ‘In-patient Hospitalization’, for the same
Illness/Injury;
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5.
C.I.7 DonorExpenses
We will cover In-patient Hospitalization Medical Expenses towards the
donorforharvestingtheorganuptotheSumInsuredasspeciedin
the Policy Schedule, subject to the below mentioned conditions:
a. The organ donor is any person in accordance with the
Transplantation of Human Organs Act 1994 (amended) and other
applicable laws and rules, provided that –
i. The organ donated is for the use of the Insured Person who
has been asked to undergo an organ transplant on Medical
Advice.
b. We have admitted a claim under Section D.I.1 – towards In-patient
Hospitalization
c. We will not cover expenses towards the Donor in respect of:
i. Any Pre or Post-hospitalization Medical Expenses,
ii. Cost towards donor screening,
iii. Cost associated to the acquisition of the organ,
iv. Any other medical treatment or complication in respect of the
donor, consequent to harvesting.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.8 RestorationofSumInsured
We will provide for a 100% restoration of the Sum Insured for any
number of times in a Policy Year whether the illness/condition is
unrelated or same, provided that:
a. The Sum Insured inclusive of earned Cumulative Bonus (if any) or
CumulativeBonusBooster(ifopted&earned)isinsufcientasa
result of previous claims in that Policy Year.
b. The Restored Sum Insured will be available only for claims made
by Insured Persons in respect of future claims that become
payable under Section D of the Policy and shall not apply to the
rstclaiminthePolicyYear.RestorationoftheSumInsuredwillonly
be provided for coverage under Section D.I.1 ‘In-patient
Hospitalization’, Section D.I.2 ‘Pre-Hospitalization’, Section D.I.3
‘Post-Hospitalization’, Section D.I.4 ‘Day Care Treatment’, Section
D.I.6 ‘Road Ambulance’, Section D.I.7 ‘Donor Expenses’, Section
D.I.9 ‘AYUSH Treatment (In-patient Hospitalization)’ Section D.IV.1
‘Non-Medical Items’.
c. The Restored Sum Insured will not be considered while calculating
the Cumulative Bonus/ Cumulative Bonus Booster.
d. Such restoration of Sum Insured will be available for any number
of times, during a Policy Year to each insured in case of an
Individual Policy and can be utilized by Insured Persons who stand
covered under the Policy before the Sum Insured was exhausted.
e. IfthePolicyisissuedonaoaterbasis,theRestoredSumInsured
willalsobeavailableonaoaterbasis.
f. If the Restored Sum Insured is not utilized in a Policy Year, it shall
not be carried forward to subsequent Policy Year.
g. For any single claim during a Policy Year the maximum Claim
amount payable shall be sum of:

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
i. The Sum Insured
ii. Cumulative Bonus (if earned) or Cumulative Bonus Booster (if
opted & earned)
iii. Restored Sum Insured
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.9 AYUSHTreatment(In-patientHospitalization)
We will pay the Medical Expenses incurred during the Policy Year,
up to the Sum Insured as specied in the Policy Schedule, of an
Insured Person in case of Medically Necessary Treatment taken during
In-patient Hospitalization for AYUSH Treatment for an Illness or Injury
that occurs during the Policy Year, provided that:
The Insured Person has undergone treatment in an AYUSH Hospital
where AYUSH Hospital is a healthcare facility wherein medical/
surgical/ para-surgical treatment procedures and interventions
are carried out by AYUSH Medical Practitioner(s) comprising any of the
following:
i) Central or State Government AYUSH Hospital; or
ii) Teaching hospitals attached to AYUSH College recognized by
Central Government / Central Council of Indian Medicine and
Central Council of Homeopathy; or
iii) AYUSH Hospital, standalone or co-located with In-patient
healthcare facility of any recognized system of medicine, registered
with the local authorities, wherever applicable, and is under the
supervisionofaqualiedregistered AYUSH Medical Practitioner
and must comply with all the following criterion:
a. HavingatleastveIn-patientbeds;
b. HavingqualiedAYUSHMedicalPractitionerinchargeround
the clock;
c. Having dedicated AYUSH therapy sections as required and/or
has equipped operation theatre where surgical procedures are
to be carried out;
d. Maintaining daily record of the patients and making them
accessible to the insurance company’s authorized
representative.
The following exclusions will be applicable in addition to the other
Policy exclusions:
Facilities and services availed for pleasure or rejuvenation or as
a preventive aid, like beauty treatments, Panchakarma, purication,
detoxicationandrejuvenation.
Allclaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.10 AirAmbulanceCover
We will reimburse the Reasonable and Customary expenses
incurred towards transportation of an Insured Person, to the
nearest Hospital or to move the Insured Person to and from
healthcare facilities within India, by an Air Ambulance, provided
that:
i. Air Ambulance is used in case of an Emergency life threatening
health condition of the Insured Person which requires immediate
and rapid ambulance transportation to the hospital or a medical
centre which ground transportation cannot provide;
ii. The Illness/ Injury, causing Emergency, is covered under the
Section D.I.1 In-patient Hospitalization;
iii. The transportation should be provided by medically equipped
aircraft which can provide medical care in ight and should
have medical equipment to monitor vitals and treat the Insured
Person suffering from an Illness/Injury such as but not limited
to ventilators, ECG’s, monitoring units, CPR equipment and
stretchers;
iv. Restoration of Sum Insured shall not be available under this
benet.
v. Air Ambulance service is offered by a Registered Ambulance
service provider;
vi. ThetreatingMedicalPractitionercertiesinwritingthattheseverity
and nature of the Insured Person’s Illness/Injury warrants the
Insured Person’s requirement for Air Ambulance;
vii. Payment under this cover is subject to a claim being admissible
under Section D.I.1 ‘In-patient Hospitalization’ or under Section
D.I.4 ‘Day Care Treatment’, for the same Illness/Injury;
Benet under this cover is payable Up to the limits as specied in
the Policy Schedule subject to maximum up to `10 Lacs in a
policy year and this is over and above the Sum Insured.
What is not covered: Expenses incurred in return transportation to
Insured Person’s home by air ambulance is excluded.
All Claims under this benet can be made as per the process
denedunderSectionG.I.5.
C.I.11 BariatricSurgeryCover
We will cover the Medical Expenses incurred towards Medically
Necessary Hospitalization of the Insured Person for Bariatric
Surgery and its complications, up to Sum Insured and as specied
in Policy Schedule subject to maximum of `5 Lacs.
The cover is available subject to below conditions:
i. SurgeryisMedically Necessary andiscertiedby anauthorized
Medical Practitioner;
ii. Hospitalization is within the Policy Year.
iii. TheInsuredPersonsatisesfollowingcriteriaasdevisedbyNIH
(National Institute of Health):
a. The BMI should be greater than 37.5 without any co-morbidity;
or greater than 32 with co-morbidity and
b. Is unable to lose weight through traditional methods like diet
and exercise.
iv. This cover is available after a Waiting Period of 36 months from the
inception of this Policy with Us, with respect to the Insured Person.
v. Restoration of Sum Insured shall not be available under this
benet
vi. ExclusionE.I.6shallnotapplyuptotheextentofthisbenet
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5
C.I.12 OutpatientExpenses
We will cover the Reasonable and Customary Charges for below
mentioned expenses incurred by the Insured Person as an Outpatient
when treatment is taken from a Network Medical Practitioner to the
extentoftheOutpatientSumInsuredoptedandasspeciedinPolicy
Scheduleforthisbenet.
i. Consultation and Diagnostic tests including Dental and Vision
consultations and diagnostics, wherever prescribed by the Network
MedicalPractitioner,uptotheOutpatientSumInsuredasspecied
in the Policy Schedule.
ii. Expenses incurred on drugs and medicines prescribed by the
Network Medical Practitioner up to 20% of the Outpatient Sum
InsuredandasspeciedinthePolicySchedule.
Overall payout in a Policy Year should not exceed 100% of the
applicable Outpatient Sum Insured.
Any medical aids such as spectacles and contact lenses, hearing aids,
crutches, wheel chair, walker, walking stick, lumbo-sacral belt shall not
becoveredunderthisbenet.Weshallnotcoveranytreatmentand/or
procedureunderthisbenetrelatedtoDentalandVision
Any unutilized amount under this benet shall not be carried
forward to subsequent Policy Year.
This benet shall be available only on Cashless basis from the
MCHI Network. All Diagnostics and Pharmacy requirements would
need to be prescribed by the Network Medical Practitioner in order
tomakethemeligibleunderthisbenet.
Restoration of Sum Insured shall not be available under this
benet.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4. and G.I.12
C.I.13 DailyCashforSharedAccommodation
WewillpayadailycashamountasspeciedinthePolicySchedule
for the Insured Person for each continuous and completed period
of 24 hours of Hospitalization provided that,
a. We have accepted claim under Section D.I.1 In-patient
Hospitalization during the Policy Year
b. The Insured Person has occupied a shared room accommodation
during such Hospitalization
c. The Insured Person has been admitted in a Hospital for a minimum
period of 48 hours continuously.
What is not covered:

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
This benet will not be payable if the Insured Person stays in an
Intensive Care Unit or High Dependency Units / wards.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5
C.II Valueaddedcovers
C.II.1 HealthCheckUp
(a) If the Insured Person, covered as adult (excluding dependent
children in oater Policy) and has completed 18 years of age,
the Insured Person may avail a comprehensive health check-up
with Our Network Provider as per the eligibility details mentioned in
the table below.
(b) In case of individual policy where more than 1 member are covered
under the same Individual Policy, upon attainment of 18 years of
age, the Insured member shall be eligible for health check-up with
Our Network Provider as per the eligibility details mentioned in the
table below.
(c) Health Check Ups will be arranged by Us and conducted at Our
Network Providers. Alternatively, the Insured member may choose
to undergo Health Check Ups as per Insured member’s choice on
Cashless basis with Our Network Provider, subject to the maximum
limitsasspeciedagainsttheapplicableSumInsured.
(d) This benet is available once in a policy year including the rst
policy year. And all the tests must have been done on the same
date.
(e) Original Copies of all reports will be provided to You.
(f) We shall cover Health Check Up only on cashless basis.
(g) All eligible Insured members under the Policy shall either follow
“Basis A” or “Basis B” while availing Health Check Up cover, within
MCHI Network.
HealthCheckUp
Package
Sum
Insured
Age
group
Basis–A Basis-B
Listoftests–Cashless
Limitsfor
testsof
Insured
member’s
choiceon
Cashless
basis
Compulsory
Tests
Optional
Tests
(Anyone)
1
`3
Lacs,
`4
Lacs,
`5 Lacs
Up
to40
Years
CBC-ESR,
FBS, Lipid
Prole,Sr.
Creatinine
B1 - Heart
monitoring
– ECG or
B2 - Liver
screening
- SGOT
and SGPT
`1,000
per adult
Insured
member
Above
40
years
CBC-ESR,
FBS, Lipid
Prole,Sr.
Creatinine
B1 - Heart
monitoring
– ECG or
B2 - Liver
screening
- SGOT
and SGPT
or
B3 -
Thyroid
Screening
- Thyroid
prole
B4 -
Diabetes
screening
- HbA1c
2
`7.5
Lacs,
`10
Lacs,
Up
to40
Years
ECG,FBS,LipidProle,
Sr. Creatinine, CBC-ESR,
SGOT, SGPT, GGT, TSH,
USG - Abdomen & pelvis
`2,500
per adult
Insured
member
Above
40
years
ECG,FBS,LipidProle,
Sr. Creatinine, CBC-ESR,
SGOT, SGPT, GGT, TSH,
HbA1c, USG Abdomen &
Pelvis, PSA (for Males),
Mammogram/ PAP Smear
(for females)
3
> `10
Lacs
Up
to40
Years
FBS,KidneyProle,ECG,
CBC-ESR,LipidProle,
LiverProle,Thyroid
Prole,2D-Echo,USGAb-
domen & Pelvis, Vitamin
D3, Vitamin B12
`5,000
per adult
Insured
member
Above
40
years
FBS, ECG, HbA1C,
KidneyProle,CBC-ESR,
LipidProle,LiverProle,
ThyroidProle,2D-Echo,
PSA (for Males)/ Mam-
mogram/ PAP Smear (for
females), USG Abdomen
& Pelvis, Vitamin D3,
Vitamin B12,
Full explanation of Tests is provided here: FBS – Fasting Blood
Sugar, ECG – Electrocardiogram, CBC-ESR – Complete Blood Count-
Erythrocyte Sedimentation Rate, Sr. Creatinine – Serum Creatinine,
HbA1c – Glycosylated Hemoglobin, SGOT – Serum Glutamate
oxaloacetate transaminase, SGPT – Serum Glutamate Pyruvate
Transaminase, GGT – Gamma Glutamyl Transferase, TMT – Tread
Mill Test, PSA – Prostate Specic Antigen, USG – Ultrasound
Sonography, TSH – Thyroid Stimulating Hormone, CBC – Complete
Blood Count
(h) This cover is available up to the limits as per Sum Insured opted
andasspeciedinthePolicySchedule.
(i) ThisbenetshallbeoverandabovetheSumInsured.
(j) Restoration of Sum Insured shall not be available under this
benet
(k) All Claims under this benet can be made as per the process
denedunderSectionG.I.14&G.I.5
C.II.2 DomesticSecondOpinion
You may choose to secure a second opinion from Our Network of
Medical Practitioners in India, if an Insured Person is diagnosed
with/ advised a treatment listed and dened under Critical Illness
during the Policy Year. The expert opinion would be directly sent to the
Insured Person.
You understand and agree that You can exercise the option to secure
an expert opinion, provided:
(a) We have received a request from You to exercise this option.
(b) That the expert opinion will be based only on the information and
documentation provided by the Insured Person that will be shared
with the Medical Practitioner
(c) This benet is only a value added service provided by Us and
does not deem to substitute the Insured Person’s visit or
consultation to an independent Medical Practitioner.
(d) The Insured Person is free to choose whether or not to obtain the
expert opinion, and if obtained then whether or not to act on it.
(e) We shall not, in any event be responsible for any actual or alleged
errors or representations made by any Medical Practitioner or in
any expert opinion or for any consequence of actions taken or not
taken in reliance thereon.
(f) The expert opinion under this Policy shall be limited to covered
Critical Illnesses and not be valid for any medico legal purposes.
(g) We do not assume any liability towards any loss or damage arising
out of or in relation to any opinion, advice, prescription, actual
or alleged errors, omissions and representations made by the
Medical Practitioner.
(h) This benet can be availed by each Insured Person only once
during a Policy Year for one Critical Illness. However, one can avail
thisbenetformultiplecriticalillnessesinayear.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
(i) AnyclaimunderthisbenetwillnotimpacttheSumInsuredand/or
Cumulative Bonus or Cumulative Bonus Booster.
(j) For the purpose of this benet covered Critical Illnesses shall
include –
1. CancerofSpeciedSeverity
A malignant tumor characterized by the uncontrolled growth & spread
of malignant cells with invasion & destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy.
The term cancer includes leukemia, lymphoma and sarcoma.
The following are excluded –
i. All tumors which are histologically described as carcinoma in
situ, benign, pre-malignant, borderline malignant, low malignant
potential, neoplasm of unknown behavior, or non-invasive,
including but not limited to: Carcinoma in situ of breasts, Cervical
dysplasia CIN-1, CIN -2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. All tumors of the prostate unless histologically classied as
having a Gleason score greater than 6 or having progressed to at least
clinicalTNMclassicationT2N0M0
v. All Thyroid cancers histologically classied as T1N0M0 (TNM
Classication)orbelow;
vi. Chronic lymphocytic leukemia less than RAI stage 3
vii. Non-invasive papillary cancer of the bladder histologically
describedasTaN0M0orofalesserclassication,
viii.All Gastro-Intestinal Stromal Tumors histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of
lessthanorequalto5/50HPFs;
ix. All tumors in the presence of HIV infection.
2. MyocardialInfarction(FirstHeartAttackofSpecicSeverity)
I The rst occurrence of heart attack or myocardial infarction, which
means the death of a portion of the heart muscle as a result of
inadequate blood supply to the relevant area. The diagnosis for this will
be evidenced by all of the following criteria:
i. a history of typical clinical symptoms consistent with the diagnosis
of Acute Myocardial Infarction (for e.g. typical chest pain)
ii. new characteristic electrocardiogram changes
iii. elevationofinfarctionspecicenzymes,Troponinsorotherspecic
biochemical markers.
II The following are excluded:
1. Other acute Coronary Syndromes
2. Any type of angina pectoris.
3. A rise in cardiac biomarkers or Troponin T or I in absence of overt
ischemic heart disease OR following an intra-arterial cardiac
procedure.
3. OpenChestCABG
I The actual undergoing of heart surgery to correct blockage or
narrowing in one or more coronary artery(s), by coronary artery bypass
grafting done via a sternotomy (cutting through the breast bone) or
minimally invasive keyhole coronary artery bypass procedures. The
diagnosis must be supported by a coronary angiography and the
realizationofsurgeryhastobeconrmedbyacardiologist.
II The following are excluded:
a. Angioplasty and/or any other intra-arterial procedures
4. OpenHeartReplacementorRepairofHeartValves
The actual undergoing of open-heart valve surgery is to replace or
repair one or more heart valves, as a consequence of defects in,
abnormalities of, or disease-affected cardiac valve (s). The diagnosis
of the valve abnormality must be supported by an echocardiography
and the realization of surgery has to be conrmed by a specialist
medical practitioner. Catheter based techniques including but not
limited to, balloon valvotomy/valvuloplasty are excluded.
5. ComaofSpeciedSeverity
1. A state of unconsciousness with no reaction or response to external
stimuli or internal needs.
This diagnosis must be supported by evidence of all of the following:
i. no response to external stimuli continuously for at least 96 hours;
ii. life support measures are necessary to sustain life; and
iii. permanentneurologicaldecitwhichmustbeassessedatleast30
days after the onset of the coma.
2. The condition has to be conrmed by a specialist medical
practitioner. Coma resulting directly from alcohol or drug abuse is
excluded.
6. KidneyFailureRequiringRegularDialysis
End stage renal disease presenting as chronic irreversible failure of
both kidneys to function, as a result of which either regular renal dialysis
(hemodialysis or peritoneal dialysis) is instituted or renal transplantation
iscarriedout.Diagnosishastobeconrmedbyaspecialistmedical
practitioner.
7. StrokeResultinginPermanentSymptoms
Any cerebrovascular incident producing permanent neurological
sequelae. This includes infarction of brain tissue, thrombosis in an
intracranial vessel, hemorrhage and embolization from an extra cranial
source. Diagnosis has to be conrmed by a specialist medical
practitioner and evidenced by typical clinical symptoms as well as
typicalndingsinCTscanorMRIofthebrain.Evidenceofpermanent
neurologicaldecitlastingforatleast3monthshastobeproduced.
The following are excluded:
1. Transient ischemic attacks (TIA)
2. Traumatic injury of the brain
3. Vascular disease affecting only the eye or optic nerve or vestibular
functions.
8. MajorOrgan/BoneMarrowTransplant
The actual undergoing of a transplant of:
1. One of the following human organs: heart, lung, liver, kidney,
pancreas, that resulted from irreversible end-stage failure of the
relevant organ, or
2. Human bone marrow using hematopoietic stem cells. The
undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
i. Other stem-cell transplants
ii. Where only islets of langerhans are transplanted
9. PermanentParalysisofLimbs
Total and irreversible loss of use of two or more limbs as a result of
injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be permanent
with no hope of recovery and must be present for more than 3 months.
10. MotorNeuronDiseasewithPermanentSymptoms
Motor neuron disease diagnosed by a specialist medical practitioner
as spinal muscular atrophy, progressive bulbar palsy, amyotrophic
lateral sclerosis or primary lateral sclerosis. There must be progressive
degeneration of corticospinal tracts and anterior horn cells or bulbar
efferent neurons. There must be current signicant and permanent
functional neurological impairment with objective evidence of motor
dysfunction that has persisted for a continuous period of at least 3
months.
11. MultipleSclerosiswithPersistingSymptoms
I. TheunequivocaldiagnosisofDeniteMultipleSclerosisconrmedand
evidenced by all of the following:
i. investigationsincluding typicalMRIndings,which unequivocally
conrmthediagnosistobemultiplesclerosis;
ii. there must be current clinical impairment of motor or sensory
function, which must have persisted for a continuous period of at
least 6 months, and
II. Other causes of neurological damage such as SLE and HIV are
excluded.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
12. Primary(Idiopathic)PulmonaryHypertension
I. An unequivocal diagnosis of Primary (Idiopathic) Pulmonary
Hypertension by a Cardiologist or specialist in respiratory medicine
with evidence of right ventricular enlargement and the pulmonary
arterypressureabove30mmofHgonCardiacCauterization.
There must be permanent irreversible physical impairment to the
degree of at least Class IV of the New York Heart Association
Classicationofcardiacimpairment.
II. TheNYHAClassicationofCardiacImpairmentareasfollows:
i. Class III: Marked limitation of physical activity. Comfortable at rest,
but less than ordinary activity causes symptoms.
ii. Class IV: Unable to engage in any physical activity without
discomfort. Symptoms may be present even at rest.
III. Pulmonary hypertension associated with lung disease, chronic
hypoventilation, pulmonary thromboembolic disease, drugs and toxins,
diseases of the left side of the heart, congenital heart disease and any
secondarycausearespecicallyexcluded.
13. AortaGraftSurgery
The actual undergoing of major Surgery to repair or correct aneurysm,
narrowing, obstruction or dissection of the Aorta through surgical
opening of the chest or abdomen.
Forthepurposeofthisbenet,Aortameansthethoracicandabdominal
aorta but not its branches.
You understand and agree that We will not cover:
a. Surgery performed using only minimally invasive or intra-arterial
techniques.
b. Angioplasty and all other intra-arterial, catheter based techniques,
"keyhole" or laser procedures.
c. Congenital narrowing of the aorta and traumatic injury of the aorta
arespecicallyexcluded.
14. Deafness
Total and irreversible Loss of hearing in both ears as a result of Illness
or accident.
This diagnosis must be supported by pure tone audiogram test and
certiedbyanEar,NoseandThroat(ENT)specialist.Totalmeans“the
lossofhearingtotheextentthatthelossisgreaterthan90decibels
across all frequencies of hearing” in both ears.
15. Blindness
I. Total, permanent and irreversible loss of all vision in both eyes as a
result of illness or accident.
II. The Blindness is evidenced by:
i. correctedvisualacuitybeing3/60orlessinbotheyesor;
ii. theeldofvisionbeinglessthan10degreesinbotheyes.
III. The diagnosis of blindness must be conrmed and must not be
correctable by aids or surgical procedure.
16. AplasticAnemia
Chronic persistent bone marrow failure which results in anemia,
neutropenia and thrombocytopenia requiring treatment with at least
one of the following:
a. Blood product transfusion;
b. Marrow stimulating agents;
c. Immunosuppressive agents; or
d. Bone marrow transplantation.
The diagnosis must be conrmed by a hematologist Medical
Practitioner using relevant laboratory investigations including Bone
MarrowBiopsyresultinginbone marrowcellularityoflessthan 25%
which is evidenced by any two of the following:
a. Absoluteneutrophilcountoflessthan500/mm³orless;
b. Plateletscountlessthan20,000/mm³orless;
c. Reticulocytecountoflessthan20,000/mm³orless.
We will not cover temporary or reversible Aplastic Anemia under this
Section.
17. CoronaryArteryDisease
Therstevidenceofnarrowingofthelumenofatleastonecoronary
arterybyaminimumof75%andoftwoothersbyaminimumof60%,
regardless of whether or not any form of coronary artery Surgery
has been performed. Coronary arteries herein refer to left main stem,
leftanteriordescendingcircumexandrightcoronaryarteryandnotits
branches which is evidenced by the following
a. evidence of ischemia on Stress ECG (NYHA Class III symptoms)
b. coronary arteriography (Hearth Cath)
18. EndStageLungFailure
End Stage Lung Disease, causing chronic respiratory failure, as
conrmedandevidencedbyallofthefollowing:
i. FEV1 test results consistently less than 1 liter measured on 3
occasions 3 months apart; and
ii. Requiring continuous and permanent supplementary oxygen
therapy for hypoxemia; and
iii. Arterial blood gas analysis with partial oxygen pressure of 55mmHg
or less (PaO2 < 55 mm Hg); and
iv. Dyspnea at rest.
19. EndStageLiverFailure
Permanent and irreversible failure of liver function that has resulted in
all three of the following:
a. Permanent jaundice;
b. Ascites; and
c. Hepatic Encephalopathy.
Liver failure secondary to drug or alcohol abuse is excluded.
20. ThirdDegreeBurns
There must be third-degree burns with scarring that cover at least
20%ofthebody’ssurfacearea.Thediagnosismustconrmthetotal
area involved using standardized, clinically accepted, body surface
areachartscovering20%ofthebodysurfacearea.
21. FulminantHepatitis
A sub-massive to massive necrosis of the liver by the Hepatitis virus,
leading precipitously to liver failure. This diagnosis must be supported
by all of the following:
a. Rapid decreasing of liver size;
b. Necrosis involving entire lobules, leaving only a collapsed reticular
framework;
c. Rapid deterioration of liver function tests;
d. Deepening jaundice; and
e. Hepatic encephalopathy.
Acute Hepatitis infection or carrier status alone does not meet the
diagnostic criteria.
22. Alzheimer’sDisease
Alzheimer’s disease is a progressive degenerative Illness of the
brain, characterized by diffuse atrophy throughout the cerebral cortex
with distinctive histopathological changes. Deterioration or loss of
intellectualcapacity,asconrmedbyclinicalevaluationandimaging
tests, arising from Alzheimer’s disease, resulting in progressive
signicant reduction in mental and social functioning, requiring the
continuous supervision of the Insured Person. The diagnosis must be
supported by the clinical conrmation of a Neurologist Medical
Practitioner and supported by Our appointed Medical Practitioner.
The following conditions are however not covered:
a. non-organic diseases;
b. alcohol related brain damage; and
c. any other type of irreversible organic disorder/dementia.
23. BacterialMeningitis
Bacterialinfectionresultinginsevereinammationofthemembranes
of the brain or spinal cord resulting in signicant, irreversible and
permanentneurologicaldecit.Theneurologicaldecitmustpersistfor
atleast6weeks.Thisdiagnosismustbeconrmedby:
a. Thepresenceofbacterialinfectionincerebrospinaluidbylumbar
puncture; and
b. A consultant neurologist Medical Practitioner.
We will not cover Bacterial Meningitis in the presence of HIV infection

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
under this Section.
24. BenignBrainTumor
a. Benignbraintumorisdenedasalifethreatening,non-cancerous
tumor in the brain, cranial nerves or meninges within the skull. The
presenceoftheunderlyingtumormustbeconrmedbyimaging
studies such as CT scan or MRI.
b. This brain tumor must result in at least one of the following and
mustbeconrmedbytherelevantmedicalspecialist.
i. Permanent Neurological decit with persisting clinical
symptoms for a continuous period of at least 90consecutive
days or
ii. Undergone surgical resection or radiation therapy to treat the
brain tumor.
The following conditions are however not covered by Us:
a. cysts;
b. granulomas;
c. malformations in the arteries or veins of the brain;
d. hematoma;
e. Abscesses
f. Pituitary Tumors
g. tumors of skull bones and
h. tumors of the spinal cord
25. ApallicSyndrome
Universal necrosis of the brain cortex with the brainstem remaining
intact. The diagnosis must be conrmed by a Neurologist Medical
Practitioner acceptable to Us and the condition must be documented
by such Medical Practitioner for at least one month.
26. Parkinson’sDisease
The unequivocal diagnosis of progressive, degenerative idiopathic
Parkinson’s disease by a Neurologist Medical Practitioner acceptable
to Us.
The diagnosis must be supported by all of the following conditions:
a. the disease cannot be controlled with medication;
b. signs of progressive impairment; and
c. inability of the Insured Person to perform at least 3 of the 6
activities of daily living as listed below (either with or without the use
of mechanical equipment, special devices or other aids and
adaptations in use for disabled persons) for a continuous period of
at least 6 months:
Activities of daily living:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the shower) or wash satisfactorily by other means
and maintain an adequate level of cleanliness and personal
hygiene;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garmentsand,asappropriate,anybraces,articiallimbsorother
surgical appliances;
iii. Transferring: The ability to move from a lying position in a bed to a
sitting position in an upright chair or wheel chair and vice versa;
iv. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of
personal hygiene;
v. Feeding: the ability to feed oneself, food from a plate or bowl to the
mouth once food has been prepared and made available.
vi. Mobility: The ability to move indoors from room to room on level
surfaces at the normal place of residence.
We will not cover Parkinson’s disease secondary to drug and/or alcohol
abuse under this Section.
27. MedullaryCysticDisease
A progressive hereditary disease of the kidneys characterised by the
presence of cysts in the medulla, tubular atrophy and interstitial
brosiswiththeclinicalmanifestationsofanaemia,polyuriaandrenal
loss of sodium, progressing to chronic renal failure. The diagnosis
must be supported by renal biopsy.
28. MuscularDystrophy
A group of hereditary degenerative diseases of muscle characterized
by progressive and permanent weakness and atrophy of certain
muscle groups. The diagnosis of muscular dystrophy must be
unequivocal and made by a Neurologist Medical Practitioner acceptable
toUs,withconrmationofatleast3ofthefollowing4conditions:
a. Family history of muscular dystrophy;
b. Clinical presentation including absence of sensory disturbance,
normalcerebrospinaluidandmildtendonreexreduction;
c. Characteristic electromyogram;
d. Clinicalsuspicionconrmedbymusclebiopsy.
The condition must result in the inability of the Insured Person to
perform at least 3 of the 6 activities of daily living as listed below (either
with or without the use of mechanical equipment, special devices or
other aids and adaptations in use for disabled persons) for a continuous
period of at least 6 months:
Activities of daily living:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the shower) or wash satisfactorily by other means
and maintain an adequate level of cleanliness and personal
hygiene;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garmentsand,asappropriate,anybraces,articiallimbsorother
surgical appliances;
iii. Transferring: The ability to move from a lying position in a bed to a
sitting position in an upright chair or wheel chair and vice versa;
iv. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of
personal hygiene;
v. Feeding: the ability to feed oneself, food from a plate or bowl to the
mouth once food has been prepared and made available;
vi. Mobility: The ability to move indoors from room to room on level
surfaces at the normal place of residence.
29. LossofSpeech
a. Total and irrecoverable loss of the ability to speak as a result
of injury or disease to the vocal cords. The inability to speak must
be established for a continuous period of 12 months. This diagnosis
must be supported by medical evidence furnished by an Ear,
Nose, Throat (ENT) specialist.
b. All psychiatric related causes are excluded.
30. SystemicLupusErythematous
A multi-system, multifactorial, autoimmune disorder characterized
by the development of auto-antibodies directed against various self-
antigens. Only those forms of systemic lupus erythematous which
involve the kidneys (Class III to Class V lupus nephritis, established by
renal biopsy, and in accordance with the World Health Organization
(WHO) classication) will be covered by Us under this Section. The
naldiagnosismustbeconrmedbyaregisteredMedicalPractitioner
specializing in Rheumatology and Immunology acceptable to Us. Other
forms of systemic lupus erythematous, discoid lupus and those forms
with only hematological and joint involvement are however not covered:
TheWHOlupusclassicationisasfollows:
• Class I: Minimal change – Negative, normal urine.
• Class II: Mesangial – Moderate proteinuria, active sediment.
• Class III: Focal Segmental – Proteinuria, active sediment.
• Class IV: Diffuse – Acute nephritis with active sediment and/or
nephritic syndrome.
• Class V: Membranous – Nephrotic Syndrome or severe proteinuria.
31. LossofLimbs
a. The physical separation of two or more limbs, at or above the wrist or
ankle level limbs as a result of injury or disease. This will include
medically necessary amputation necessitated by injury or disease.
The separation has to be permanent without any chance of surgical
correction. Loss of Limbs resulting directly or indirectly from self-
inictedinjury,alcoholordrugabuseisexcluded.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
32. MajorHeadTrauma
a. AccidentalheadinjuryresultinginpermanentNeurologicaldecit
to be assessed no sooner than 3 months from the date of the
accident. This diagnosis must be supported by unequivocal
ndings on Magnetic Resonance Imaging, Computerized
Tomography, or other reliable imaging techniques. The accident
must be caused solely and directly by accidental, violent, external
and visible means and independently of all other causes.
b. The Accidental Head injury must result in an inability to perform
at least three (3) of the following Activities of Daily Living either
with or without the use of mechanical equipment, special devices
or other aids and adaptations in use for disabled persons. For the
purposeofthisbenet,theword“permanent”shallmeanbeyond
the scope of recovery with current medical knowledge and
technology.
c. The Activities of Daily Living are:
i. Washing: the ability to wash in the bath or shower (including
getting into and out of the bath or shower) or wash satisfactorily
by other means;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garments and, as appropriate, any braces, articial limbs or
other surgical appliances;
iii. Transferring: the ability to move from a bed to an upright chair
or wheelchair and vice versa;
iv. Mobility: the ability to move indoors from room to room on level
surfaces;
v. Toileting: the ability to use the lavatory or otherwise manage
bowel and bladder functions so as to maintain a satisfactory
level of personal hygiene;
vi. Feeding: the ability to feed oneself once food has been
prepared and made available.
d. The following are excluded:
a) Spinal cord injury
33. BrainSurgery
The actual undergoing of surgery to the brain, under general
anesthesia, during which a Craniotomy is performed. Burr hole and
brain surgery as a result of an accident is excluded. The procedure
mustbeconsiderednecessarybyaqualiedspecialistandthebenet
shall only be payable once corrective surgery has been carried out.
34. Cardiomyopathy
The unequivocal diagnosis by a consultant cardiologist of
Cardiomyopathy causing impaired ventricular function suspected by
ECGabnormalitiesandconrmedbycardiacechoofvariableetiology
and resulting in permanent physical impairments to the degree of at
leastClassIV oftheNew YorkAssociation(NYHA) Classicationof
cardiac impairment.
The NYHA Classication of Cardiac Impairment (Source: “Current
Medical Diagnosis and Treatment – 39th Edition”):
a. Class I: No limitation of physical activity. Ordinary physical activity
does not cause undue fatigue, dyspnoea, or angina pain.
b. Class II: Slight limitation of physical activity. Ordinary physical
activity results in symptoms.
c. Class III: Marked limitation of physical activity. Comfortable at rest,
but less than ordinary activity causes symptoms.
d. Class IV: Unable to engage in any physical activity without
discomfort. Symptoms may be present even at rest.
We will not cover Cardiomyopathy related to alcohol abuse under this
Section.
35. Creutzfeldt-JacobDisease(CJD)
A Diagnosis of Creutzfeldt-Jakob disease must be made by a Specialist
Medical Practitioner (Neurologist). There must be permanent clinical
loss of the ability in mental and social functioning for a minimum period
of30daystotheextentthatpermanentsupervisionorassistancebya
third party is required.
Socialfunctioningisdenedastheabilityoftheindividualtointeractin
the normal or usual way in society.
Mental functioning would mean functions /processes which we can do
with our minds.
36. TerminalIllness
An Insured Person shall be regarded as terminally ill only if he/ she
is diagnosed as suffering from a condition which, in the opinion of two
appropriate independent Medical Practitioners, is highly likely to lead
to death within 12 months from the date of the diagnosis and the
Insured Person is not receiving any active treatment for the terminal
illness, other than that of the pain relief. The terminal illness must
bediagnosedandconrmedbyMedicalPractitionersregisteredwith
the Indian Medical Association and approved by Us.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.13.
C.II.3 Tele-Consultation
Insured Person may avail tele-consultations with our Medical
Practitioner(s) through our network in India. These consultations would
be available through tele/chat mode.
Any claim under this benet will not impact theSum Insured and/or
Cumulative Bonus or Cumulative Bonus Booster (if opted).
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.14
C.II.4 CumulativeBonus
a) On Sum Insured
WewillincreaseYourSumInsuredby25%asspeciedunderPolicy
Schedule at the end of the Policy Year if the Policy is renewed with Us
without any break:
a) No Cumulative Bonus will be added if the Policy is not renewed
with Us by the end of the Grace Period.
b) The Cumulative Bonus will not be accumulated in excess of
200%oftheSumInsuredunderthecurrentPolicywithUsunder
any circumstances.
c) Any Cumulative Bonus that has accrued for a Policy Year will be
credited at the end of that Policy Year if the policy is renewed with
us within grace period and will be available for any claims made in
the subsequent Policy Year.
d) Merging of policies: If the Insured Persons in the expiring Policy
are covered under multiple policies and such expiring Policy has
been Renewed with Us on a Family Floater basis then the
Cumulative Bonus to be carried forward for credit in such Renewed
Policy shall be the lowest percentage of Cumulative Bonus
applicable on the lowest Sum Insured of the last policy year
amongst all the expiring polices being merged.
e) Splitting of policies: If the Insured Persons in the expiring Policy
are covered on a Family Floater basis and such Insured Persons
Renew their expiring Policy with Us by splitting the Sum Insured
in to two or more Family Floater/Individual policies then the
Cumulative Bonus shall be apportioned to such Renewed Policies
in the proportion of the Sum Insured of each Renewed Policy.
f) Reduction in Sum Insured: If the Sum Insured has been reduced at
the time of Renewal, the applicable Cumulative Bonus shall be
calculated on the revised Sum Insured on pro-rata basis.
g) Increase in Sum Insured: If the Sum Insured under the Policy has
been increased at the time of Renewal, the Cumulative Bonus
shall be calculated on the Sum Insured of the last completed
Policy Year.
h) Cumulative bonus shall not be available for claims made under
Value added cover (Section D.II) and also for D.III.1.i
Maternity & New Born Hospitalization Expenses, D.III.3.i Maternity
& New Born Hospitalization Expenses, D.III.1.iii Health Maintenance
Benet,D.I.10AirAmbulanceCover,D.I.12OutpatientExpenses,
D.I.13 Daily Cash for Shared Accommodation and D.IV.3 Infertility
Treatment.
i) This clause does not alter Our right to decline a Renewal or
cancellation of the Policy for reasons as mentioned under Section
F.I.6
C.II.5 SwitchOffBenet
IntheeventofyourtraveloutsideIndiaaftertherstpolicyyear,you
may switch off your insurance cover for a maximum continuous period
of30daysinapolicyyearandearnapremiumdiscountintheform
of pro-rated premium, based on the total number of days up to which
the cover has been switched off. Such pro-rated premium can be
utilized in the form of premium discount at the time of policy renewal.
When the insurance cover is in Switch Off mode, only the following
cover(s) if opted in the policy, shall remain active:

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
I. Section D.IV.4 Personal Accident Cover and
II. Section D.III.4.ii Worldwide Emergency Hospitalization with
Outpatient Cover under Freedom optional package
III. Section D.IV.6 Critical Illness Add On Cover
a. Premium discount shall be calculated on a pro-rata basis the
number of days the policy has been switched off on a per day
basis and this discount shall be adjusted in the renewal premium
falling due immediately after the expiring Policy Period.
b. In a Floater Policy, Switch Off Benet can be availed only if all
the Insured Persons travel outside India. However, in case of
an Multi-Individual Policy if any one or more Insured Person(s)
travel outside India, you can avail this benet and the premium
discount shall be calculated based on the applicable premium for
that/those particular individual(s).
c. ThisbenetshallnotbeavailableintherstPolicyYear.
d. This benet cannot be availed in the last 90 days of the Policy
Year.
e. During the Switch-off period, Your cover will be limited only
to Section D.IV.4 Personal Accident, Section D.III.4.ii
Worldwide Emergency Hospitalization with Outpatient Cover and
Section D.IV.6 Critical Illness Add-on, if opted. Any claim under
the oater policy, arising during the switch off period other than
claim under Section D.IV.4 Personal Accident Cover, Section
D.III.4.ii Worldwide Emergency Hospitalization with Outpatient
Cover and Section D.IV.6 Critical Illness Add-on, shall not be
payable. In case of Multi-Individual policies where members are
covered on individual basis, the switch off period shall apply only to
the respective member for which the request to switch off the
coverage is placed with the Insurer. The coverage shall start once
the cover is switched on either upon the expiry of the Switch Off
periodor30daysfromtheSwitchOffdate,whicheverisearlier.
f. The date of travel to abroad for all the Insured Members should be
sameincaseofaoaterpolicyinordertobeeligibletoutilizethis
cover.
g. InaFloaterPolicy,SwitchOffBenetcanbeavailedonlyifallthe
Insured Persons travel outside India at the same time. The date of
travel to abroad and return to India for all the Insured Members
should be same to be eligible to utilize this cover.
h. In case of a Multi-Individual Policy, You can Switch Off the Policy
for one or more members provided that the date of travel to abroad
and return to India for those Insured Members is same to be
eligible to utilize this cover.
i. ThisbenetcanbeutilizedonlyonceinaPolicyYearirrespective
of Policy type (Floater or Individual/ Multi-Individual) .
j. You need to intimate Us at least 72 hours prior to the date of travel
to switch off the policy as per process mentioned in G.I.17. We
would require the following details:
a. Date and time of leaving India
b. Date and time of your return to India
k. In case You arrive back to India earlier than the date informed to
Us, then You need to intimate us at least 24 hours prior to the
return travel to India in order to Switch On the Policy. If out of all
members who travelled, only one or few members return to India
earlier than the date informed to Us, then the Policy shall be
switched on from the earliest date of return to India for all the
members.
l. Your coverage shall be switched off and reactivated as per the
details provided in clause (j) above subject to a maximum
switch off period of 30 days. If the return to India is later than
30 days from the date of Switch off, the coverage shall be
reactivatedimmediatelyafter30daysirrespectiveofyourreturn.
m. We may require the following documents to record the date of your
travel in order to Switch-Off and Switch-on the policy for You
a. Flight tickets of the Insured members travelling to abroad
b. Flight tickets of the Insured members travelling back to India
n. Your Policy coverage will be automatically activated based on the
informationpertainingtodateofreturnprovidedtousor30days
from the Switch Off date, whichever is earlier. In case of policy
termof2yearsand3years,youcanavailthisbeneteachyear
and the discount shall be accumulated during the policy period
which can be redeemed at the time of policy renewal as per the
below
a. If the policy is renewed with the same policy term or higher,
then 100% of the earned discount shall be adjusted in the
renewal premium as ‘Discount in renewal premium’.
b. If the policy is renewed with a reduced policy term, then the
earned discount shall be adjusted on a proportionate basis in
theratioasspeciedbelow:
RenewalPolicy
Term
DiscounttobeAdjusted=EarnedDiscountX
PreviousPolicy
Term
Illustration:PreviousPolicyTerm=3years;SwitchOffDiscount
Earnedover3years=`1,800
If
Renewed
Policy
Termis
Renewal
Premium
(Excluding
optional
covers,Rider
andtaxes)
SwitchOff
discountutilized
Renewal
Premium
Payableafter
adjusting
SwitchOff
discount
1 Year 13,000 600(1,800*1/3as
Insured is renewing
from 3 Year Policy Term
to 1 Year Policy Term)
12,400
2 Years 27,000 1,200(1,800*2/3as
Insured is renewing
from 3 Year Policy Term
to 2 Year Policy Term)
25,800
3 Years 42,000 1,800(Insuredis
renewing with the same
Policy Term of 3 years)
40,200
Illustration2:SwitchOffPeriod
TravelPeriod
From:15/01/2022 To:20/01/2022
Time:16:00hrs. Time:15:00hrs.
RequestedDateofSwitch
Off
15/01/2022
RequestedDateofSwitch
On
20/01/2022
Inthiscase,SwitchOffshallhappenon15/01/2022at23:59:59hrsand
SwitchOnshallhappenon20/01/2022at00:00:00hrs.
Forthepurposeofthisbenet,
Switch Off – means to deactivate all the covers in the Policy, except
coverage under Section D.IV.4 Personal Accident Cover and Section
D.III.4.ii Worldwide Emergency Hospitalization with Outpatient Cover
Section D.IV.6 Critical Illness Add-on, from the requested Switch Off
date.
C.II.6. WellnessProgram
You can earn reward points by opting for Our Healthy Life
Management Program wherein you need to complete number of steps
per day as per the table given below, that will help You in improving
Your well-being.
HealthyLifeManagementProgram-RewardsStructure
No.ofdays
inaPolicy
Year
No.ofsteps
10,000
steps and
above per
day
8,000-
9,999 steps
per day
6,000-
7,999 steps
per day
Less than
6,000steps
per day
240days
and above
20% 15% 10% Nil
180-239
days
15% 10% 5% Nil
120-179
days
10% 5% Nil Nil
Conditionsunderthisbenet:
i. Thenumberofdaysspeciedinthetableaboveshouldfallunder
the rst 9 (nine) months of every Policy Year. The activities
undertakentowardsthisbenetduringthelast3(three)monthsof
the Policy Year shall not be considered for reward calculation.
ii. This wellness program is available only for the adult members with
age 18 years and above. However, in a Floater policy, this program
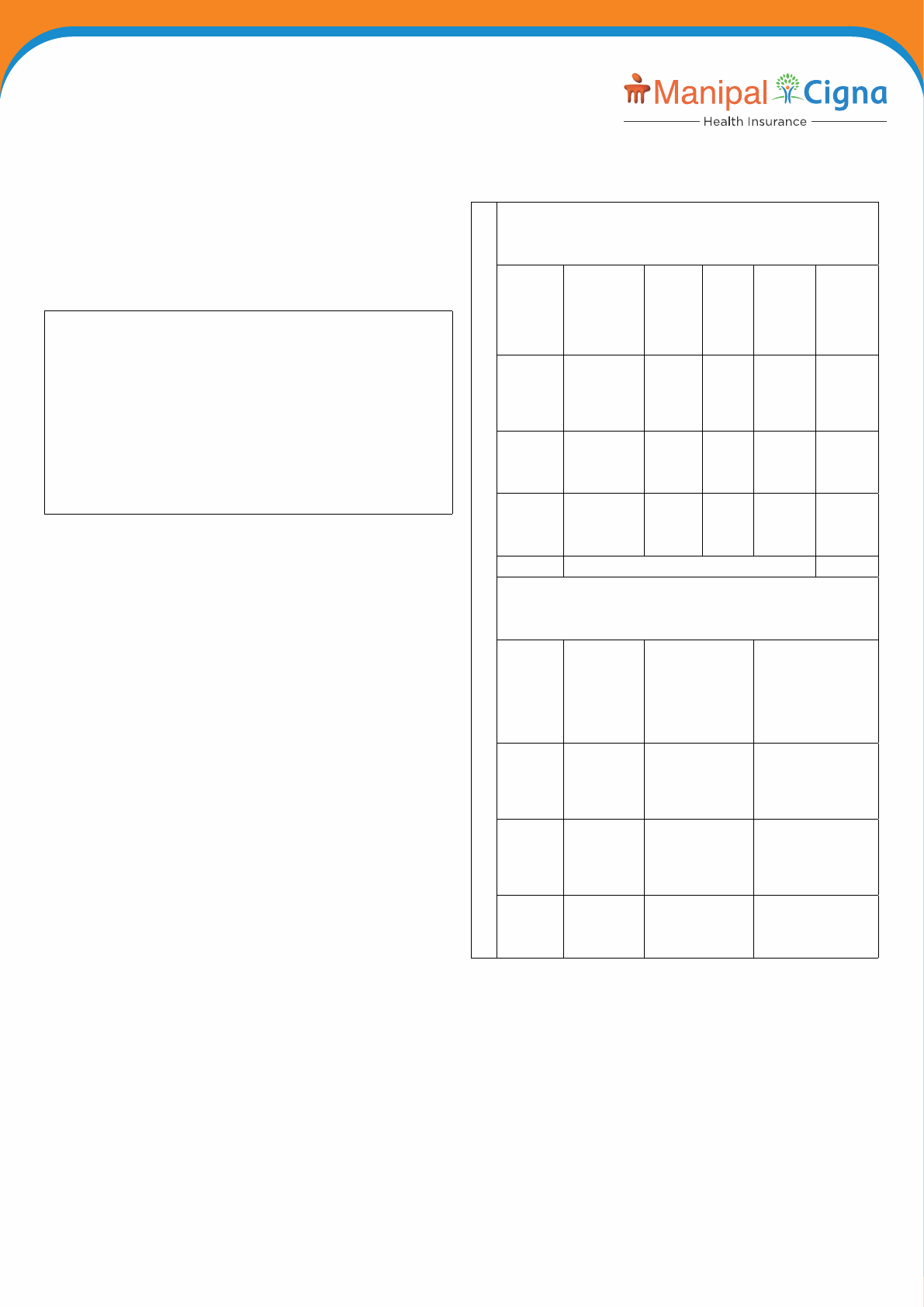
ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
shall be available only to the independent adult members and shall
not be available to dependent children.
iii. In an Individual Policy with one or more members, earning of
reward points will be at member level wherein each member can
earnUpto20%ofhis/herrespectiveexpiringbasepremiumasper
theapplicabletermsandconditionsbutinaoaterpolicy,earning
of reward points will be at policy level wherein all eligible members
cumulativelycanearnamaximumUpto20%oftheexpiringbase
premium as per the applicable terms and conditions.
iv. Inaoaterpolicytheaboverewardpercentagewouldbedivided
as per the number of eligible Adult Insured members as per the
below illustration.
Inaoaterpolicy,therewardpercentagewouldbedividedasperthe
number of eligible Adults covered.
For Example
In a 2A+2C policy, the Healthy Life Management Program shall be
applicablefor2Aonly.AssumingAdult1attainsascoreof10,000steps
perdayforaperiodof240daysandAdult2attainsascoreof6000
stepsperdayforaperiodof240days.
The reward points shall be calculated as per the below:
Adult1:20%/2=10%
Adult2:10%/2=5%
Hence,thetotalearnedrewardpointswouldbe10%+5%=15%ofthe
existing Policy premium (Excluding optional cover/ Rider and taxes).
v. No reward points will be allocated for any count of steps per day,
foraperiodoflessthan120days.
vi. Maximum reward points that can be earned in a single Policy Year
willbelimitedto20%ofthepremiumpaid(excludingpremiumfor
Optional covers, Riders and taxes) in the existing Policy. In case
of 2 or 3 year policies, maximum reward points that can be earned
shallnotexceed20%ofthetotalpremiumpaid(excludingpremium
for Optional covers, Riders and taxes) for 2 years or 3 years as
applicable.
vii. Each earned reward point will be valued at 1 Rupee. Accrued
rewards can be redeemed against payable premium (excluding
premium for Optional covers, Riders and Taxes) from 1st Renewal
of the Policy.
viii. The earned reward points can be utilized as Discount in the
renewal premium falling due immediately after the accrual. Carry
forward of earned reward points shall not be allowed.
ix. Redemption against renewal premium will be available only at the
time such renewal is due. Any earned rewards will lapse at the end
of the grace period if the policy is not renewed with us.
Refer Annexure- A below on the Illustration of Reward Points.
Annexure - A - Illustration of Healthy Life Management Program
Rewards
ReductionofRenewalPolicyYear
PolicyTerm-3years
(Premium indicated here is just for illustration purposes in case of 1
Adult policy and may not be the actual premium.)
Each earned reward point will be valued at 1 Rupee
Year Premium
(Excluding
optional
covers/
Riderand
taxes)
Activity No.of
Days
Reward
%
Reward
Points
Earned
Year 1 10000 10,000
and
above
steps/
day
240
days
and
above
20% 2000
Year 2 11000 8,000
- 9,999
steps/
day
240
days
and
above
15% 1650
Year 3 12000 6,000
- 7,999
steps/
day
240
days
and
above
10% 1200
Total 33000 4850
The earned reward points could be redeemed as discount as per
the below process to pay a portion of the renewal premium
RenewalofPolicyasperbelowtable
If
Renewed
Policy
Termis
Renewal
Premium
(Excluding
optional
covers,
Riderand
taxes)
Reward
discountutilized
RenewalPremium
Payableafter
adjustingReward
discount
1 Year
Policy
13000 1617(4850*1/3
as Insured is
renewing 3 Year
policy to 1 Year
Policy)
11383
2 Years
Policy
27000 3233(4850*2/3
as Insured
renewing 3 Year
policy to 2 Year
Policy)
23767
3 Years
Policy
42000 4850(Insured
renewing to the
same policy
tenure of 3 years)
37150

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
Increase of Renewal Policy Year
PolicyTerm-1years
(Premium indicated here is just for illustration purposes and may not
be the actual premium.)
Each earned reward point will be valued at 1 Rupee
Year Premium
paid
(Excluding
optional
cover,
Riderand
taxes)
Activity No.
of
Days
Rewards
%
Points
Earned
Year 1 10000 6,000
- 7,999
steps /
day
180
- 239
days
5% 500
Total 10000 500
The earned reward points could be redeemed as discount as per the
below process to pay a portion of the renewal premium
RenewalofPolicyasperbelowtable
If
Renewed
Policy
Termis
Renewal
Premium
(Excluding
optional
cover,
Riderand
taxes)
Rewards
discount
utilized
RenewalPremiumPayable
afteradjustingRewards
discount
1 Year
Policy
11000 500(as
Insured is
renewing
1 Year
policy to
1 Year
Policy)
10500
2 Year
Policy
21000 500(as
Insured is
renewing
1 Year
policy to
2 Year
Policy)
20500
3 Year
Policy
33000 500(as
Insured is
renewing
1 Year
policy to
3 Year
Policy)
32500
The notications related to wellness program will be communicated
via SMS, email and the program specic phone/ web application.
Details about reward points will be available on the program app (if
any) or would be shared through SMS and/or Renewal Notice which
would be sent to customers.
C.II.7 DiscountfromNetworkProviders
The Insured Person can avail discounts on Diagnostics, Pharmacy
and Health Supplements offered through our Network Providers.
C.II.8 PremiumWaiverBenet
In case, the Policyholder who is also an Insured Person under the
Policy suffers Death due to an injury caused by an Accident within
365 days from the date of the event or he/she is diagnosed with a
Critical Illness, listed under this section, We will pay the next one full
Policy Year’s Renewal Premium (including Optional covers, Riders and
Taxes) of the Policy, for a policy tenure of 1 year. The premium shall be
paid towards existing Insured Persons covered under the same policy,
withbenetssameastheexpiringPolicy.
IncaseofanychangeinPolicybenets,completepremiumwillbepaid
by the Policyholder.
The cover is available subject to below conditions:
• If only one person is covered under the Policy, policy will not be
renewed in case of death of the Policyholder.
• The Policyholder is not added in the Policy in the middle of the
PolicyYear.There is nochangeincovers, SumInsured,benet
structure, limits and conditions applicable under the Policy, at the
time of renewal.
• No new member is being added under the renewed Policy.
• In case of a policy with existing tenure of 2 or 3 years, it will be
renewed only for one year, provided all the terms and conditions,
benetsandpolicylimitsremainsame.
Forthepurposeofthisbenet,CriticalIllnessesshallinclude–
a) CancerofSpeciedSeverity
b) MyocardialInfarction(FirstHeartAttackofSpecicSeverity)
c) Open Chest CABG
d) Open Heart Replacement or Repair of Heart Valves
e) ComaofSpeciedSeverity
f) Kidney Failure Requiring Regular Dialysis
g) Stroke Resulting in Permanent Symptoms
h) Major Organ/Bone Marrow Transplant
i) Permanent Paralysis of Limbs
j) Motor Neuron Disease with Permanent Symptoms
k) Multiple Sclerosis with Persisting Symptoms
Onceaclaimhasbeenacceptedandpaidunderthisbenet,thiscover
will automatically terminate in respect of that Insured Person.
Any claim under this benet will not impact the Sum Insured and/or
Cumulative Bonus and/or Cumulative Bonus Booster.
C.III. OptionalPackages
These optional packages shall be available to all eligible Insured
Persons covered under the Policy. Selection of this package is allowed
at Policy level only.
The limits specied under below optional package shall override
the applicable limits mentioned as part of base cover for the respective
coverages.
The Insured Person can opt for any one of the below packages.
C.III.1 EnhancePlus
(Applicable for Protect Plan)
C.III.1.i Maternity&NewBornHospitalizationExpenses
A. MaternityExpenses
We will cover Maternity Expenses up to Maternity Sum insured and as
perPlanoptedandasspeciedinthePolicyScheduleforthedelivery
of a child and/ or Maternity Expenses incurred during the Policy Year,
related to a Medically Necessary and lawful termination of pregnancy
up to maximum 2 deliveries or terminations during the lifetime of an
Insured Person.
You understand and agree that:
(a) Our maximum liability per delivery or termination is subject to the
MaternitySumInsuredspeciedinthePolicySchedule.
(b) The female adult Insured Person should have been continuously
covered under this Policy for at least 36 months before availing this
benet.
(c)Thecoverunderthisbenetshallberestrictedtotwochildrenonly.
(d)Thepaymenttowardsanyadmittedclaimunderthisbenetforany
complication arising out of or as a consequence of maternity or
childbirthwillberestrictedtoMaternitySumInsuredspeciedin
the Policy Schedule however any restored amount will not be
available for coverage under this section.
(e) Pre or post natal Maternity Expenses will be covered within the
Maternity Sum Insured under this benet however; any Pre or
Post-hospitalization Expenses under Section D.I.2 and D.I.3,
abovewillnotbeapplicableforthisbenet.
(f) Maternity Sum Insured available under Maternity Expenses will be
in addition to Sum Insured.
(g) Applicable Deductible under the applicable plan shall also apply to
thisbenet.
(h) WewillnotcoverthefollowingexpensesunderMaternityBenet:
i) Medical Expenses in respect of the harvesting and storage
of stem cells when carried out as a preventive measure against
possible future Illnesses.
ii) Medical Expenses for ectopic pregnancy. However, these

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
expenses will be covered under the In-patient Hospitalization
under Section D.I.1.
(i) Exclusion E.I.18 shall not apply to this cover subject to terms and
conditionsunderthisbenet
B. NewBornBabyExpenses:
Subject to a claim being admitted under Maternity Expenses under
Section D.III.1.i.A, We will cover.
(a) Medical Expenses towards treatment of the New Born Baby while
the Insured Person is hospitalized as an In-patient for delivery.
(b) The Reasonable and Customary Charges incurred on the New
Born Baby during and post birth up to 90 days from the date of
delivery, within the limits specied in the Policy Schedule under
Maternity Expenses without payment of any additional premium.
(c) Any restored Sum Insured will not be available for coverage under
this section
(d) Subject to the underwriting and to the terms and conditions of the
Policy, We will cover the New Born Baby beyond 90 days on
payment of requisite premium for the New Born Baby into the
Policy by way of an endorsement or at the next Renewal, whichever
is earlier.
Applicable Deductible under the applicable plan shall also apply to
thisbenet.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C. FirstYearVaccinations
We will cover Reasonable and Customary charges for vaccination
expenses for the New Born Baby as per National Immunization
Scheme (India) listed below, till the baby completes 1 year (12 months)
within the limits specied in the Policy Schedule under Maternity
Expenses without payment of any additional premium. In case the
Policy ends before the New Born Baby has completed 1 year (12
months),thecoverageunderthisbenetshallcontinuesubjecttothe
Policy being renewed in the subsequent year. Any restored Sum
Insured will not be available for coverage under this section.
Time Interval Vaccinations to be done (Age) Frequency
0–3months
BCG (Birth to 2 weeks) 1
OPV(0‚6‚10weeks)OROPV+IPV1
(6,10weeks)
3 OR 4
DPT(6&10week) 2
Hepatitis-B(0&6week) 2
Hib(6&10week) 2
3 – 6 months
OPV (14 week) OR OPV + IPV2 1 or 2
DPT (14 week) 1
Hepatitis-B (14 week) 1
Hib (14 week) 1
9 months Measles (+9 months) 1
12 months Chicken Pox (12 months) 1
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5.
C.III.1.ii RoomAccommodationUpgrade
We will upgrade the Room category coverage under Section D.I.1 In-
patient hospitalization up to ‘Any Room Category’ subject to maximum
ofSumInsuredOptedandasspeciedinthePolicySchedule.
C.III.1.iii HealthMaintenanceBenet
We will cover, up to limits specied in the Policy Schedule, by way
of reimbursement of the Reasonable and Customary Charges for
below mentioned expenses incurred by the Insured Person for
Medically Necessary charges incurred during the Policy Year on an
Out Patient basis.
i. Consultation with Medical Practitioner, Diagnostic tests, preventive
tests, drugs, prosthetics, medical aids (spectacles and contact
lenses, hearing aids, crutches, wheel chair, walker, walking stick,
lumbo-sacral belt), prescribed by the specialist Medical Practitioner
uptothelimitsspeciedinthePolicySchedule.
ii. Towards Dental Treatments and AYUSH forms of Medicines
wherever prescribed by a Medical Practitioner.
Insured can use Our application or contact Us for scheduling an
appointment for availing services covered under this benet at our
Network provider.
Any unutilised Health Maintenance Benet limit shall lapse at the
end of the Policy Year. Fresh limits will be available as specied in
the Policy Schedule for the new Policy Year.
All Waiting Periods and Permanent Exclusions including Co-pay’s
applicable on the Policy under Section E shall not apply to this section.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
underSectionsG.I.14andG.I.18.Further,allclaimsunderthisbenet
will be subject to the any one claim limits specied under Section
G.I.18 of the Policy.
C.III.2 Assure
(Applicable for Sum Insured `3Lacs, `4 Lacs and `5 Lacs under
Protect Plan)
C.III.2.i RoomAccommodationLimit
We will limit the Room category coverage under Section D.I.1 In-
patienthospitalizationupto1%oftheoptedSumInsuredperdayand
asspeciedinthePolicySchedule.ForICUaccommodation,wewill
coverupto2%oftheoptedSumInsuredperdayandasspeciedin
the Policy Schedule.
If the Insured Person is admitted in a room category/ limit that is higher
than the one that is specied in the Policy Schedule, then the
Policyholder/Insured Person shall bear a ratable proportion of the total
Associated Medical Expenses (including surcharge or taxes thereon)
in the proportion of the difference between the room rent of the entitled
room category to the room rent actually incurred.
C.III.2.iiDiseaseSpecicSub-limits
We will indemnify the Medical Expenses under Section D.I.1 In-patient
hospitalization incurred by an Insured Person in respect of the below
listed ailments / procedures (refer the table below) up to the limits
speciedagainsteachandeveryailment/procedurefortheapplicable
Sum Insured options:
Sum Insured (in `) `3 & `4
Lacs
`5 Lacs
Treatment for each Ailment / Procedure
mentioned below:
1. Surgery for treatment of all
types of Hernia
2. Hysterectomy
3. Surgeries for benign Prostate
Hypertrophy
4. Surgical treatment of stones of renal
system
`50,000 `65,000
Treatment of Cataract (Per Eye)
`20,000 `30,000
Treatment of Total Knee replacement
(Per knee)
`80,000 `1,00,000
Treatment for breakage of bones
`2,00,000 `2,50,000
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 and G.I.5.
C.III.2.iii ModernandAdvancedTreatments
We will cover the following procedures (wherever medically indicated)
either as In-patient or as part of Day Care Treatment in a hospital up
to10%oftheSumInsuredasspeciedinthePolicySchedule,during
the Policy Year:
a. Uterine Artery Embolization and HIFU (High intensity focused
ultrasound)
b. Balloon Sinuplasty
c. Deep Brain stimulation
d. Oral chemotherapy
e. Immunotherapy - Monoclonal Antibody to be given as injection
f. Intra vitreal injections
g. Robotic surgeries
h. Stereotactic radio surgeries

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
i. Bronchial Thermoplasty
j. Vaporization of the prostrate (Green laser treatment or holmium
laser treatment)
k. IONM - (Intra Operative Neuro Monitoring)
l. Stem cell therapy: Hematopoietic stem cells for bone marrow
transplant for hematological conditions to be covered.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 and G.I.5.
C.III.3 Enhance
(Applicable for Advantage Plan)
C.III.3.i Maternity&NewBornHospitalizationExpenses
A. MaternityExpenses
We will cover Maternity Expenses up to Maternity Sum insured and as
perPlanoptedandasspeciedinthePolicyScheduleforthedelivery
of a child and/ or Maternity Expenses incurred during the Policy Year,
related to a Medically Necessary and lawful termination of pregnancy
up to maximum 2 deliveries or terminations during the lifetime of an
Insured Person.
You understand and agree that:
(a) Our maximum liability per delivery or termination is subject to the
MaternitySumInsuredspeciedinthePolicySchedule.
(b) The female adult Insured Person should have been continuously
covered under this Policy for at least 36 months before availing this
benet.
(c)Thecoverunderthisbenetshallberestrictedtotwochildrenonly.
(d) Thepaymenttowardsanyadmittedclaimunderthisbenetforany
complication arising out of or as a consequence of maternity or
childbirthwillberestrictedtoMaternitySumInsuredspeciedin
the Policy Schedule however any restored amount will not be
available for coverage under this section.
(e) Pre or post-natal Maternity Expenses will be covered within the
Maternity Sum Insured under this benet however; any Pre or
Post-hospitalization Expenses under Section D.I.2 and D.I.3,
abovewillnotbeapplicableforthisbenet.
(f) Maternity Sum Insured available under Maternity Expenses will be
in addition to Sum Insured.
(g) Applicable Deductible under the applicable plan shall also apply to
thisbenet.
(h)WewillnotcoverthefollowingexpensesunderMaternityBenet:
i) Medical Expenses in respect of the harvesting and storage
of stem cells when carried out as a preventive measure against
possible future Illnesses.
ii) Medical Expenses for ectopic pregnancy. However, these
expenses will be covered under the In-patient Hospitalization
under Section D.I.1.
Exclusion E.I.18 shall not apply to this cover subject to terms and
conditionsunderthisbenet
B. NewBornBabyExpenses
Subject to a claim being admitted under Maternity Expenses under
Section D.III.3.i.A, We will cover.
(a) Medical Expenses towards treatment of the New Born Baby while
the Insured Person is hospitalized as an In-patient for delivery.
(b) The Reasonable and Customary Charges incurred on the New
Born Baby during and post birth up to 90 days from the date of
delivery, within the limits specied in the Policy Schedule under
Maternity Expenses without payment of any additional premium.
(c) Any restored Sum Insured will not be available for coverage under
this section
(d) Subject to the underwriting and to the terms and conditions of
thePolicy,WewillcovertheNewBornBabybeyond90dayson
payment of requisite premium for the New Born Baby into the
Policy by way of an endorsement or at the next Renewal, whichever
is earlier.
Applicable Deductible under the applicable plan shall also apply to this
benet.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C. FirstYearVaccinations
We will cover Reasonable and Customary charges for vaccination
expenses for the New Born Baby as per National Immunization
Scheme (India) listed below, till the baby completes 1 year (12 months)
within the limits specied in the Policy Schedule under Maternity
Expenses without payment of any additional premium. In case the
Policy ends before the New Born Baby has completed 1 year (12
months),thecoverageunderthisbenetshallcontinuesubjecttothe
Policy being renewed in the subsequent year. Any restored Sum
Insured will not be available for coverage under this section.
Time Interval Vaccinations to be done (Age) Frequency
0–3months
BCG (Birth to 2 weeks) 1
OPV(0‚6‚10weeks)OROPV+IPV1
(6,10weeks)
3 OR 4
DPT(6&10week) 2
Hepatitis-B(0&6week) 2
Hib(6&10week) 2
3 – 6 months
OPV (14 week) OR OPV + IPV2 1 or 2
DPT (14 week) 1
Hepatitis-B (14 week) 1
Hib (14 week) 1
9 months Measles (+9 months) 1
12 months Chicken Pox (12 months) 1
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5.
C.III.3.iiRoomAccommodationUpgrade
We will upgrade the Room category coverage under Section D.I.1
In-patient hospitalization up to ‘Any Room Category’ subject to
maximum of Sum Insured Opted and as specied in the Policy
Schedule.
C.III.4 Freedom
(Applicable for Protect and Advantage Plans)
This package is available to all Insured Persons provided they are
Indian resident at inception of the Policy and at subsequent renewals
of this policy.
C.III.4.i RoomAccommodationUpgrade
We will upgrade the Room category coverage under Section D.I.1
In-patient hospitalization up to ‘Any Room Category’ subject to
maximum of Sum Insured Opted and as specied in the Policy
Schedule.
C.III.4.iiWorldwideEmergencyHospitalizationwithOutpatientCover
We will cover Medical Expenses incurred during the Policy Year, for
Emergency In-patient Hospitalization Treatments or Emergency
Outpatient Treatment of the Insured Person incurred outside India,
covered up to Sum Insured as specied in the Policy Schedule,
provided that:
(a)The treatment is Medically Necessary and has been certied as
an Emergency by a Medical Practitioner, where such treatment
cannot be postponed until the Insured Person has returned to India
and is payable under Section D.I.1 ‘In-patient Hospitalization’ and/
or D.I.12 ‘Outpatient Expenses’ of the Policy.
(b) The Medical Expenses payable shall be limited to Emergency
In-patient Hospitalization and Emergency Outpatient only.
(c) AnypaymentunderthisbenetwillonlybemadeinIndia,inIndian
rupees on a reimbursement basis and subject to maximum of Sum
Insured. Insured Person can contact Us at the numbers provided
on the Health Card for any claim assistance. In case where
Cumulative Bonus accumulated is used for payment of claim
underthisbenet,themaximumliabilityunderasinglePolicyyear
shall not exceed the Opted Sum Insured including Cumulative
Bonus or Cumulative Bonus Booster as applicable.
(d)Thepaymentofanyclaimunderthisbenetwillbebasedonthe
rate of exchange as on the date of payment to the Hospital
published by Reserve Bank of India (RBI) and shall be used for

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
conversion of foreign currency into Indian rupees for payment
of claim. You further understand and agree that where on the
date of discharge, if RBI rates are not published, the exchange rate
next published by RBI shall be considered for conversion.
(e) You have given Us, intimation of such hospitalization within 48
hours of admission.
(f) Any claim made under this benet will be as per the claims
procedure provided under Clause G.1.5 and G.I.15 of this Policy.
(g)Anyclaim payableunderthisbenetis overandabovetheSum
Insured.
(h) Restoration of Sum Insured shall not be available under this
benet.
(i) ExclusionE.II.13doesnotapplytothisbenet.
C.IV Optionalcovers
The following optional covers shall apply under the Policy for an
Insured Person if specically mentioned on the Policy Schedule
and shall apply to all Insured Persons under a single policy without any
individual selection.
C.IV.1 Non-MedicalItems
We will cover the cost of Non-Medical items, listed under Annexure III
List 1 of the Policy, incurred towards Medically Necessary
Hospitalization of the insured person, arising out of Disease/ Illness or
Injury.
The cover is available subject to the claim being admissible under
Section D.I.1 ‘In-patient Hospitalization’ and/ or Section D.I.4 Day Care
Treatment cover under this policy and the expenses on Non-medical
items are related to the same Illness/ Injury.
ExclusionE.II.18shallnotbeapplicableforthisbenet.
AnyclaimmadeunderthisoptionalbenetwillreducetheSumInsured.
Allclaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.IV.2 Deductible
You can opt for a Deductible of `10,000 or `25,000 in the Policy.
Wherever a Deductible is selected such amount will be applied for each
Policy Year on the aggregate of all Claims in that Policy Year other than
forclaimsunderxedbenetcoversandHealthCheckUps.Deductible
shall apply to all sections other than D.IV.4 Personal Accident Cover,
D.I.13 Daily Cash for Shared Accommodation, D.I.12 Outpatient
Expenses, D.II. Value added covers and Add On Riders if opted.
For the purpose of calculating the deductible and assessment of
admissibility all claims must be submitted in accordance with Section
G.I.16 of Claims Process.
ForDeductibleofRs10,000,thecovercanbeoptedeitheratinception
or can be opted or removed at the time of Policy Renewal.
ForDeductibleofRs.25,000,thecovercanbeoptedeitheratinception
or at the time of Policy Renewal. However once opted, the Insured
Person can remove the Deductible of Rs 25,000 onlyat the time of
renewal falling immediately due after 4 continuous Policy Years or any
subsequent renewals thereon, from the year of opting Rs 25,000
Deductible
This benet shall not be available if D.III.2 Assure optional package is
opted.
All other terms, conditions, waiting periods and exclusions shall apply.
C.IV.3 InfertilityTreatment
We will cover the Medical Expenses of the eligible Insured Person
if hospitalized on the advice of the Medical Practitioner for Infertility
Treatments up to maximum of `2.5 lacs as per Sum Insured opted
andasspeciedinPolicyScheduleprovidedthat,
a. D.III.1 ‘Enhance Plus’ or D.III.3 ‘Enhance’ Optional Package is
opted and Sum Insured opted under the Policy and mentioned in
Policy Schedule is `7.5 lacs and above.
b. This cover is limited to IVF and/or IUI treatments.
c. The Insured Person should have been continuously covered under
thisPolicyforatleast36monthsbeforeavailingthisbenet.
d. The benet shall be restricted to two successful procedures
leading to conception during the lifetime of the eligible Insured
Person and the coverage shall terminate thereafter
e. Sum Insured available under this section will be in addition to
Maternity Sum Insured under Section D.III.1.i Maternity & New Born
Hospitalization Expenses or D.III.3.i Maternity & New Born
Hospitalization Expenses
f. Restoration of Sum Insured shall not be available under this
benet.
g. Exclusion E.I.17 shall not apply to this cover subject to terms and
conditionsunderthisbenet
h. The cover shall automatically cease upon the eligible Insured
Personattaining60yearsofage.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.IV.4 PersonalAccidentCover
We will pay two times of the Sum Insured opted subject to maximum of
`50 Lacs, as specied in the Policy Schedule, in case the Insured
Person suffers an Injury solely and directly due to an Accident that
occurs during the Policy Period and such Injury solely and directly
results in the Insured Person’s Death or Permanent Total Disablement
whichisofthenaturespeciedbelowwithin365daysoftheAccident.
TableofBenets Percentage
oftheSum
Insured
payable
a. Type of Permanent Total Disablement
i) Total and irrecoverable loss of sight of both eyes 100%
ii) Loss by physical separation or total and permanent
loss of use of both hands or both feet
100%
iii) Loss by physical separation or total and
permanent loss of use of one hand and one foot
100%
iv) Total and irrecoverable loss of sight of one eye and
loss of a Limb
100%
v) Total and irrecoverable loss of hearing of both ears
and loss of one Limb/loss of sight of one eye
100%
vi) Total and irrecoverable loss of hearing of both ears
and loss of speech
100%
vii) Total and irrecoverable loss of speech and loss of
one Limb/loss of sight of one eye
100%
viii) Permanent total and absolute disablement (not
falling under the above) disabling the Insured
Person from engaging in any employment or
occupationorbusinessforremunerationorprot,
of any description whatsoever which results in
“Loss of Independent Living”
100%
Forthepurposeofthisbenet,
- Limb means a hand at or above the wrist or a foot above the ankle;
- Physical separation of one hand or foot means separation at or
above wrist and/or at or above ankle, respectively.
Thebenetsasspeciedabovewillbepayableprovidedthat:
a. The Permanent Total Disablement is proved to Our satisfaction;
and a disability certicate issued by a Civil Surgeon or the
equivalent appointed by the District/State or Government Board;
and
b. The Permanent Total Disablement continues for a period of at least
180 days from the commencement of the Permanent Total
Disablement;providedthatWemustbe satisedatthe expiryof
the 180 days that there is no reasonable medical hope of
improvement.
c. If We have admitted a claim for Permanent Total Disablement
inaccordancewiththisbenet,thenWeshallnotbeliabletomake
anypaymentunderthisbenetonthedeathoftheInsuredPerson,
if the Insured Person subsequently dies.
d. Onceaclaimhasbeenacceptedandpaidunderthisbenetincase
of Death then cover under this Policy shall immediately and
automatically cease in respect of that Insured Person.
e. Restoration of Sum Insured shall not be available under this
benet.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
C.IV.5 CumulativeBonusBooster
WewillprovideanoptiontoincreasetheSumInsuredby50%foreach
policyyearuptoamaximumof200%ofSumInsuredprovidedthatthe
Policy is renewed with Us without a break.
a. No cumulative bonus will be added if the Policy is not renewed
with Us by the end of the Grace Period. The Cumulative Bonus
will not be accumulated in excess of 200% of the Sum Insured
under the current Policy with Us.
b. Any earned Cumulative Bonus will not be reduced for claims made
in the future, wherever the earned Cumulative Bonus is used for
payment of a claim during a particular Policy Year.
c. In case of opting for Cumulative Bonus Booster, the Cumulative
Bonus under section D.II.4 shall not be available, however all
terms and conditions of the said section shall apply.
d. This Cumulative bonus shall not be available for claims made for
Value added cover (Section D.II) and also for D.III.1.i Maternity
& New Born Hospitalization Expenses, D.III.3.i Maternity & New
Born Hospitalization Expenses, D.III.1.iii Health Maintenance
Benet,D.I.10AirAmbulanceCover,D.I.12OutpatientExpenses,
D.I.13 Daily Cash for Shared Accommodation and D.IV.3 Infertility
Treatment
C.IV.6 Addon-CriticalIllnessRider
Along with this Product You can also avail the ManipalCigna Critical
IllnessAddOnCover(UIN:MCIHLIP21128V022021)oritssubsequent
revisions. Please ask for the Prospectus and Proposal Form of the
same at the time of purchase. All waiting periods, exclusions and terms
and conditions of applicable rider including medical check-up
requirement will apply.
ForthepurposeofthisBenet,CriticalIllnesswillbeaslistedunderthe
ManipalCigna Critical Illness Add on Cover Policy documents.
D. Exclusions
We shall not be liable to make any payment under this Policy caused
by, based on, arising out of or howsoever attributable to any of the
following unless otherwise covered or specied under the Policy or
any Cover opted under the Policy. All the waiting period shall be
applicable individually for each Insured Person and claims shall be
assessed accordingly.
D.I StandardExclusions
D.I.1 Pre-existingDisease-Code-Excl.01
a. Expenses related to the treatment of a Pre-existing Disease
(PED) and its direct complications shall be excluded until the
expiry of the applicable waiting period
a. 24 months of continuous coverage from the date of
commencement of coverage for Sum Insured `7.5 Lacs and
above
b. 36 months of continuous coverage from the date of
commencement of coverage for Sum Insured Up to `5 Lacs.
b. In case of enhancement of sum insured, the exclusion shall apply
afresh to the extent of sum insured increase.
c. If the Insured Person is continuously covered without any break as
dened under the portability norms of the extant IRDAI (Health
Insurance) Regulations then waiting period for the same would be
reduced to the extent of prior coverage.
d. Coverage under the policy after the expiry of Pre-existing disease
waiting period for any pre-existing disease is subject to the same
being declared at the time of application and accepted by us.
D.I.2 Specieddisease/procedureWaitingPeriod-Code-Excl.02
a. Expenses related to the treatment of the listed Conditions,
surgeries/treatments shall be excluded until the expiry of 24 months
ofcontinuouscoverageafterthedateofinceptionoftherstpolicy
with us. This exclusion shall not be applicable for claims arising
due to an accident.
b. In case of enhancement of sum insured the exclusion shall apply
afresh to the extent of sum insured increase.
c. If any of the specied disease/procedure falls under the waiting
periodspeciedforpre-Existingdiseases,thenthelongerofthe
two waiting periods shall apply.
d. The waiting period for listed conditions shall apply even if
contracted after the policy or declared and accepted without a
specicexclusion.
e. If the Insured Person is continuously covered without any break
asdenedundertheapplicablenormsonportabilitystipulatedby
IRDAI, then waiting period for the same would be reduced to the
extent of prior coverage.
f. Listofspecicdiseases/procedures:
i. Cataract,
ii. Hysterectomy for Menorrhagia or Fibromyoma or prolapse of
Uterus or myomectomy for broids unless necessitated by
malignancy,
iii. Knee Replacement Surgery (other than caused by an
Accident), Non-infectious Arthritis, Gout, Rheumatism,
Osteoarthritis and Osteoporosis, Joint Replacement Surgery
(other than caused by Accident), Prolapse of Intervertebral
discs(other than caused by Accident), all Vertebrae Disorders,
including but not limited to Spondylitis, Spondylosis,
Spondylolisthesis, Congenital Internal,
iv. Varicose Veins and Varicose Ulcers,
v. Stones in the urinary uro-genital and biliary systems including
calculus diseases and complications thereof,
vi. Benign Prostate Hypertrophy, all types of Hydrocele,
vii. Fissure, Fistula in anus, Piles, all types of Hernia, Pilonidal
sinus, Hemorrhoids and any abscess related to the anal region.
viii. Chronic Suppurative Otitis Media (CSOM), Deviated Nasal
Septum, Sinusitis and related disorders, Surgery on tonsils/
Adenoids, Tympanoplasty and any other benign ear, nose and
throat disorder or surgery.
ix. gastric and duodenal ulcer, any type of Cysts/Nodules/
Polyps/internal tumors/skin tumors, and any type of Breast
lumps(unless malignant), Polycystic Ovarian Diseases,
x. Any surgery of the genito-urinary system unless necessitated
by malignancy.
If these diseases are pre-existing at the time of proposal or
subsequently found to be pre-existing the pre-existing waiting
periods as mentioned in the Policy Schedule shall apply.
D.I.3 30daysWaitingPeriod-Code-Excl.03
a) Expenses related to the treatment of any illness within 30 days
ofcontinuouscoveragefromtherstpolicycommencementdate
shall be excluded except claims arising due to an accident,
provided the same are covered.
b) This exclusion shall not, however, apply if the Insured Person has
Continuous Coverage for more than twelve months.
c) The within referred waiting period is made applicable to the
enhanced sum insured in the event of granting higher sum insured
subsequently
D.I.4 Investigation&Evaluation-Code-Excl04
a. Expenses related to any admission primarily for diagnostics and
evaluation purposes only are excluded.
b. Any diagnostic expenses which are not related or not incidental to
the current diagnosis and treatment are excluded.
D.I.5 RestCure,rehabilitationandrespitecare-Code-Excl05
a) Expenses related to any admission primarily for enforced bed rest
and not for receiving treatment. This also includes:
i. Custodial care either at home or in a nursing facility for personal
care such as help with activities of daily living such as bathing,
dressing, moving around either by skilled nurses or assistant or
non-skilled persons.
ii. Any services for people who are terminally ill to address
physical, social, emotional and spiritual needs.
D.I.6 Obesity/WeightControl:Code-Excl06
Expensesrelatedtothesurgicaltreatmentofobesitythatdoesnotfull
all the below conditions:
1. Surgery to be conducted is upon the advice of the Doctor
2. The surgery/Procedure conducted should be supported by clinical
protocols
3. The member has to be 18 years of age or older and
4. Body Mass Index (BMI);
a. greaterthanorequalto40or

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
b. greater than or equal to 35 in conjunction with any of the
following severe comorbidities following failure of less invasive
methods of weight loss:
i. Obesity-related cardiomyopathy
ii. Coronary heart disease
iii. Severe Sleep Apnea
iv. Uncontrolled Type2 Diabetes
D.I.7 Change-of-Gendertreatments:Code-Excl07
Expenses related to any treatment, including surgical management, to
change characteristics of the body to those of the opposite sex.
D.I.8 CosmeticorPlasticSurgery:Code-Excl08
Expenses for cosmetic or plastic surgery or any treatment to change
appearance unless for reconstruction following an Accident, Burn(s) or
Cancer or as part of medically necessary treatment to remove a direct
and immediate health risk to the insured. For this to be considered a
medical necessity, it must be certied by the attending Medical
Practitioner
D.I.9 HazardousorAdventuresports:Code-Excl09
Expenses related to any treatment necessitated due to participation as
a professional in hazardous or adventure sports, including but not
limited to, para-jumping, rock climbing, mountaineering, rafting, motor
racing, horse racing or scuba diving, hand gliding, sky diving, deep-sea
diving.
D.I.10 Breachoflaw:Code-Excl10
Expenses for treatment directly arising from or consequent upon any
Insured Person committing or attempting to commit a breach of law
with criminal intent
D.I.11 ExcludedProviders:Code-Excl11
Expenses incurred towards treatment in any hospital or by any Medical
Practitioner or any other provider specically excluded by the
Insureranddisclosedinitswebsite/notiedtothePolicyholdersare
not admissible. However, in case of life threatening situations or
following an accident, expenses up to the stage of stabilization are
payable but not the complete claim.
D.I.12 Treatment for Alcoholism, drug or substance abuse or any
addictive condition and consequences thereof. Code-Excl12
D.I.13 Treatments received in heath hydros, nature cure clinics, spas
or similar establishments or private beds registered as a nursing home
attached to such establishments or where admission is arranged
wholly or partly for domestic reasons. Code- Excl13
D.I.14 Dietary supplements and substances that can be purchased
without prescription, including but not limited to Vitamins, minerals and
organic substances unless prescribed by a Medical Practitioner as part
of hospitalization claim or day care procedure. Code-Excl14
D.I.15 RefractiveError:Code-Excl15
Expenses related to the treatment for correction of eye sight due to
refractive error less than 7.5 diopters
D.I.16 UnprovenTreatments:Code-Excl16
Expenses related to any unproven treatment, services and supplies for
or in connection with any treatment. Unproven treatments are
treatments, procedures or supplies that lack signicant medical
documentation to support their effectiveness.
D.I.17 SterilityandInfertility:Code-Excl17
Expenses related to sterility and infertility. This includes:
i. Any type of contraception, sterilization
ii. Assisted Reproduction services including articial insemination
and advanced reproductive technologies such as IVF, ZIFT, GIFT,
ICSI
iii. Gestational Surrogacy
iv. Reversal of sterilization
D.I.18 Maternity:CodeExcl18
i. Medical treatment expenses traceable to childbirth (including
complicated deliveries and caesarean sections incurred during
hospitalization) except ectopic pregnancy;
ii. Expense towards miscarriage (unless due to an accident) and
lawful medical termination of pregnancy during the policy period.
D.II SpecicExclusions
D.II.1 MaternityWaitingPeriod
Any treatment arising from or traceable to pregnancy, childbirth
including caesarean section until 36 months of continuous coverage
has elapsed for the particular Insured Person since the inception of the
rst Policy with Us. However, this exclusion / waiting period will not
applytoEctopicPregnancyprovedbydiagnosticmeansandcertied
to be life threatening by the attending Medical Practitioner.
D.II.2 PersonalWaitingperiod:
A special Waiting Period not exceeding 48 months, may be applied to
individual Insured Persons for the list of acceptable Medical Ailments
listed under the Underwriting Manual of the Product, depending upon
declarations on the proposal form and existing health conditions. Such
waitingperiodsshallbespecicallystatedintheScheduleandwillbe
appliedonlyafterreceivingYourspecicconsent.
D.II.3 90 day waiting period for Critical Illness Add On Cover (if
opted)
Any critical illness contracted and/or the disease incepts or manifests
duringtherst90daysfromtheInceptionDateofthepolicywillnotbe
coveredunderthecriticalillnessbenetwhereveropted.
D.II.4 MentalIllnessCoverWaitingPeriod
Any treatment arising out of a condition caused by or associated to a
Mental illness or a medical condition under below mentioned ICD
Codes impacting mental health, shall not be covered until 24 months
of continuous coverage has elapsed for the particular Insured Person
sincetheinceptionoftherstPolicywithUs.
ICD 10 CODES DISEASES
F05 Delirium due to known physiological condition
F06 Other mental disorders due to known physiological
condition
F07 Personality and behavioural disorders due to known
physiological condition
F10 Alcohol related disorders
F20 Schizophrenia
F23 Brief psychotic disorders
F25 Schizoaffective disorders
F29 Unspeciedpsychosisnotduetoasubstanceor
known physiological condition
F31 Bipolar disorder
F32 Depressive episode
F39 Unspeciedmood[affective]disorder
F40 Phobic Anxiety disorders
F41 Other Anxiety disorders
F42 Obsessive-compulsive disorder
F44 Dissociative and conversion disorders
F45 Somatoform disorders
F48 Other nonpsychotic mental disorders
F60 Specicpersonalitydisorders
F84 Pervasive developmental disorders
F90 Attention-decithyperactivitydisorders
F99 Mentaldisorder,nototherwisespecied

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
D.II.5 BariatricSurgeryWaitingPeriod
Bariatric Surgery shall not be covered until 36 months of continuous
coverage has elapsed for the particular Insured Person since the
inceptionoftherstPolicywithUs
D.II.6 InfertilityTreatmentWaitingPeriod
Any treatment taken for Infertility Treatment until 36 months of
continuous coverage has elapsed for the particular Insured Person
sincetheinceptionoftherstPolicywithUs.
D.II.7 Dental Treatment, orthodontic treatment, dentures or Surgery of
any kind unless necessitated due to an Accident and requiring minimum
24 hours Hospitalization. Treatment related to gum disease or tooth
disease or damage unless related to irreversible bone disease involving
thejawwhichcannotbetreatedinanyotherway,unlessspecically
covered under the Policy.
D.II.8 Circumcision unless necessary for treatment of a disease, illness
or injury not excluded hereunder or due to an accident.
D.II.9 Instrument used in treatment of Sleep Apnea Syndrome (C.P.A.P.)
and Continuous Peritoneal Ambulatory Dialysis (C.P.A.D.) and Oxygen
Concentrator for Bronchial Asthmatic condition, Infusion pump or any
other external devices used during or after treatment.
D.II.10 External Congenital Anomaly or defects or any complications or
conditions arising therefrom.
D.II.11 Prostheses, corrective devices and medical appliances, which are
not required intra-operatively for the disease/ illness/ injury for which
the Insured Person was Hospitalized.
D.II.12 Any stay in Hospital without undertaking any treatment or any
other purpose other than for receiving eligible treatment of a type that
normally requires a stay in the hospital
D.II.13 Treatment received outside India other than for coverage under
D.III.4.ii Worldwide Emergency Hospitalization with Outpatient Cover
under Freedom optional package if opted.
D.II.14 Costs of donor screening or costs incurred in an organ transplant
surgery involving organs not harvested from a human body.
D.II.15 Any form of Non-Allopathic treatment (except AYUSH Treatment
(In-patient Treatment)), Hydrotherapy, Acupuncture, Reexology,
Chiropractic treatment or any other form of indigenous system of
medicine.
D.II.16 All Illness/expenses caused by ionizing radiation or contamination
by radioactivity from any nuclear fuel (explosive or hazardous form)
or from any nuclear waste from the combustion of nuclear fuel nuclear,
chemical or biological attack or in any other sequence to the loss.
D.II.17 All expenses caused by or arising from or attributable to foreign
invasion, act of foreign enemies, hostilities, warlike operations (whether
war be declared or not or while performing duties in the armed forces
of any country), participation in any naval, military or air-force operation,
civil war, public defense, rebellion, revolution, insurrection, military or
usurped power, active participation in riots, conscation or
nationalization or requisition of or destruction of or damage to property
by or under the order of any government or local authority.
D.II.18 All non-medical expenses including convenience items for personal
comfort not consistent with or incidental to the diagnosis and treatment
of the disease/illness/injury for which the Insured Person was
hospitalized - belts, collars, splints, slings, braces, stockings of any
kind, diabetic footwear, thermometer and any medical equipment
that is subsequently used at home except when they form part of room
expenses, procedure charges and cost of treatment. For complete list
of Non-medical expenses, please refer to the Annexure III List – I
“Items for which Coverage is not available in the Policy”
D.II.19 Any deductible amount or percentage of admissible claim under
co-payifapplicableandasspeciedinthePolicySchedule.
D.II.20 Existing diseases disclosed by the Insured Person (limited to
the extent of the ICD codes mentioned in line with Chapter IV,
Guidelines on Standardization of Exclusions in Health Insurance
Contracts,2019),providedthesameisappliedattheunderwritingand
consented by You/ Insured Person.
E. GeneralTermsandClauses
E.I StandardGeneralTermsandClauses
E.I.1 DisclosureofInformation
The Policy shall be null and void and all premium paid thereon shall be
forfeited to the Company in the event of misrepresentation, mis-
description or non-disclosure of any material fact by the policyholder.
(“ Material facts” for the purpose of this policy shall mean all relevant
information sought by the company in the proposal form and other
connected documents to enable it to take informed decision in the
context of underwriting the risk)
E.I.2 ConditionPrecedenttoAdmissionofLiability
ThetermsandconditionsofthePolicymustbefullledbytheInsured
Person for the Company to make any payment for claim(s) arising
under the policy.
E.I.3 ClaimSettlement(provisionforPenalInterest)
i. The Company shall settle or reject the claim, as the case may be,
within30daysfromthedateofreceiptoflastnecessarydocument.
ii. In the case of delay in the payment of a claim, the Company shall
be liable to pay interest to the policyholder from the date of receipt
of last necessary document to the date of payment of claim at a
rate2%abovethebankrate.
iii. However, where the circumstances of a claim warrant an
investigation in the opinion of the Company, it shall initiate and
complete such investigation at the earliest, in any case not later
than30daysfromthedateofreceiptoflastnecessarydocument.
In such cases, the Company shall settle or reject the claim within
45 days from the date of receipt of last necessary document.
iv. In case of delay beyond stipulated 45 days, the Company shall be
liable to pay interest to the policyholder at a rate 2% above the
bank rate from the date of receipt of last necessary document to
the date of payment of claim.
"Bank rate" shall mean the rate xed by the Reserve Bank of India
(RBl)atthe beginningofthenancial yearinwhichclaim hasfallen
due.
E.I.4 CompleteDischarge
Any payment to the policyholder, insured person or his/her nominees
or his/her legal representative or assignee or to the Hospital, as the
casemaybe,foranybenetunderthepolicyshallbeavaliddischarge
towards payment of claim by the Company to the extent of that amount
for the particular claim.
E.I.5 MultiplePolicies
- In case of multiple policies taken by an insured person during a
period from one or more insurers to indemnify treatment costs, the
insured person shall have the right to require a settlement of his/her
claim in terms of any of his/her policies. In all such cases, the insurer
chosen by the insured person shall be obliged to settle the claim as
long as the claim is within the limits of and according to the terms of the
chosen policy.
- Insured person having multiple policies shall also have the right to
prefer claims under this policy for the amounts disallowed under any
other policy / policies even if the sum insured is not exhausted. Then
the insurer shall independently settle the claim subject to the terms and
conditions of this policy.
- If the amount to be claimed exceeds the sum insured under a
single policy, the insured person shall have right to choose insurer from
whom he/she wants to claim the balance amount.
- Where an insured person has policies from more than one insurer
to cover the same risk on indemnity basis, the insured person shall
onlybeindemniedthetreatmentcostsinaccordancewiththeterms
and conditions of the chosen policy.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
E.I.6 Fraud
If any claim made by the insured person, is in any respect fraudulent,
or if any false statement, or declaration is made or used in support
thereof, or if any fraudulent means or devices are used by the insured
personoranyoneactingonhis/herbehalftoobtainanybenetunder
thispolicy,allbenetsunderthispolicyshallbeforfeited.
Any amount already paid against claims made under this policy which
are found fraudulent later shall be repaid by all recipients(s)/
Policyholder(s), who has made that particular claim, who shall be
jointly and severally liable for such repayment to the Insurer.
For the purpose of this clause, the expression "fraud" means any of
the following acts committed by the Insured Person or by his agent or
the hospital/doctor/any other party acting on behalf of the insured
person, with intent to deceive the insurer or to induce the insurer to
issue an insurance Policy: -
a) the suggestion, as a fact of that which is not true and which the
Insured Person does not believe to be true;
b) the active concealment of a fact by the Insured Person having
knowledge or belief of the fact;
c) anyotheractttedtodeceive;and
d) any such act or omission as the law specially declares to be
fraudulent
The company shall not repudiate the claim and/or forfeit the policy
benetsonthegroundsofFraud,iftheinsuredperson/beneciarycan
prove that the misstatement was true to the best of his knowledge
and there was no deliberate intention to suppress the fact or that
such misstatement of or suppression of such material fact are within
the knowledge of the Insurer.
E.I.7. Cancellation
i. The policyholder may cancel this policy by giving 15 days written notice
and in such an event, the Company shall refund premium for the
unexpired policy period as detailed below.
RefundGridas%ofPremium
Policy
Cancelation
Within (Days)
Policy Year-1 Policy Year-2 Policy Year-3
0-30Days 85.00% 87.50% 89.00%
31-90Days 75.00% 80.00% 82.50%
91 - 181 Days 50.00% 70.00% 75.00%
182 - 272 Days 30.00% 60.00% 70.00%
273 - 365 Days 0.00% 50.00% 60.00%
366 - 456 Days
NIL
35.00% 55.00%
457 - 547 Days 25.00% 45.00%
548 - 638 Days 15.00% 40.00%
639-730Days 0.00% 30.00%
731 - 821 Days
NIL
25.00%
822 - 912 Days 15.00%
913-1003
Days
5.00%
1004andmore
Days
0.00%
No refund will be processed for cancellation of policies with Premium
Payment Mode as Half-yearly, Quarterly or Monthly.
Notwithstanding anything contained herein or otherwise, no refunds of
premium shall be made in respect of Cancellation where, any claim has
beenadmittedorhasbeenlodgedoranybenethasbeenavailedby
the insured person under the policy.
ii. The Company may cancel the policy at any time on grounds of
misrepresentation, non - disclosure of material facts, fraud by the
insured person by giving 15 days written notice. There would be no
refund of premium on cancellation on grounds of misrepresentation,
non-disclosure of material facts or fraud.
E.I.8. Migration
The Insured Person will have the option to migrate the Policy to other
health insurance products/plans offered by the company by applying
for migration of the policy at least 30 days before the policy
renewal date as per IRDAI guidelines on Migration. If such person is
presently covered and has been continuously covered without any
lapses under any health insurance product/plan offered by the
company,theInsuredPersonwillgettheaccruedcontinuitybenetsin
waiting periods as per IRDAI guidelines on migration.
For Detailed Guidelines on Migration, kindly refer IRDAI Guidelines
RefNo:IRDAI/HLT/REG/CIR/003/01/2020
E.I.9. Portability
The insured person will have the option to port the policy to other
insurers by applying to such insurer to port the entire policy along with
all the members of the family, if any, at least 45 days before, but not
earlier than 60 days from the policy renewal date as per IRDAI
guidelines related to portability. If such person is presently covered and
has been continuously covered without any lapses under any health
insurance policy with an Indian General/Health insurer, the proposed
insured person will get the accrued continuity benets in waiting
periods as per IRDAI guidelines on portability.
For detailed Guidelines on Portability, kindly refer IRDAI Guidelines Ref
No:IRDAI/HLT/REG/CIR/003/01/2020andScheduleIofIRDAI(Health
Insurance)Regulations2016forthePortabilitynorms
E.I.10. RenewalofPolicy
The policy shall ordinarily be renewable except on grounds of fraud,
misrepresentation by the insured person.
i. The Company shall endeavour to give notice for renewal. However,
the Company is not under obligation to give any notice for renewal.
ii. Renewal shall not be denied on the ground that the insured person
had made a claim or claims in the preceding policy years.
iii. Request for renewal along with requisite premium shall be received
by the Company before the end of the policy period.
iv. At the end of the policy period, the policy shall terminate and can
be renewed within the Grace Period of 30/15 days, to maintain
continuity of benets without break in policy. Coverage is not
available during the grace period.
v. No loading shall apply on renewals based on individual claims
experience.
E.I.11. WithdrawalofPolicy
i. In the likelihood of this product being withdrawn in future, the
Companywillintimatetheinsuredpersonaboutthesame90days
prior to expiry of the policy.
ii. Insured person will have the option to migrate to similar health
insurance product available with the Company at the time of renewal
withalltheaccruedcontinuitybenetssuchascumulativebonus,
waiver of waiting period, as per IRDAI guidelines, provided the
policy has been maintained without a break.
E.I.12. MoratoriumPeriod
After completion of eight continuous years under the policy no look
back to be applied. This period of eight years is called as moratorium
period. The moratorium would be applicable for the sums insured of the
rstpolicyandsubsequentlycompletionof8continuousyearswould
be applicable from date of enhancement of sums insured only on the
enhanced limits. After the expiry of Moratorium Period no health
insurance claim shall be contestable except for proven fraud and
permanent exclusions specied in the policy contract. The policies
would however be subject to all limits, sub limits, co-payments,
deductibles as per the policy contract.
E.I.13. PremiumPaymentinInstalments(Whereverapplicable)
If the insured person has opted for Payment of Premium on an
Instalment basis i.e. Half Yearly, Quarterly or Monthly, as mentioned in
thePolicySchedule/CerticateofInsurance,thefollowingConditions
shall apply (notwithstanding any terms contrary elsewhere in the
policy).
i. Grace Period of 30 days would be given for Half-yearly and
Quarterly mode of payment and grace period of 15 days for
monthly mode of payment would be given to pay the instalment
premium due for the Policy.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
ii. During such grace period, coverage will not be available from the
due date of instalment premium till the date of receipt of premium
by Company.
iii. The insured person will get the accrued continuity benet in
respectofthe“WaitingPeriods”,“SpecicWaitingPeriods”inthe
event of payment of premium within the stipulated grace Period.
iv. No interest will be charged if the instalment premium is not paid on
due date.
v. In case of instalment premium due not received within the grace
period, the policy will get cancelled.
vi. In the event of a claim, all subsequent premium instalments shall
immediately become due and payable.
vii. The company has the right to recover and deduct all the pending
instalments, from the claim amount due under the policy.
E.I.14. Possibility of Revision of Terms of the Policy Including the
PremiumRates
The Company, with prior approval of IRDAI, may revise or modify the
terms of the policy including the premium rates. The insured person
shallbenotiedthreemonthsbeforethechangesareeffected.
E.I.15. FreeLookperiod
The Free Look period shall be applicable on new individual health
insurance policies and not on renewals or at the time of porting/
migrating the policy.
Theinsuredpersonshallbeallowedafreelookperiodoffteendays
from date of receipt of the policy document to review the terms and
conditions of the policy and to return the same if not acceptable.
If the insured has not made any claim during the Free Look Period, the
insured shall be entitled to
a. a refund of the premium paid less any expenses incurred by the
Company on medical examination of the insured person and the
stamp duty charges or;
b. where the risk has already commenced and the option of return
of the policy is exercised by the insured person, a deduction
towards the proportionate risk premium for period of cover or;
c. Where only a part of the insurance coverage has commenced,
such proportionate premium commensurate with the insurance
coverage during such period.
E.I.16. RedressalofGrievance
If you have a grievance that you wish us to redress, you may contact us
with the details of the grievance through:
Our website: www.manipalcigna.com
Email: [email protected],
Senior Citizens may write to us at -
TollFree:1800-102-4462
ContactNo.:+912261703600
Courier:AnyofOurBranchofceorcorporateofceduringbusiness
hours.
Insured Person may also approach the grievance cell at any of
company’s branches with the details of the grievance.
IfInsuredPersonisnotsatisedwiththeredressalofgrievancethrough
one of the above methods, insured person may contact the grievance
ofcer at, ‘The Grievance Cell, ManipalCigna Health Insurance
Company Limited, 401/402, Raheja Titanium, Western Express
Highway, Goregaon East, Mumbai - 400063, India or email -
For updated details of grievance ofcer, kindly refer link -
https://www.manipalcigna.com/grievance-redressal
IfInsuredpersonisnotsatisedwiththeredressalofgrievancethrough
above methods, the Insured Person may approach the ofce of
Insurance Ombudsman of the respective area/region for redressal of
grievance as per Insurance Ombudsman Rules 2017. The contact
details of Ombudsman ofces attached as Annexure I to this Policy
document.
Grievance may also be lodged at IRDAI Integrated Grievance
Management System - https://igms.irda.gov.in/
You may also approach the Insurance Ombudsman if your complaint is
openformorethan30daysfromthedateoflingthecomplaint.
E.I.17. Nomination
The policyholder is required at the inception of the policy to make a
nomination for the purpose of payment of claims under the policy in
the event of death of the policyholder. Any change of nomination shall
be communicated to the company in writing and such change shall be
effective only when an endorsement on the policy is made. In the event
of death of the policyholder, the Company will pay the nominee {as
namedinthePolicySchedule/PolicyCerticate/Endorsement(ifany)}
and in case there is no subsisting nominee, to the legal heirs or legal
representatives of the Policyholder whose discharge shall be treated as
fullandnaldischargeofitsliabilityunderthePolicy.
E.II. SpecicTermsandClauses
E.II.1. MaterialChange
Material information to be disclosed includes every matter that You are
aware of, that relates to questions in the Proposal Form and which is
relevant to Us in order to accept the risk of insurance and if so on what
terms. You must exercise the same duty to disclose those matters to Us
before the Renewal, extension, variation, endorsement or reinstatement
of the contract.
E.II.2. AlterationsinthePolicy
This Policy constitutes the complete contract of insurance. No change
or alteration will be effective or valid unless approved in writing which
will be evidenced by a written endorsement, signed and stamped by
Us.
E.II.3. ChangeofPolicyholder
The policyholder may be changed only at the time of Renewal of the
Policy. The new policyholder must be a member of the Insured Person’s
immediate family. Such change would be solely subject to Our
discretion and payment of premium by You. The renewed Policy shall
be treated as having been renewed without break.
The policyholder may be changed upon request in case of his demise,
his moving out of India or in case of divorce during the Policy Period.
E.II.4. NoConstructiveNotice
Any knowledge or information of any circumstance or condition in
relation to the Policyholder/ Insured Person which is in Our possession
andnotspecicallyinformedbythePolicyholder/InsuredPersonshall
not be held to bind or prejudicially affect Us notwithstanding
subsequent acceptance of any premium.
E.II.5. Geography
The geographical scope of this policy applies to events within India
other than for D.III.4.ii Worldwide Emergency Hospitalization with
Outpatient Cover under Freedom optional package (if opted) and
which are specically covered in the Policy Schedule. However all
admitted or payable claims shall be settled in India in Indian rupees.
E.II.6. Recordstobemaintained
You or the Insured Person, as the case may be shall keep an accurate
record containing all medical records pertaining to claim and shall allow
Us or our representative (s) to inspect such records. You or the Insured
Person as the case may be, shall furnish such information as may be
required by Us under this Policy at any time during the Policy Period
anduptothreeyearsafterthePolicyexpiration,oruntilnaladjustment
(if any) and resolution of all Claims under this Policy.
E.II.7. GracePeriod
The Policy may be renewed by mutual consent and in such event the
Renewal premium should be paid to Us on or before the date of expiry
ofthePolicyandinnocaselaterthantheGracePeriodof30daysfrom
the expiry of the Policy. We will not be liable to pay for any claim arising
out of an Injury/ Accident/ Condition that occurred during the Grace
Period. The provisions of Section 64VB of the Insurance Act shall be
applicable. All policies Renewed within the Grace Period shall be
eligible for continuity of cover.
E.II.8. RenewalTerms
a. The Policy is ordinarily renewable on mutual consent for life,
subject to application of Renewal and realization of Renewal
premium.The Policy with Freedom optional package shall be
renewed subject to the Insured Person being an Indian resident at
the time of renewal.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
b. We shall not be liable for any claim arising out of an ailment
suffered or Hospitalization commencing or disease/illness/condition
contracted during the period between the expiry of previous policy
and date of inception of subsequent policy.
c. Renewals will not be denied except on grounds of misrepresentation,
moral hazard, fraud, non-disclosure of material facts or non-
cooperation by You.
d. Where We have discontinued or withdrawn this product/plan You
will have the option to renewal under the nearest substitute Policy
being issued by Us, provided however benets payable shall be
subject to the terms contained in such other policy which has been
approved by IRDAI.
e. Insured Person shall disclose to Us in writing of any material
change in the health condition at the time of seeking Renewal of this
Policy, irrespective of any claim arising or made. The terms and
condition of the existing policy will not be altered.
f. We may, revise the Renewal premium payable under the Policy
or the terms of cover, provided that all such changes are approved
by IRDAI and in accordance with the IRDAI rules and regulations
as applicable from time to time. Renewal premium will not alter based
on individual claims experience. We will intimate You of any such
changes at least 90 days prior to date of such revision or
modication.
g. Alterations like increase/ decrease in Sum Insured or Change
in Plan/Product, addition/deletion of members, addition deletion
of Medical Condition existing prior to policy inception will be allowed
at the time of Renewal of the Policy. You can submit a request
forthechangesbyllingtheproposalformbeforetheexpiryofthe
Policy. We reserve Our right to carry out underwriting in relation
to acceptance of request for change of Sum Insured or addition/
deletion of members, addition deletion of Medical Condition
existing prior to policy inception, on renewal. The terms and
conditions of the existing policy will not be altered.
h. Any enhanced Sum Insured during any policy renewals will not
be available for an illness, disease, injury already contracted
under the preceding Policy Periods. All waiting periods as mentioned
below shall apply afresh for this enhanced limit from the effective
date of such enhancement.
i. Wherever the Sum Insured is reduced on any Policy Renewals,
the waiting periods as mentioned below shall be waived only up to
the lowest Sum Insured of the last 36/ 24 consecutive months as
applicable to the relevant waiting periods of the Plan opted.
j. Where an Insured Person is added to this Policy, either by way of
endorsement or at the time of renewal, all waiting periods under
Section E.I.1 to E.I.3 and E.II.1 and E.II.6 will be applicable
considering such Policy Year as the rst year of Policy with the
Company.
k. Applicable Cumulative Bonus shall be accrued on each renewal as
per eligibility under the plan opted.
l. Incaseofoaterpolicies,childrenattaining26yearsatthetimeof
renewal will be moved out of the oater into an individual
cover, however all continuity benets on the policy will remain
intact. Cumulative Bonus earned on the Policy will stay with the
oatercover.
III. YoumaypaythepremiumthroughNationalAutomatedClearing
House(NACH)/StandingInstruction(SI)providedthat
i. NACH/Standing Instruction Mandate form is completely lled &
signed by You.
ii. The Premium amount which would be auto debited & frequency of
instalmentisdulylledinthemandateform.
iii. NewMandateFormisrequiredtobelledincaseofanychange
in the Policy Terms and Conditions whether or not leading to
change in Premium.
iv. You need to inform us at least 15 days prior to the due date of
instalment premium if You wish to discontinue with the NACH/
Standing Instruction facility.
Non-payment of premium on due date as opted by You in the mandate
form subject to an additional renewal/ revival period will lead to
termination of the policy.
E.II.9. Premiumcalculation
Premium will be calculated based on the Sum Insured opted, Age,
gender,riskclassicationandZoneofCover.DefaultZoneofCoverwill
be based on Your City-Location based on Your correspondence
address. All Premiums are age based and will vary as per the change
in age group.
For premium calculation of oater policies, Age of eldest member
would be considered.
Premium towards D.III.1.i Maternity & New born baby Hospitalization
Expenses, D.III.3.i Maternity & New born baby Hospitalization
Expenses and D.IV.3 Infertility Treatment shall be applied to female
Insured Members covered as adult in the Policy.
Premium can be paid on Single, Half yearly, Quarterly and Monthly
basis. Premium payment mode can only be selected at the inception of
the Policy or at the renewal of the Policy.
In case of premium payment modes other than Single, a loading will be
applied on the premium.
Loading grid applicable for Half-yearly, Quarterly and Monthly payment
mode.
Premium payment mode %Loadingonpremium
Monthly 5.50
Quarterly 3.50
Half yearly 2.50
ZoneClassication
ZoneI: Mumbai, Thane & Navi Mumbai, Gujarat and Delhi & NCR
ZoneII: Bangalore, Hyderabad, Chennai, Chandigarh, Ludhiana, Kolkata,
Pune
ZoneIII: Rest of India excluding the locations mentioned under Zone I &
Zone II
IdenticationofZonewillbebasedonthelocation-Cityoftheproposed
Insured Persons.
(a) Persons paying Zone I premium can avail treatment all over India wit
out any Co-pay.
(b) Persons paying Zone II premium
i) Can avail treatment in Zone II and Zone III without any Co-pay.
ii) AvailingtreatmentinZoneIwillhavetobear10%ofeachand
every claim.
(c) Person paying Zone III premium
i) Can avail treatment in Zone III, without any Co-pay.
ii) AvailingtreatmentinZoneIIwillhavetobear10%ofeachand
every claim.
iii)AvailingtreatmentinZoneIwillhavetobear20%ofeachand
every claim.
***OptiontoselectZone1iftheactualZoneisZone2orZone3,and
would be available on payment of applicable premium at the time of
buying the First Policy and on subsequent renewals
Aforesaid Co-payments for claims occurring outside of the Zone will
not apply in case of Hospitalization due to Accident.
E.II.10.DiscountsunderthePolicy
You can avail of the following discounts on the premium on Your policy.
i. LifetimeDiscounts
a. EmployeeDiscount:10%discountonthepremium
b. Standing Instruction Discount: 3% discount on the renewal
premium, if the renewal premium is received through standing
instruction.
c. Long Term policy discount - Long term discount of 7.5% for
selectinga2yearpolicyand10%forselectinga3yearpolicy.This
discount is available only with ‘Single’ Premium Payment mode
d. Familydiscount: (Applicable only with cover on individual basis)
20%discountonthepremiumisapplicableforcovering2ormore
members under the same individual Policy.
ii. ShortTermDiscounts
a. ManipalCigna Existing Customer Discount: 5% discount will
be applicable to customers of ManipalCigna Insurance who
are already covered under Group / Retail Products. Discount
would be applicable once, only at inception and shall not be offered
to Portability/ Migration related proposals.
b. WorksiteMarketingDiscount–Adiscountof10%willbeavailable
on polices which are sourced through worksite marketing channel.
Discount would be applicable once only at inception of the Policy.
DiscountunderF.II.10.i(d)isapplicableonlytoindividualpolicies.All
other discounts mentioned above are available to both individual
aswellasoaterpolicies.Maximumdiscountinasinglepolicyshallnot
exceed40%.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
Family Discount, Long Term Discount and Worksite Marketing Discount
is applied on the total Policy premium which is sum total of individual
premium for Family policies.
E.II.11 Loadings&SpecialConditions
We may apply a risk loading on the premium payable (excluding
Statutory Levis and Taxes) or Special Conditions on the Policy
based upon the health status of the persons proposed for insurance
and declarations made in the Proposal Form. These loadings will
beappliedfrominceptiondateoftherstPolicyincludingsubsequent
Renewal(s) with Us. There will be no loadings based on individual
claims experience.
We may apply a specic sub-limit on a medical condition/ailment
depending on the past history and declarations or additional waiting
periods(amaximum of48monthsfrom thedateofinception ofrst
policy) on pre-existing diseases as part of the special conditions on the
Policy.
We shall inform You about the applicable risk loading or special
condition through a counter offer letter or through an electronic mode,
as the case may be and You would need to revert with consent and
additionalpremium(ifany),withinthedurationspeciedinthecounter
offer letter.
In case, You neither accept the counter offer nor revert to Us within the
duration specied, We shall cancel Your application and refund the
premium paid. Your Policy will not be issued unless We receive Your
consent.
E.II.12.Communications&Notices
Any communication or notice or instruction under this Policy shall be in
writing and will be sent to:
a. Thepolicyholder’s,attheaddressasspeciedinPolicySchedule
b. ToUs,attheaddressspeciedinthePolicySchedule.
c. No insurance agents, brokers, other person or entity is authorised
to receive any notice on the behalf of Us unless explicitly stated in
writing by Us.
d. Notice and instructions will be deemed served 10 days after
posting or immediately upon receipt in the case of hand delivery,
facsimile or e-mail.
E.II.13.ElectronicTransactions
You agree to comply with all the terms, conditions as We shall
prescribe from time to time, and conrms that all transactions
effected facilities for conducting remote transactions such as the
internet, World Wide Web, electronic data interchange, call centres,
tele-service operations (whether voice, video, data or combination
thereof) or by means of electronic, computer, automated machines
network or through other means of telecommunication, in respect of
this Policy, or Our other products and services, shall constitute legally
binding when done in compliance with Our terms for such facilities.
Sales through such electronic transactions shall ensure that all
conditions of Section 41 of the Insurance Act, 1938 prescribed for the
proposal form and all necessary disclosures on terms and conditions
and exclusions are made known to You. A voice recording in case of
tele-sales or other evidence for sales through the World Wide Web shall
be maintained and such consent will be subsequently validated /
conrmedbyYou.
All terms and conditions in respect of Electronic Transactions shall be
within the approved Terms and Conditions of the Policy.
E.II.14.LimitationofLiability
If a claim is rejected or partially settled and is not the subject of any
pending suit or other proceeding or arbitration, as the case may be,
within twelve months from the date of such rejection or settlement, the
claim shall be deemed to have been abandoned and Our liability shall
be extinguished and shall not be recoverable thereafter.
E.II.15.TermsandconditionsofthePolicy
The terms and conditions contained herein and in the Policy Schedule
shall be deemed to form part of the Policy and shall be read together as
one document.
E.II.16.DisputeResolution
Any and all disputes or differences under or in relation to this Policy
shall be determined by the Indian Courts and subject to Indian law
without reference to any principle which would result in the application
of the law of any other jurisdiction.
F. Othertermsandconditions
F.I. Claimprocess&management
F.I.1. ConditionPreceding
ThefullmentofthetermsandconditionsofthisPolicy(includingthe
realization of premium by their respective due dates) in so far as they
relate to anything to be done or complied with by You or any Insured
Person, including complying with the following steps, shall be the
condition precedent to the admissibility of the claim.
Completed claim forms and processing documents must be furnished
to Us within the stipulated timelines for all reimbursement claims.
Failure to furnish this documentation within the time required shall not
invalidate nor reduce any claim if You can satisfy Us that it was not
reasonably possible for You to submit / give proof within such time.
The due intimation, submission of documents and compliance with
requirements as provided under the Claims Process under this Section,
by You shall be essential failing which We shall not be bound to accept
a claim.
Cashless and Reimbursement Claim processing and access to
network hospitals is through our service partner/TPA, details of the
same will be available on the Health Card issued by Us as well as on
our website. For the latest list of network hospitals you can log on to
our website. Wherever a TPA is used, the TPA will only work to facilitate
claim processing. All customer contact points will be with Us including
claim intimation, submission, settlement and dispute resolutions.
F.I.2. PolicyHolder’s/InsuredPersonsDutyatthetimeofClaim
You are required to check the applicable list of Network Providers, at
Our website or call center before availing the Cashless services.
On occurrence of an event which may lead to a Claim under this Policy,
You shall:
(a)Forthwithintimate,leandsubmittheClaiminaccordancetothe
ClaimProceduredenedunderSectionG.I.3,G.I.4,andG.I.5as
mentioned below.
(b) If so requested by Us, You or the Insured Person must submit
himself/ herself for a medical examination by Our nominated
Medical Practitioner as often as We consider reasonable and
necessary. The cost of such examination will be borne by Us.
(c) Allow the Medical Practitioner or any of Our representatives to
inspect the medical and Hospitalization records, investigate the
facts and examine the Insured Person.
(d) Assist and not hinder or prevent Our representatives in pursuance
of their duties for ascertaining the admissibility of the claim, its
circumstances and its quantum under the provisions of the Policy.
F.I.3. ClaimIntimation
Upon the discovery or occurrence of any Illness / Injury that may give
rise to a Claim under this Policy, You / Insured Person shall undertake
the following:
In the event of any Illness or Injury or occurrence of any other
contingency which has resulted in a Claim or may result in a claim
covered under the Policy, You/the Insured Person, must notify Us either
at the call center or in writing, in the event of:
• Planned Hospitalization, You/the Insured Person will intimate such
admission at least 3 days prior to the planned date of admission.
• Emergency Hospitalization, You /the Insured Person will intimate
such admission within 48 hours of such admission.
The following details are to be provided to Us at the time of intimation
of Claim:
• Policy Number
• Name of the Policyholder
• Name of the Insured Person in whose relation the Claim is being
lodged
• Nature of Illness / Injury
• Name and address of the attending Medical Practitioner and
Hospital
• Date of Admission
• Any other information as requested by Us
F.I.4.CashlessFacility
Cashless facility is available only at our Network Hospital. The Insured
Person can avail Cashless facility at the time of admission into any

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
Network Hospital, by presenting the health card as provided by Us with
thisPolicy,alongwithavalidphotoidenticationproof(VoterIDcard/
Driving License / Passport / PAN Card / any other identity proof as
approved by Us).
(a) ForPlannedHospitalization:
i. The Insured Person should at least 3 days prior to admission to
the Hospital approach the Network Provider for Hospitalization for
medical treatment.
ii. The Network Provider will issue the request for authorization letter
for Hospitalization in the pre-authorization form prescribed by the
IRDA.
iii. The Network Provider shall electronically send the pre-
authorization form along with all the relevant details to the 24
(twenty four) hour authorization/cashless department along with
contact details of the treating Medical Practitioner and the Insured
Person.
iv. Upon receiving the pre-authorization form and all related medical
information from the Network Provider, We will verify the eligibility
of cover under the Policy.
v. Wherever the information provided in the request is sufcient to
ascertain the authorisation We shall issue the authorisation Letter
to the Network Provider. Wherever additional information or
documents are required We will call for the same from the Network
provider and upon satisfactory receipt of last necessary
documents the authorisation will be issued. All authorisations will
be issued within a period of 4 hours from the receipt of last
complete documents.
vi. The Authorisation letter will include details of sanctioned amount,
anyspeciclimitationontheclaim,anyco-paysordeductiblesand
non-payable items if applicable.
vii. The authorisation letter shall be valid only for a period of 15 days
from the date of issuance of authorization.
In the event that the cost of Hospitalization exceeds the authorized limit
as mentioned in the authorization letter:
i. The Network Provider shall request Us for an enhancement of
authorisation limit as described under Section G.I.4 (a) including
detailsofthespeciccircumstanceswhichhaveledtotheneedfor
increase in the previously authorized limit. We will verify the
eligibility and evaluate the request for enhancement on the
availability of further limits.
ii. We shall accept or decline such additional expenses within 24
(twenty-four) hours of receiving the request for enhancement from
You.
In the event of a change in the treatment during Hospitalization to the
Insured Person, the Network Provider shall obtain a fresh authorization
letter from Us in accordance with the process described under G.I.4 (a)
above.
At the time of discharge:
i. theNetworkProvidermayforwardanalrequestforauthorization
for any residual amount to us along with the discharge summary
and the billing format in accordance with the process described at
G.I.4 (a)above.
ii. Uponreceiptofthenalauthorisationletterfromus,Youmaybe
discharged by the Network Provider.
(b) IncaseofEmergencyHospitalization
i. The Insured Person may approach the Network Provider for
Hospitalization for medical treatment.
ii. The Network Provider shall forward the request for authorization
within 48 hours of admission to the Hospital as per the process
under Section G.I.4 (a).
iii. It is agreed and understood that we may continue to discuss the
Insured Person’s condition with the treating Medical Practitioner till
Our recommendations on eligibility of coverage for the Insured
Personarenalised.
iv. In the interim, the Network Provider may either consider treating
the Insured Person by taking a token deposit or treating him as per
their norms in the event of any lifesaving, limb saving, sight saving,
Emergency medical attention requiring situation.
v. The Network Provider shall refund the deposit amount to You
barring a token amount to take care of non-covered expenses
once the pre-authorization is issued.
Note: Cashless facility for Hospitalization Expenses shall be limited
exclusively to Medical Expenses incurred for treatment undertaken in
a Network Hospital for Illness or Injury which are covered under
the Policy and shall not be available to the Insured Person for coverage
under Daily Cash for Shared Accommodation (Section D.1.13),
Worldwide Emergency with Outpatient Cover under Freedom optional
package (Section D.III.4.ii). For all Cashless authorizations, You will, in
any event, be required to settle all non-admissible expenses, Co-
payment and / or Deductibles (if applicable), directly with the Hospital.
The Network Provider will send the claim documents along with the
invoice and discharge voucher, duly signed by the Insured Person
directly to us. The following claim documents should be submitted to
Us within 15 days from the date of discharge from Hospital -
• Claim Form Duly Filled and Signed
• Original pre-authorisation request
• Copy of pre-authorisation approval letter (s)
• CopyofPhotoIDofPatientVeriedbytheHospital
• Original Discharge/Death Summary
• Operation Theatre Notes (if any)
• Original Hospital Main Bill and break up Bill
• Original Investigation Reports, X Ray, MRI, CT Films, HPE
• Doctors Reference Slips for Investigations/Pharmacy
• Original Pharmacy Bills
• MLC/FIR Report/Post Mortem Report (if applicable and conducted)
We may call for any additional documents as required based on the
circumstances of the claim
There can be instances where We may deny Cashless facility for
Hospitalization due to insufcient Sum Insured or insufcient
information to determine admissibility in which case You/ Insured
Person may be required to pay for the treatment and submit the claim
for reimbursement to Us which will be considered subject to the Policy
Terms & Conditions.
We in our sole discretion, reserves the right to modify, add or restrict
any Network Hospital for Cashless services available under the Policy.
Before availing the Cashless service, the Policyholder / Insured Person
is required to check the applicable/latest list of Network Hospital on the
Company’s website or by calling our call centre.
F.I.5. ClaimReimbursementProcess
(a)CollectionofClaimDocuments
i. Wherever You have opted for a reimbursement of expenses, You
may submit the following documents for reimbursement of the
claimtoOurbranchorheadofceatyourownexpensenotlater
than 15 days from the date of discharge from the Hospital. You can
obtainaClaimFormfromanyofourBranchOfcesordownloada
copy from our website www.manipalcigna.com
ii. List of necessary claim documents to be submitted for
reimbursement are as following:
Claim form duly signed
Copy of photo ID of patient
Hospital Discharge summary
Operation Theatre notes
Hospital Main Bill
Hospital Break up bill
Investigation reports
Originalinvestigationreports,XRay,MRI,CTlms,HPE,ECG
Doctors reference slip for investigation
Pharmacy Bills
MLC/ FIR report, Post Mortem Report if applicable and conducted
KYC documents (Photo ID proof, address proof, recent passport
size photograph)
Cancelled cheque for NEFT payment
Payment receipt.
We may call for any additional documents/information as required
based on the circumstances of the claim.
iii. Our branch ofces shall give due acknowledgement of collected
documents to You.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
In case You/ Insured Person delay submission of claim documents
asspeciedinG.I.5.(a)above,theninadditiontothedocuments
mentioned in G.I.5.(a) above, You are also required to provide Us
the reason for such delay in writing. In case You delay submission
of claim documents, then in addition to the documents mentioned
above, You are also required to provide Us the reason for such
delay in writing. We will accept such requests for delay up to an
additional period of 30 days from the stipulated time for such
submission. We will condone delay on merit for delayed Claims
where the delay has been proved to be for reasons beyond Your
Insured Persons control.
where the delay has been proved to be for reasons beyond Your/
Insured Persons control.
F.I.6. ScrutinyofClaimDocuments
a. We shall scrutinize the claim and accompanying documents. Any
deciencyofdocumentsshallbeintimatedtoYouandtheNetwork
Provider, as the case may be within 5 days of their receipt.
b. Ifthedeciencyinthenecessaryclaimdocumentsisnotmetorare
partiallymetin10workingdaysoftherstintimation,Weshallremind
Youofthesameandevery10(ten)daysthereafter.
c. We will send a maximum of 3 (three) reminders.
d. We shall settle the claim payable amount arrived post scrutinizing the
claimdocumentsexcludingthedeciencyintimatedtoYou.
e. In case a reimbursement claim is received when a Pre-Authorization
letter has been issued, before approving such claim a check will be
made with the provider whether the Pre-authorization has been utilized
as well as whether the Policyholder has settled all the dues with the
provider. Once such check and declaration is received from the
Provider, the case will be processed.
F.I.7. ClaimAssessment
We will assess all admissible claims under the Policy in the following
progressive order -
(a) For Plans without Deductible Option
i) Where a room accommodation is opted for higher than the
eligible room category under the plan, the room rent for the
applicable accommodation will be apportioned on pro rata
basis. Such apportioned amount will apply to all “Associated
Medical Expenses”. [(a). Cost of Pharmacy & consumables,
(b). Cost of implant and medical device, (c). Cost of diagnostic
test,willnotbepartofAssociatedMedicalExpenses)]
ii) Any Sub-limits or Zonal Co-payment shall be applicable on the
amount payable after applying the Section G.I.7 a (i)
(b) For Plans with Deductible Option
i) Where a room accommodation is opted for higher than the
eligible room category under the plan, the room rent for the
applicable accommodation will be apportioned on pro rata
basis. Such apportioned amount will apply to all “Associated
Medical Expenses”. [(a). Cost of Pharmacy & consumables,
(b). Cost of implant and medical device, (c). Cost of diagnostic
test,willnotbepartofassociatedmedicalexpenses)]
ii) Arrived payable claim amount will be assessed against the
deductible.
iii) Any Sub-limits or Zonal Co-payment shall be applicable on the
amount payable after applying the Section G.I.7 b (i), (ii)
(c) The Claim amount assessed under Section G.I.7 a) and b) will be
deducted from the following amounts in the following progressive
order –
i) Deductible (if opted)
ii) Zonal Co-payment (if applicable)
iii) Sum Insured
iv) Cumulative Bonus or Cumulative Bonus Booster
v) Restored Sum Insured
ClaimAssessmentforBenetPlans:
WewillpayxedbenetamountsasspeciedinthePolicySchedule
in accordance with the terms of this Policy. We are not liable to make
any reimbursements of Medical Expenses or pay any other amounts
notspeciedinthePolicy.
ClaimassessmentforpolicieswithMonthly,QuarterlyandHalf-
YearlyPremiumPaymentMode:
In case of a claim (Cashless/Re-imbursement), an amount equivalent
to the balance of the instalment premiums payable, in that policy year,
would be recoverable from the admissible claim amount payable in
respect of the Insured person.
F.I.8. ClaimsInvestigation
We may investigate claims at Our own discretion to determine the
validity of claim. Such investigation shall be concluded within 15 days
from the date of assigning the claim for investigation and not later than
30 days from the date of receipt of last necessary document.
Verication carried out, if any, will be done by individuals or entities
authorisedbyUstocarryoutsuchverication/investigation(s)andthe
costsforsuchverication/investigationshallbebornebytheUs.
F.I.9. PreandPost-hospitalizationclaims
You should submit the Post-hospitalization claim documents at Your
own expense within 15 days of completion of Post-hospitalization
treatment or eligible post hospitalization period of cover, whichever is
earlier.
We shall receive Pre and Post- hospitalization claim documents either
along with the inpatient Hospitalization papers or separately and
process the same based on merit of the claim subject to Policy terms
and conditions, derived on the basis of documents received.
F.I.10. RepresentationagainstRejection:
Where a rejection is communicated by Us, You may if so desired within
15 days represent to Us for reconsideration of the decision.
F.I.11 PaymentTerms
The Sum Insured opted under the Plan shall be reduced by the amount
payable/paidundertheBenet(s)andthebalanceshallbeavailable
as the Sum Insured for the unexpired Policy Year.
If You/ Insured Person suffers a relapse within 45 days of the date of
discharge from the Hospital for which a claim has been made, then
such relapse shall be deemed to be part of the same claim and all the
limits for “Any One Illness” under this Policy shall be applied as if they
were under a single claim.
For Cashless Claims, the payment shall be made to the Network
Hospitalwhosedischargewouldbecompleteandnal.
For Reimbursement Claims, the payment will be made to you. In the
unfortunate event of Your death, We will pay the nominee (as named
in the Policy Schedule) and in case of no nominee to the Legal Heir who
holds a succession certicate or Indemnity Bond to that effect,
whichever is available and whose discharge shall be treated as full and
naldischargeofitsliabilityunderthePolicy.
ClaimprocessApplicabletothefollowingSections:
F.I.12 OutpatientExpenses
(a) Assessment of Claim Documents
We shall assess the claim documents and assess the admissibility
of claim subject to terms and conditions of the Policy.
(b) Settlement & Repudiation of a claim
Weshallsettleclaims,includingitsrejection,within5(ve)working
days of the receipt of the last ‘necessary’ document but not later
than30days.
ThisbenetshallbesettledonCashlessBasisonlyasmentionedin
G.I.4
F.I.13 DomesticSecondOpinion
(a) Receive Request for Expert Opinion on Critical Illness
You can submit Your request for an expert opinion by calling Our
call centre or register request through email.
(b) Facilitating the Process
We will schedule an appointment or facilitate delivery of Medical
Records of the Insured Person to a Medical Practitioner in India.
The expert opinion is available only in the event of the Insured
Person being diagnosed with covered Critical Illness.
F.I.14 HealthCheckupandTele-Consultation
(a) You or The Insured Person shall seek appointment by calling Our
call centre.
(b) We will facilitate Your appointment and We will guide You to the

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
nearest Network Provider for conducting the medical examination.
(c) Reports of the Medical Tests can be collected directly from the
centre.
F.I.15 WorldwideEmergencyHospitalizationwithOutpatientCover
a) In an unlikely event of You or the Insured Person requires
Emergency medical treatment outside India, You or Insured Person,
must notify Us either at Our call centre or in writing within 48 hours
of such admission.
b) YoushallleaclaimforreimbursementinaccordancewithSection
G.I.5 of the Policy.
F.I.16 Deductible
a) Any claim towards hospitalization during the Policy Period must
be submitted to Us for assessment in accordance with the claim
process laid down under Section G.I.4 and Section G.I.5 towards
cashless or reimbursement respectively in order to assess and
determine the applicability of the Deductible on such claim. Once
the claim has been assessed, if any amount becomes payable after
applying the deductible, We will assess and pay such claim in
accordance with Section G.I.6. and G.I.7.
b) Wherever such hospitalization claims as stated under G.I.16. a)
above is being covered under another Policy held by You, We will
assess the claim on available photocopies duly attested by Your
Insurer / TPA as the case may be.
F.I.17 SwitchOffandOnBenet
To Switch Off/On the Policy and other related documentation, You
our customer care centre at 1800-102-4462 as mentioned in Your
Policy Schedule.
F.I.18 HealthMaintenanceBenet
(a) Submission of claim
You can send the Health Maintenance Benet claim form along
with the invoices, treating Medical Practitioner’s prescription,
reports, duly signed by You / Insured Person as the case may
be,toOurbranchofceorHeadOfceatyourownexpense.The
Health Maintenance Benet under D.III.1 ‘Enhance’ optional
package can be claimed only once during the Policy Period up to
theextentoflimitunderthisbenet.
(b) Assessment of Claim Documents
We shall assess the claim documents and assess the admissibility
of claim subject to terms and conditions of the Policy .
(b) Settlement & Repudiation of a claim
Weshallsettleclaims,includingitsrejection,within5(ve)working
days of the receipt of the last ‘necessary’ document but not later
than30days.
F.I.19 ApplicationofMultiplepoliciesclause
In case this clause is invoked in accordance to the terms and conditions
as provided under this Policy, the Claim will be adjudicated as under:
a) Retail policy of the Company & any other Policy from other
insurers:
i) Cashless hospitalization: In case the Insured avail
Cashless Facility for Hospitalization then Insured / Hospital will
intimate us of the admission through a pre-authorization request
with all details & estimated amount for the Hospitalization. The
policyholder having multiple policies shall also have the right to
prefer claims from other policy/policies for the amounts
disallowed under the earlier chosen policy/policies, even if the
sum insured is not exhausted.Then the Insurer(s) shall settle
the claim subject to the terms and conditions of the other policy
/ policies so chosen. Post discharge, the hospital will send
all the original documents to one of the insurer & certied
copies of all documents to other insurers for settlement along
with authorization letter. The Company will evaluate the entire
bill & arrive at the total payable amount & deduct the amount
already settled by the other insurers & settle the difference
payable amount to the hospital as per AL issued.
ii) Reimbursement claim: In case the Insured gets
admitted&pays theentirebill &thenlesfor reimbursement
claim then he will have to intimate us of the admission 48
hours before admission for planned admissions & within 24
hours post hospitalization for emergency hospitalization but in
no case later than discharge from the Hospital. Insured will
need to submit details of the other insurance policies to the
Company. Post discharge insured will send all the original
documents along with bills & claim form to one of the insurer
&certiedcopiesofalldocuments&billsalongwithdulylled
claim form to the other insurers. The policyholder having
multiple policies shall also have the right to prefer claims from
other policy / policies for the amounts disallowed under the
earlier chosen policy / policies, even if the sum insured is not
exhausted. Then the Insurer (s) shall settle the claim subject to
the terms and conditions of the other policy / policies so chosen.
b) Retailpolicy&grouppolicyfromtheCompany:
i). Cashless process: In case the insured needs to utilize
cashless facility for hospitalization then the insured / hospital will
intimate the Company about the hospitalization through pre-
authorization process. The policyholder having multiple
policies shall also have the right to prefer claims from other
policy / policies for the amounts disallowed under the earlier
chosen policy / policies, even if the sum insured is not
exhausted. Then the Insurer(s) shall settle the claim subject to
the terms and conditions of the other policy / policies so chosen.
Post discharge hospital will send as many separate claims
as no of policies with the Company with attached authorization
letters & original documents with the 1st claim & copy of
documents with the other claims for settlement to the
Company. The Company will settle all the claims as per policy
terms & conditions & authorization letter issued.
ii). Reimbursement Claim process: In case the Insured gets
admitted&pays theentirebill &thenlesfor reimbursement
claim then he will have to intimate the Company of the
admission 48 hours before admission for planned admissions
& within 24 hours post hospitalization for emergency
hospitalization along with all the policy numbers.
Post discharge insured will send all original documents & bills
along with duly lled claim form. The policyholder having
multiple policies shall also have the right to prefer claims
from other policy / policies for the amounts disallowed under the
earlier chosen policy / policies, even if the sum insured is not
exhausted. Then the Insurer(s) shall settle the claim subject
to the terms and conditions of the other policy / policies so chosen.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
F.II .Annexure–I:
Ombudsman
NameoftheOfceofInsuranceOmbudsman State-wiseAreaofJurisdiction
AHMEDABAD
OfceoftheInsuranceOmbudsman,
Jeevan Prakash Building, 6
th
oor,
Tilak Marg, Relief Road,
Ahmedabad-380001.
Tel.:079-25501201/02/05/06
Email:- [email protected]
State of Gujarat and Union Territories of Dadra and Nagar Haveli and
Daman and Diu.
BENGALURU
OfceoftheInsuranceOmbudsman,
Jeevan Soudha Building, PID No. 57-27-N-19
Ground Floor, 19/19, 24
th
Main Road,
JP Nagar, 1
st
Phase,
Bengaluru-560078.
Tel.:080-26652048/26652049
Email:- [email protected]
State of Karnataka.
BHOPAL
OfceoftheInsuranceOmbudsman,
Janak Vihar Complex,
2
nd
Floor,6,MalviyaNagar,Opp.AirtelOfce,
Near New Market,
Bhopal-462003
Tel.:0755-2769201/202
Fax:0755-2769203
Email:- [email protected]
States of Madhya Pradesh and Chhattisgarh.
BHUBANESWAR
OfceoftheInsuranceOmbudsman,
62, Forest park,
Bhubaneshwar-751009.
Tel.:0674-2596461/2596455
Fax:0674-2596429
Email:- [email protected]
State of Orissa.
CHANDIGARH
OfceoftheInsuranceOmbudsman,
S.C.O.No.101,102&103,2
nd
Floor,
Batra Building, Sector 17 - D,
Chandigarh-160017.
Tel.:0172-2706196/6468
Fax:0172-2708274
Email:- [email protected]
States of Punjab, Haryana (excluding 4 districts viz Gurugram,
Faridabad, Sonepat and Bahadurgarh), Himachal Pradesh, Union
Territories of Jammu & Kashmir, Ladakh and Chandigarh.
CHENNAI
OfceoftheInsuranceOmbudsman,
Fatima Akhtar Court,
4
th
Floor, 453 (old 312), Anna Salai, Teynampet,
CHENNAI-600018.
Tel.:044-24333668/24335284
Fax:044-24333664
Email:- [email protected]
State of Tamil Nadu and Union Territories - Puducherry Town and
Karaikal (which are part of Union Territory of Puducherry).
DELHI
OfceoftheInsuranceOmbudsman,
2/2 A, Universal Insurance Building,
Asaf Ali Road,
NewDelhi-110002.
Tel.:011-23232481/23213504
Email:- [email protected]
Delhi, 4 Districts of Haryana viz. Gurugram, Faridabad, Sonepat and
Bahadurgarh.
GUWAHATI
OfceoftheInsuranceOmbudsman,
‘Jeevan Nivesh’, 5
th
Floor,
Nr. Panbazar over bridge, S.S. Road,
Guwahati-781001(ASSAM).
Tel.:0361-2132204/2132205
Email:- [email protected]
States of Assam, Meghalaya, Manipur, Mizoram, Arunachal Pradesh,
Nagaland and Tripura.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
HYDERABAD
OfceoftheInsuranceOmbudsman,
6-2-46, 1
st
oor,“MoinCourt”
Lane Opp. Saleem Function Palace,
A. C. Guards, Lakdi-Ka-Pool,
Hyderabad-500004.
Tel.:040-65504123/23312122
Fax:040-23376599
Email:- [email protected]
State of Andhra Pradesh, Telangana and Yanam - a part of Union
Territory of Puducherry.
JAIPUR
OfceoftheInsuranceOmbudsman,
Jeevan Nidhi - II Bldg., Gr. Floor,
Bhawani Singh Marg,
Jaipur-302005.
Tel.:0141-2740363
Email:- [email protected]
State of Rajasthan.
KOCHI
OfceoftheInsuranceOmbudsman,
2
nd
Floor,CC27/2603,PulinatBldg.,
Opp. Cochin Shipyard, M. G. Road,
Ernakulam-682015.
Tel.:0484-2358759/9338
Fax:0484-2359336
Email:- [email protected]
States of Kerala and Union Territory of (a) Lakshadweep (b) Mahe-a
part of Union Territory of Puducherry.
KOLKATA
OfceoftheInsuranceOmbudsman,HindustanBldg.Annexe,4,
C.R. Avenue, 4
th
Floor,KOLKATA-700072.
TEL.:033-22124340/22124339
Fax:033-22124341
Email:- [email protected]
States of West Bengal, Sikkim and Union Territories of Andaman &
Nicobar Islands.
LUCKNOW
OfceoftheInsuranceOmbudsman,
6
th
Floor, Jeevan Bhawan,
Phase-II, Nawal Kishore Road, Hazratganj,
Lucknow-226001.
Tel.:0522-2231330/1
Fax:0522-2231310
Email:- [email protected]
Districts of Uttar Pradesh
Lalitpur, Jhansi, Mahoba, Hamirpur, Banda, Chitrakoot, Allahabad,
Mirzapur, Sonbhadra, Fatehpur, Pratapgarh, Jaunpur,Varanasi,
Gazipur, Jalaun, Kanpur, Lucknow, Unnao, Sitapur, Lakhimpur,
Bahraich, Barabanki, Raebareli, Sravasti, Gonda, Faizabad, Amethi,
Kaushambi, Balrampur, Basti, Ambedkarnagar, Sultanpur, Maharajganj,
Santkabirnagar, Azamgarh, Kushinagar, Gorakhpur, Deoria, Mau,
Ghazipur, Chandauli, Ballia, Sidharthnagar.
MUMBAI
OfceoftheInsuranceOmbudsman,
3
rd
Floor, Jeevan Seva Annexe,
S. V. Road, Santacruz (W),
Mumbai-400054.
Tel.:022-26106552/6960
Fax:022-26106052
Email:- [email protected]
State of Goa and Mumbai Metropolitan Region excluding Areas of Navi
Mumbai and Thane.
NOIDA
OfceoftheInsuranceOmbudsman,
Bhagwan Sahai Palace
4
th
Floor, Main Road,
Naya Bans, Sector 15,
Distt: Gautam Buddh Nagar,
U.P-201301.
Tel.:0120-2514252/2514253
Email:- [email protected]
State of Uttaranchal and the districts of Uttar Pradesh:
Agra, Aligarh, Bagpat, Bareilly, Bijnor, Budaun, Bulandshehar, Etah,
Kanooj, Mainpuri, Mathura, Meerut, Moradabad, Muzaffarnagar,
Oraiyya, Pilibhit, Etawah, Farukkabad, Firozbad, Gautambodhanagar,
Ghaziabad, Hardoi, Shahjahanpur, Hapur, Shamli, Rampur, Kashganj,
Sambhal, Amroha, Hathras, Kanshiramnagar, Saharanpur.
PATNA
OfceoftheInsuranceOmbudsman,
1
st
Floor,Kalpana Arcade Building,
Bazar Samiti Road,
Bahadurpur,
Patna-800006.
Tel.:0612-2680952
Email:- [email protected]
States of Bihar and Jharkhand.
PUNE
OfceoftheInsuranceOmbudsman,
Jeevan Darshan Bldg., 3
rd
Floor,
C.T.S. No.s. 195 to 198,
N.C. Kelkar Road, Narayan Peth,
Pune-411030.
Tel.:020-41312555
Email:- [email protected]
State of Maharashtra, Areas of Navi Mumbai and Thane but excluding
Mumbai Metropolitan.

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
F.III.Annexure-II:
Title
Description
PleaserefertothePlanandSumInsuredyouhaveoptedtounderstandtheavailablebenetsunderyourplaninbrief
Your
Coverage
Details:
Identify your Plan Protect Advantage
BasicCover
This section
lists the Basic
benets
available on
your plan
Identify your Opted
Sum Insured (in `)
`3 Lacs, `4 Lacs, `5 Lacs, `7.5 Lacs,
`10Lacs,`12.5 Lacs, `15 Lacs,
`20Lacs,`25 Lacs, `30Lacs,`40Lacs,
`50Lacs,`100Lacs
`5 Lacs, `7.5 Lacs, `10Lacs,`12.5 Lacs, `15 Lacs,
`20Lacs,`25 Lacs, `30Lacs,`40Lacs,`50Lacs,`100
Lacs
Inpatient
Hospitalization
(When you are
hospitalized)
Room Rent: Covered up to Single Private A/C Room
For ICU - Covered up to Sum Insured
Thisbenetshallalsoofferthebelowcoversuptothelimitsmentioned:
a. Listed Modern and Advanced Treatments:
For Sum Insured <`5Lacs:Upto50%ofSumInsured
ForSumInsured>=`5 Lacs: Up to Sum Insured
b. HIV/AIDS & STD:
Up to Sum Insured
c. Mental Illness
Up to Sum Insured
For ICD Codes mentioned below: Waiting Period of 24 months shall apply
ICD 10
CODES
DISEASES
F05 Delirium due to known physiological condition
F06 Other mental disorders due to known physiological condition
F07 Personality and behavioural disorders due to known physiological condition
F10 Alcohol related disorders
F20 Schizophrenia
F23 Brief psychotic disorders
F25 Schizoaffective disorders
F29
Unspeciedpsychosisnotduetoasubstanceorknownphysiological
condition
F31 Bipolar disorder
F32 Depressive episode
F39 Unspeciedmood[affective]disorder
F40 Phobic Anxiety disorders
F41 Other Anxiety disorders
F42 Obsessive-compulsive disorder
F44 Dissociative and conversion disorders
F45 Somatoform disorders
F48 Other nonpsychotic mental disorders
F60 Specicpersonalitydisorders
F84 Pervasive developmental disorders
F90 Attention-decithyperactivitydisorders
F99 Mentaldisorder,nototherwisespecied
Pre-hospitalization MedicalExpensesCoveredupto60daysbeforethedateofhospitalization;CoveredUptotheSumInsured
Post-
hospitalization
MedicalExpensesCoveredupto180dayspostdischargefromthehospital;CoveredUptotheSum
Insured
Day Care
Treatment
Covered up to the Sum Insured
Domiciliary
Hospitalization
(Treatment at Home)
Coveredupto10%oftheSumInsured
PreandPostHospitalizationExpenses:30dayseach
Road Ambulance
(Reimbursement of
Ambulance Expenses)
Covered up to the Sum Insured
Donor Expenses
(Hospitalization
Expenses of the donor
providing the organ)
Covered up to the Sum Insured

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
Restoration of Sum
Insured
(When opted Sum
Insuredisinsufcient
due to claims)
Multiple Restoration is available in a Policy Year for all illnesses, whether unrelated or same, in addition to
the Sum Insured
Applicable for below covers only
1. D.I.1 - In-patient Hospitalization (Except for Bariatric Surgery)
2. D.I.2 - Pre - hospitalization
3. D.I.3 - Post - hospitalization
4. D.I.4 - Day Care Treatment
5. D.I.6 - Road Ambulance
6. D.I.7 - Donor Expenses
7. D.I.9 - AYUSH Treatment
8. D.IV.1 – Non-Medical Items
Restoration shall not get triggered for the 1
st
claim
The maximum liability under a single claim shall not be more than Base Sum Insured + Cumulative Bonus +
Restored Sum Insured
AYUSH Treatment (In-
patient Hospitalization)
Covered up to the Sum Insured
Air Ambulance Cover
Covered up to sum insured subject to maximum of `10LacsinadditiontotheSumInsuredforexpenses
incurred on Air Ambulance
Bariatric Surgery
Cover
Covered up to the Sum Insured opted subject to maximum of `5 Lacs Waiting Period of 36 months shall
apply for Bariatric Surgery
Outpatient Expenses Not Available
Option to choose from - `20,000,`30,000,`50,000Per
policy Year
Can be used to pay for Consultations and Diagnostics
includingDentalandVision:Upto100%oftheSumInsured
optedforOutpatientbenet.
Upto20%oftheOutpatientLimitcanbeusedforPharmacy
(Drugs and Medicines prescribed by Medical Practitioners).
Thisbenetisavailableonlyoncashlessbasisfromthe
Network providers of ManipalCigna Health Insurance
Company Limited.
Anyunutilizedamountunderthisbenetshallnotbecarried
forward to subsequent Policy Year.
Daily Cash for Shared
Accommodation
DailyCashbenetforoccupyingsharedaccommodationwhilehospitalized,shallbe
covered as below:-
a. For Sum Insured up to `10Lacs:`800perdayuptomaximumof`5,600
b. For Sum Insured above `10Lacs:`1,000perdayuptomaximumof`7,000
Payable for each continuous and completed 24 Hours of Hospitalization during the
Policy Year
Thisbenetgetstriggeredpost48hoursofIn-patienthospitalizationandshallbepayablefrom1stday
onwards.
ValueAdded
Covers
This section
lists the
additional
value added
benetsthat
are available
along with
your plan
Health Check Up
Availableeachpolicyyear(includingtherstyear),toallAdultinsuredpersonswhohavecompleted18
years of Age.
• For Sum Insured Up to `5 lacs: Package 1 subject to a maximum of Up to `1000per
adult member
• For Sum Insured above `5 lacs and Up to `10lacs:Package2subjecttoamaximum
of Up to `2500peradultmember
• For Sum Insured above `10lacs:Package3subjecttomaximumofUpto`5000per
adult member
Annually from 1
st
year onwards
The packages shall be offered on cashless basis only. However, the eligible insured may avail any health
checkfromtheMCHINetworkofHealthCheckUpCenterUptothelimitspecied
Domestic Second
Opinion
Available for 36 listed Critical Illnesses
Tele-Consultation Unlimited Tele-consultation during the Policy Year
Cumulative Bonus
Aguaranteedbonusof25%ofSumInsuredforeverycompletedPolicyYear,subjecttoamaximum
accumulationupto200%oftheSumInsured.
SwitchOffBenet
The Policy can be Switched Off, after one year, any time during the Policy Year except for Personal Accident
Cover, Worldwide Emergency Hospitalization with Outpatient Cover under Freedom optional package and
Critical Illness Add-On cover, if opted, in case you/ Insured Person travel out of India, for a period maximum
upto30days.
Thisbenetshallnotbeavailableforthelast90daysofthePolicyYear.
Premium discount shall be calculated on pro-rated basis if Policy is switched off due to Insured Person (in
individualpolicy)orallInsuredPersons(underoaterpolicy)travellingoutofIndiaandthisdiscountshallbe
adjusted in the renewal premium falling due immediately after the expiring Policy Period.
The Policy will reactivate the cover Switch-On on the requested date of Switch On as intimated to Us by
You/ Insured Person.
TheoptiontoSwitchOffthecovershallbeavailableonlyonceinapolicyyearandUptoamaximumof30
days at a stretch. This shall not deactivate the following cover, if opted:
1. Worldwide Emergency Hospitalization with Outpatient Cover under Freedom
optional package
2. Personal Accident Cover
3. Critical Illness Add-on

ManipalCigna ProHealth Prime | Protect Plan and Advantage Plan | Terms & Conditions | UIN: MCIHLIP22224V012122 | April 2022
Optional
Packages
This section
lists the
available
optional
packages
under your
plan and the
limits under
each of these
options.
The limits
specied
under these
optional
packages
shall override
the applicable
limits
mentioned as
part of base
cover for the
respective
coverages.
Enhance Plus
1. Maternity & New Born Hospitalization Expenses
a. Maternity Cover (up to maximum 2 deliveries or terminations) -
Coveredupto10%ofSumInsuredOptedsubjecttoa
maximum
of `1 Lac in addition to the Sum Insured opted
b. New Born Baby -
Coverage for the In-patient hospitalization expenses of a new
born up to the limit provided under Maternity Expenses
c. First Year Vaccination
Covered as per national immunization program, up to the limit
provided under Maternity Expenses
Not Available
2. Room Accommodation upgrade
The Insured Person shall be eligible to upgrade the
room type category eligibility under the Policy to “Any
Room Category” in a Hospital.
3. Health Maintenance Benefit
Up to `3000perPolicyYear.
Reimbursement of the Reasonable and Customary Charges
incurred
by the Insured Person for Medically Necessary charges incurred
during the Policy Year on an Out Patient basis for:
i. Consultation with Medical Practitioner, Diagnostic tests,
preventive tests, drugs, prosthetics, medical aids (spectacles
and contact lenses, hearing aids, crutches, wheel chair, walker,
walking stick, lumbo-sacral belt), prescribed by the specialist
Medical Practitioner.
ii. Towards Dental Treatments and AYUSH forms of Medicines
wherever prescribed by a Medical Practitioner.
Assure (Applicable for
Sum Insured `3 Lacs,
`4 Lacs and `5 Lacs)
i. Room Accommodation Limit
RoomRent-Upto1%ofSumInsuredperday.
ICU-Upto2%ofSumInsuredperday.
ii. Disease Specific Sub-limits
Sum Insured (In `) `3 and `4 Lacs `5 Lacs
Treatment for each Ailment/
Procedure mentioned below:
1. Surgery for treatment of all
types of Hernia
2. Hysterectomy
3. Surgeries for benign
Prostate Hypertrophy
4. Surgical treatment of stones
of renal system
`50,000 `65,000
Treatment of Cataract (Per
Eye)
`20,000 `30,000
Treatment of Total Knee
replacement (Per knee)
`80,000 `1,00,000
Treatment for breakage of
bones
`2,00,000 `2,50,000
iii. Modern and Advanced Treatments
CoveredUpto10%ofSumInsured
Wellness Program
RewardscanbeearnedbycompletingactivitiesspeciedunderOurHealthyLifeManagementProgramup
tomaximumof20%ofexpiringbasePremium(excludingPremiumforoptionalcovers,Riderandtaxes).
These earned Reward Points can be used against payable Renewal premium (excluding Premium for
optional covers, Rider and taxes) as discount from 1
st
Renewal of the Policy.
Carry forward of earned Reward Points shall not be allowed.
Discount from Network
Provider
Discount on Pharmacy, Diagnostics and Health Supplements, offered by the Network Providers of
ManipalCigna Health Insurance Company Limited
Premium Waiver
Benet
Waives off one year Policy Premium (including optional covers, rider and taxes) upon occurrence of any
of the listed contingencies (Accidental death/ listed Critical Illnesses) to the Policyholder who is also an
Insured Person in the Policy

ManipalCignaProHealthPrime|ProtectPlanandAdvantagePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Enhance Not Available
1. Maternity & New Born
Hospitalization Expenses
a. Maternity Cover (up to
maximum 2 deliveries or
terminations) -
Coveredupto10%of
Sum Insured Opted
subject to a maximum
of `1 Lac in addition to
the Sum Insured opted
b. New Born Baby -
Coverage for the In-
patient hospitalization
expenses of a new born
up to the limit provided
under Maternity
Expenses
c. First Year Vaccination
Covered as per national
immunization program,
up to the limit provided
under Maternity
Expenses
2. Room Accommodation
upgrade
The Insured Person
shall be eligible to
upgrade the room type
category eligibility under
the Policy to “Any Room
Category” in a Hospital.
Freedom (Applicable
to Indian Residents
only)
1. Room Accommodation upgrade
The Insured Person shall be eligible to upgrade the room type category eligibility under the Policy to “Any
Room Category” in a Hospital.
2. Worldwide Emergency Hospitalization with Outpatient Cover
Covered up to Sum Insured opted for Emergency In-patient Hospitalization or Emergency Outpatient
outside India.
AnyclaimpayableunderthisbenetisoverandabovetheSumInsured.
Optional
Covers
This section
lists the
available
optional
covers under
your plan
and the limits
under each of
these options
Non-Medical Items
Non-Medical items covered up to Sum Insured opted in case of In-patient Hospitalization and/or Day Care
Treatment
Deductible
Deductible of `10,000or`25,000canbeoptedattheinceptionor
during any Renewal of the Policy.
For Deductible of `10,000,thecovercanberemovedatthetimeof
Policy Renewal.
For Deductible of `25,000,theInsuredPersoncanremovethe
deductible of `25,000onlyatthetimeofrenewalfallingimmediately
due after 4 continuous Policy Years or any subsequent renewals
thereon, from the year of opting `25,000deductible
Thisbenetwillnotbeavailableif‘Assure’optionalpackageisopted
Not Available
Infertility Treatment
Infertility Cover (Available if D.III.1 ‘Enhance Plus’ or D.III.3 ‘Enhance’ optional package is opted and for
`7.5 Lacs and above Sum Insured options)
Covered for Infertility Expenses up to `2.5 Lacs in addition to Maternity Sum Insured under Maternity
Cover.
Waiting period of 36 months shall apply for this cover.
Maximum upto 2 successful procedures shall be covered during the lifetime of the eligible Insured Person
and the coverage shall terminate thereafter.
ThecovershallautomaticallyceaseupontheeligibleInsuredPersonattaining60yearsofage.
Personal Accident
Cover
LumpsumbenetequaltotwotimesofSumInsuredsubjecttoamaximumof`50Lacsincaseof
Accidental Death or Permanent Total Disablement of Insured Member due to accident.
Cumulative Bonus
booster
Aguaranteedbonusof50%increaseinSumInsuredperPolicyYearirrespectiveofclaims,subjecttoa
maximumaccumulationupto200%oftheSumInsured.
ThisbenetisapplicableforSumInsuredoptedfor`5 lacs and above.
OptingforthisBenetwillreplacetheCumulativeBonusintheBaseCover.
Addoncover
(Rider)
This section
lists the Add
on cover
available
under your
plan
ManipalCigna Critical
Illness Add On Cover
Lumpsumpaymentofanadditional100%ofSumInsuredOpted.

ManipalCignaProHealthPrime|ProtectPlanandAdvantagePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
F.IV.Annexure-lII
ListI-ItemsforwhichCoverageisnotavailableinthePolicy
Sl.
No.
Item
1. BABY FOOD
2. BABY UTILITIES CHARGES
3. BEAUTY SERVICES
4. BELTS / BRACES
5. BUDS
6. COLD PACK / HOT PACK
7. CARRY BAGS
8. EMAIL I INTERNET CHARGES
9. FOOD CHARGES (OTHER THAN PATIENT’s DIET PROVIDED
BY HOSPITAL)
10. LEGGINGS
11. LAUNDRY CHARGES
12. MINERAL WATER
13. SANITARY PAD
14. TELEPHONE CHARGES
15. GUEST SERVICES
16. CREPE BANDAGE
17. DIAPER OF ANY TYPE
18. EYELET COLLAR
19. SLINGS
20. BLOOD GROUPING AND CROSS MATCHING OF DONORS
SAMPLES
21. SERVICE CHARGES WHERE NURSING CHARGE ALSO
CHARGED
22. TELEVISION CHARGES
23. SURCHARGES
24. ATTENDANT CHARGES
25. EXTRA DIET OF PATIENT (OTHER THAN THAT WHICH
FORMS PART OF BED CHARGE)
26. BIRTH CERTIFICATE
27. CERTIFICATE CHARGES
28. COURIER CHARGES
29. CONVEYANCE CHARGES
30. MEDICAL CERTIFICATE
31. MEDICAL RECORDS
32. PHOTOCOPIES CHARGES
33. MORTUARY CHARGES
34. WALKING AIDS CHARGES
35. OXYGEN CYLINDER (FOR USAGE OUTSIDE THE
HOSPITAL)
36. SPACER
37. SPIROMETRE
38. NEBULIZER KIT
39. STEAM INHALER
40. ARMSLING
41. THERMOMETER
42. CERVICAL COLLAR
43. SPLINT
44. DIABETIC FOOT WEAR
45. KNEE BRACES (LONG / SHORT / HINGED)
46. KNEE IMMOBILIZER / SHOULDER IMMOBILIZER
47. LUMBO SACRAL BELT
48. NIMBUS BED OR WATER OR AIR BED CHARGES
49. AMBULANCE COLLAR
50. AMBULANCE EQUIPMENT
51. ABDOMINAL BINDER
52. PRIVATE NURSES CHARGES - SPECIAL NURSING
CHARGES
53. SUGAR FREE Tablets
54. CREAMS POWDERS LOTIONS (Toiletries are not payable,
only prescribed medical pharmaceuticals payable)
55. ECG ELECTRODES
56. GLOVES
57. NEBULISATION KIT
58. ANYKITWITHNODETAILSMENTIONED[DELIVERYKIT,
ORTHOKIT,RECOVERYKIT,ETC]
59. KIDNEY TRAY
60. MASK
61. OUNCE GLASS
62. OXYGEN MASK
63. PELVIC TRACTION BELT
64. PAN CAN
65. TROLLY COVER
66. UROMETER, URINE JUG
67. AMBULANCE
68. VASOFIX SAFETY
ListII-ItemsthataretobesubsumedintoRoomCharges
SI.
No.
Item
1. BABY CHARGES (UNLESS SPECIFIED / INDICATED)
2. HAND WASH
3. SHOE COVER
4. CAPS
5. CRADLE CHARGES
6. COMB
7. EAU-DE-COLOGNE I ROOM FRESHNERS
8. FOOT COVER
9. GOWN
10. SLIPPERS
11. TISSUE PAPER
12. TOOTH PASTE
13. TOOTH BRUSH
14. BED PAN
15. FACE MASK
16. FLEXI MASK
17. HAND HOLDER
18. SPUTUM CUP
19. DISINFECTANT LOTIONS
20. LUXURY TAX
21. HVAC
22. HOUSE KEEPING CHARGES
23. AIR CONDITIONER CHARGES
24. IM IV INJECTION CHARGES

ManipalCignaProHealthPrime|ProtectPlanandAdvantagePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
ManipalCignaProHealthPrime|ProtectPlanandAdvantagePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
25. CLEAN SHEET
26. BLANKET / WARMER BLANKET
27. ADMISSION KIT
28. DIABETIC CHART CHARGES
29. DOCUMENTATION CHARGES I ADMINISTRATIVE
EXPENSES
30. DISCHARGE PROCEDURE CHARGES
31. DAILY CHART CHARGES
32. ENTRANCE PASS I VISITORS PASS CHARGES
33. EXPENSES RELATED TO PRESCRIPTION ON DISCHARGE
34. FILE OPENING CHARGES
35. INCIDENTAL EXPENSES I MISC. CHARGES (NOT
EXPLAINED)
36. PATIENT IDENTIFICATION BAND I NAME TAG
37. PULSEOXYMETER CHARGES
ListIII-ItemsthataretobesubsumedintoProcedureCharges
1. HAIR REMOVAL CREAM
2. DISPOSABLES RAZORS CHARGES (for site preparations)
3. EYE PAD
4. EYE SHEILD
5. CAMERA COVER
6. DVD, CD CHARGES
7. GAUSE SOFT
8. GAUZE
9. WARD AND THEATRE BOOKING CHARGES
10. ARTHROSCOPY AND ENDOSCOPY INSTRUMENTS
11. MICROSCOPE COVER
12. SURGICAL BLADES, HARMONICSCALPEL, SHAVER
13. SURGICAL DRILL
14. EYE KIT
15. EYE DRAPE
16. X-RAY FILM
17. BOYLES APPARATUS CHARGES
18. COTTON
19. COTTON BANDAGE
20. SURGICAL TAPE
21. APRON
22. TORNIQUET
23. ORTHOBUNDLE, GYNAEC BUNDLE
ListIV-Itemsthataretobesubsumedintocostsoftreatment
SI.
No.
Item
1. ADMISSION / REGISTRATION CHARGES
2. HOSPITALIZATION FOR EVALUATION / DIAGNOSTIC
PURPOSE
3. URINE CONTAINER
4. BLOOD RESERVATION CHARGES AND ANTE NATAL
BOOKING CHARGES
5. BIPAP MACHINE
6. CPAP / CAPO EQUIPMENTS
7. INFUSION PUMP - COST
8. HYDROGEN PEROXIDE \SPIRIT \ DISINFECTANTS ETC
9. NUTRITION PLANNING CHARGES - DIETICIAN
CHARGES - DIET CHARGES
10. HIV KIT
11. ANTISEPTIC MOUTHWASH
12. LOZENGES
13. MOUTH PAINT
14. VACCINATION CHARGES
15. ALCOHOL SWABES
16. SCRUB SOLUTIONISTERILLIUM
17. GLUCOMETER & STRIPS
18. URINE BAG

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
A. Preamble
This is a legal contract between You and Us subject to the receipt of full
premium, Disclosure to Information Norm including the information
provided by You in the Proposal Form and the terms, conditions and
exclusions of this Policy.
If any Claim arising as a result of a Disease/Illness or Injury that
occurred during the Policy Period becomes payable, then We shall pay
thebenetsinaccordancewithterms,conditionsandexclusionsofthe
Policy subject to availability of Sum Insured and Cumulative Bonus (if
any). All limits mentioned in the Policy Schedule are applicable for each
Policy Year of coverage.
B. Denitions
B.I. StandardDenitions
1. Accident means a sudden, unforeseen and involuntary event caused
by external, visible and violent means.
2. Any one Illness means continuous Period of illness and it includes
relapse within 45 days from the date of last consultation with the
Hospital/Nursing Home where the treatment was taken.
3. AYUSH Hospital is a healthcare facility wherein medical/ surgical/
para-surgical treatment procedures and interventions are carried out
by AYUSH Medical Practitioner (s) comprising any of the following:
a) Central or State Government AYUSH Hospital; or
b) Teaching hospitals attached to AYUSH College recognized by the
Central Government / Central Council of Indian Medicine / Central
Council for Homeopathy; or
c) AYUSH Hospital, standalone or co-located with in-patient
healthcare facility of any recognized system of medicine,
registered with the local authorities, wherever applicable, and is
under the supervision of a qualied registered AYUSH Medical
Practitioner and must comply with all the following criterion:
i) Havingatleastvein-patientbeds;
ii) Having qualiedAYUSHMedicalPractitioner inchargeround
the clock;
iii) Having dedicated AYUSH therapy sections as required and/
or has equipped operation theatre where surgical procedures
are to be carried out;
iv) Maintaining daily record of the patients and making them
accessible to the insurance company’s authorized
representative.
4. Cashless Facility means a facility extended by the insurer to the
insured where the payments, of the costs of treatment undergone by
the insured in accordance with the Policy terms and conditions, are
directly made to the network provider by the insurer to the extent
pre-authorization approved.
5. Co-payment means a cost-sharing requirement under a health
insurance policy that provides that the policyholder/insured will bear a
specied percentage of the admissible claim amount.A co-payment
does not reduce the Sum Insured.
6. ConditionPrecedent means a policy term or condition upon which the
Insurer’s Liability under the Policy is conditional upon.
7. CongenitalAnomaly refers to a condition(s) which is present since
birth, and which is abnormal with reference to form, structure or
position.
a. Internal Congenital Anomaly - which is not in the visible and
accessible parts of the body is called Internal Congenital Anomaly
b. ExternalCongenitalAnomaly - Congenital Anomaly which is in the
visible and accessible parts of the body.
8. CriticalIllness means the following:
a) CancerofSpeciedSeverity
A malignant tumour characterised by the uncontrolled growth & spread
of malignant cells with invasion & destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy.
The term cancer includes leukemia, lymphoma and sarcoma.
The following are excluded –
i. All tumors which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant
potential, neoplasm of unknown behavior, or non-invasive,
including but not limited to: Carcinoma in situ of breasts, Cervical
dysplasia CIN-1, CIN -2 and CIN-3.
ii. Any non-melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. Alltumorsoftheprostateunlesshistologicallyclassiedashaving
a Gleason score greater than 6 or having progressed to at least
clinicalTNMclassicationT2N0M0.
v. All Thyroid cancers histologically classied as T1N0M0 (TNM
Classication)orbelow;
vi. Chronic lymphocytic leukaemia less than RAI stage 3
vii. Non-invasive papillary cancer of the bladder histologically
describedasTaN0M0orofalesserclassication,
viii.All Gastro-Intestinal Stromal Tumors histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of
lessthanorequalto5/50HPFs;
ix. All tumors in the presence of HIV infection.
b) MyocardialInfarction(FirstHeartAttackofSpecicSeverity)
I The rst occurrence of heart attack or myocardial infarction, which
means the death of a portion of the heart muscle as a result of
inadequate blood supply to the relevant area. The diagnosis for this will
be evidenced by all of the following criteria:
i. a history of typical clinical symptoms consistent with the diagnosis
of Acute Myocardial Infarction (for e.g. typical chest pain)
ii. new characteristic electrocardiogram changes
iii. elevationofinfarctionspecicenzymes,Troponinsorotherspecic
biochemical markers.
II The following are excluded:
i. Other acute Coronary Syndromes
ii. Any type of angina pectoris.
iii. A rise in cardiac biomarkers or Troponin T or I in absence of overt
ischemic heart disease OR following an intra-arterial cardiac
procedure.
c) OpenChestCABG
I The actual undergoing of heart surgery to correct blockage ornarrowing
in one or more coronary artery (s), by coronary artery bypass grafting
done via a sternotomy (cutting through the breast bone) or minimally
invasive keyhole coronary artery bypass procedures. The diagnosis
must be supported by a coronary angiography and the realisation of
surgeryhastobeconrmedbyacardiologist.
II The following are excluded:
a. Angioplasty and/or any other intra-arterial procedures
d) OpenHeartReplacementorRepairofHeartValves
The actual undergoing of open-heart valve surgery is to replace or
repair one or more heart valves, as a consequence of defects in,
abnormalities of, or disease-affected cardiac valve (s). The diagnosis of
the valve abnormality must be supported by an echocardiography and
therealizationofsurgeryhastobeconrmedbyaspecialistmedical
practitioner. Catheter based techniques including but not limited to,
balloon valvotomy/valvuloplasty are excluded.
e) ComaofSpeciedSeverity
1. A state of unconsciousness with no reaction or response to external
stimuli or internal needs.
PolicyContract
Plans:Active
MANIPALCIGNAPROHEALTHPRIME

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
This diagnosis must be supported by evidence of all of the following:
i. no response to external stimuli continuously for at least 96 hours;
ii. life support measures are necessary to sustain life; and
iii. permanentneurologicaldecitwhichmustbeassessedatleast30
days after the onset of the coma.
2. Theconditionhastobeconrmedbyaspecialistmedicalpractitioner.
Coma resulting directly from alcohol or drug abuse is excluded.
f) KidneyFailureRequiringRegularDialysis
End stage renal disease presenting as chronic irreversible failure of
both kidneys to function, as a result of which either regular renal
dialysis (haemodialysis or peritoneal dialysis) is instituted or renal
transplantation is carried out. Diagnosis has to be conrmed by a
specialist medical practitioner.
g) StrokeResultinginPermanentSymptoms
Any cerebrovascular incident producing permanent neurological
sequelae. This includes infarction of brain tissue, thrombosis in an
intracranial vessel, haemorrhage and embolization from an extra
cranialsource.Diagnosishastobeconrmedbyaspecialistmedical
practitioner and evidenced by typical clinical symptoms as well as
typicalndingsinCTScanorMRIofthebrain.Evidenceofpermanent
neurologicaldecitlastingforatleast3monthshastobeproduced.
The following are excluded:
1. Transient ischemic attacks (TIA)
2. Traumatic injury of the brain
3. Vascular disease affecting only the eye or optic nerve or vestibular
functions.
h) MajorOrgan/BoneMarrowTransplant
The actual undergoing of a transplant of:
1. One of the following human organs: heart, lung, liver, kidney,
pancreas, that resulted from irreversible end-stage failure of the
relevant organ, or
2. Human bone marrow using haematopoietic stem cells. The
undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
i. Other stem-cell transplants
ii. Where only islets of langerhans are transplanted
i) PermanentParalysisofLimbs
Total and irreversible loss of use of two or more limbs as a result of
injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be permanent
with no hope of recovery and must be present for more than 3 months.
j) MotorNeuronDiseasewithPermanentSymptoms
Motor neuron disease diagnosed by a specialist medical practitioner as
spinal muscular atrophy, progressive bulbar palsy, amyotrophic lateral
sclerosis or primary lateral sclerosis. There must be progressive
degeneration of corticospinal tracts and anterior horn cells or bulbar
efferent neurons. There must be current signicant and permanent
functional neurological impairment with objective evidence of motor
dysfunction that has persisted for a continuous period of at least
3 months.
k) MultipleSclerosiswithPersistingSymptoms
I. TheunequivocaldiagnosisofDeniteMultipleSclerosisconrmedand
evidenced by all of the following:
i. investigations including typical MRI ndings which unequivocally
conrmthediagnosistobemultiplesclerosisand
ii. there must be current clinical impairment of motor or sensory
function, which must have persisted for a continuous period of
at least 6 months.
II. Other causes of neurological damage such as SLE and HIV are
excluded.
9. CumulativeBonus
Cumulative Bonus means any increase in the Sum Insured granted by
the insurer without an associated increase in premium.
10. DayCareCentre- A day care centre means any institution established
for day care treatment of illness and / or injuries or a medical set - up
within a hospital and which has been registered with the local
authorities, wherever applicable, and is under the supervision of a
registeredandqualiedmedicalpractitionerANDmustcomplywithall
minimum criteria as under:-
a. hasqualiednursingstaffunderitsemployment
b. hasqualiedmedicalpractitioner(s)incharge
c. has a fully equipped operation theatre of its own where surgical
procedures are carried out
d. maintains daily records of patients and will make these accessible
to the Insurance company’s authorized personnel.
11. Day Care Treatment means medical treatment, and/or surgical
procedure which is:
i) Undertaken under General or Local Anesthesia in a hospital/day
care centre in less than 24 hrs because of technological
advancement, and
ii) Which would have otherwise required a Hospitalization of more
than 24 hours.
Treatment normally taken on an out-patient basis is not included in
thescopeofthisdenition.
12. Deductible means a cost-sharing requirement under a health
insurance policy that provides that the Insurer will not be liable for a
speciedrupeeamountincaseofindemnitypoliciesandforaspecied
number of days/hours in case of hospital cash policies, which will apply
beforeanybenetsarepayablebytheinsurer.Adeductibledoesnot
reduce the sum insured.
13. Dental Treatment Dental treatment means a treatment related to
teeth or structures supporting teeth including examinations, llings
(where appropriate), crowns, extractions and surgery.
14. DisclosuretoInformationNorm means the Policy shall be void and
all premium paid hereon shall be forfeited to the Company, in the event
of misrepresentation, mis-description or non-disclosure of any material
fact.
15. DomiciliaryHospitalization means medical treatment for an illness/
disease/injury which in the normal course would require care and
treatment at a hospital but is actually taken while conned at home
under any of the following circumstances:
a) the condition of the patient is such that he/she is not in a condition
to be removed to a hospital, or
b) the patient takes treatment at home on account of non - availability
of room in a hospital.
16. Emergency Care means management for a severe illness or injury
which results in symptoms which occur suddenly and unexpectedly,
and requires immediate care by a medical practitioner to prevent death
or serious long term impairment of the insured person’s health.
17. GracePeriodmeansthespeciedperiodoftimeimmediatelyfollowing
the premium due date during which a payment can be made to renew or
continueapolicyinforcewithoutlossofcontinuitybenets such as
waiting periods and coverage of pre- existing diseases. Coverage is not
available for the period for which no premium is received.
18. Hospital means any institution established for in - patient care and day
care treatment of illness and/or injuries and which has been registered
as a hospital with the local authorities, under the Clinical
Establishments(RegistrationandRegulation)Act,2010orunderthe
enactmentsspeciedundertheScheduleofSection56(1)ofthesaid
Act OR complies with all minimum criteria as under:
- hasqualiednursingstaffunderitsemploymentroundtheclock;
- hasatleast10In-patientbeds,intownshavingapopulationofless
than10,00,000andatleast15In-patientbedsinallotherplaces;
- hasqualiedmedicalpractitioner(s)inchargeroundtheclock;
- has a fully equipped operation theatre of its own where surgical
procedures are carried out
- maintains daily records of patients and makes these accessible to
the Insurance company’s authorized personnel.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
19.HospitalizationorHospitalized means admission in a hospital for a
minimum period of 24 consecutive in patient care hours except for
speciedprocedures/treatments,where such admissioncouldbefor
a period of less than 24 consecutive hours.
20.Illness means a sickness or disease or pathological condition leading
to the impairment of normal physiological function and requires medical
treatment.
a) Acute condition Acute condition is a disease, illness or injury
that is likely to respond quickly to treatment which aims to return
the person to his or her state of health immediately before suffering
the disease/illness/injury which leads to full recovery
b) Chroniccondition-Achronicconditionisdenedasadisease,
illness, or injury that has one or more of the following characteristics:
1. it needs ongoing or long-term monitoring through consultations,
examinations, check-ups, and /or tests
2. it needs ongoing or long-term control or relief of symptoms
3. it requires rehabilitation for the patient or for the patient to be
specially trained to cope with it
4. itcontinuesindenitely
5. it recurs or is likely to recur
21. Injury means accidental physical bodily harm excluding illness or
disease solely and directly caused by external, violent and visible and
evidentmeanswhichisveriedandcertiedbyaMedicalPractitioner.
22. In-patientCare means treatment for which the Insured Person has to
stay in a hospital for more than 24 hours for a covered event.
23. Intensive Care Unit means an identiedsection,wardorwingofa
Hospital which is under the constant supervision of a dedicated medical
practitioner (s), and which is specially equipped for the continuous
monitoring and treatment of patients who are in a critical condition, or
require life support facilities and where the level of care and supervision
is considerably more sophisticated and intensive than in the ordinary
and other wards.
24. Medical Advice means any consultation or advise from a Medical
Practitioner including the issue of any prescription or follow-up
prescription.
25. Medical Expenses means those expenses that an Insured Person
has necessarily and actually incurred for medical treatment on account
of Illness or Accident on the advise of a Medical Practitioner, as long as
these are no more than would have been payable if the Insured Person
had not been insured and no more than other hospitals or doctors in the
same locality would have charged for the same medical treatment.
26. Medically Necessary Treatment or Medically Necessary means
any treatment, tests, medication, or stay in Hospital or part of a stay in
Hospital which
• Is required for the medical management of the Illness or injury
suffered by the Insured;
• Must not exceed the level of care necessary to provide safe,
adequate and appropriate medical care in scope, duration or
intensity.
• Must have been prescribed by a Medical Practitioner.
• Must conform to the professional standards widely accepted in
international medical practice or by the medical community in India.
27. MedicalPractitionerA Medical practitioner means a person who holds
a valid registration from the medical council of any state or Medical
Council of India or Council for Indian Medicine or for Homeopathy set
up by Government of India or a State Government and is and is thereby
entitled to practice medicine within its jurisdiction; and is acting within
the scope and jurisdiction of license.
28. NetworkProvider means hospitals or health care provider enlisted by
an insurer, TPA or jointly by an insurer and TPA to provide medical
services to an insured by a cashless facility.
29. Non-NetworkProvider Any hospital, day care centre or other provider
that is not part of the network.
30. Notication of Claim Notication of claim means the process of
intimating a claim to the insurer or TPA through any of the recognized
modes of communication.
31. Migration means, the right accorded to health insurance policyholders
(including all members under family cover and members of group
Health insurance policy), to transfer the credit gained for pre-existing
conditions and time bound exclusions, with the same insurer.
32. OPDTreatment- OPD treatment is one in which the Insured visits a
clinic / hospital or associated facility like a consultation room for
diagnosis and treatment based on the advice of a Medical Practitioner.
The Insured is not admitted as a day care or In-Patient.
33. Pre-existingDisease means any condition, ailment, injury or disease
a. That is/are diagnosed by a physician within 48 months prior to the
effective date of the policy issued by the insurer or its reinstatement
or
b. For which medical advice or treatment was recommended by, or
received from, a physician within 48 months prior to the effective
date of the policy issued by the insurer or its reinstatement.
34. Pre-hospitalizationMedicalExpenses
Pre-hospitalization Medical Expenses means medical expenses
incurredduringpredenednumberofdaysprecedingtheHospitalization
of the Insured Person, provided that:
- Such Medical Expenses are incurred for the same condition for
which the Insured Person’s Hospitalization was required, and
- The In-patient Hospitalization claim for such Hospitalization is
admissible by the Insurance Company.
35. Post-hospitalizationMedicalExpenses
Post-hospitalization Medical Expenses means medical expenses
incurred during predened number of days immediately after the
insured person is discharged from the hospital provided that:
i. Such Medical Expenses are for the same condition for which the
insured person’s Hospitalization was required, and
ii. The inpatient Hospitalization claim for such Hospitalization is
admissible by the insurance company.
36. Portability means the right accorded to an individual health insurance
policyholder (including all members under family cover), to transfer the
credit gained for pre-existing conditions and time bound exclusions,
from one insurer to another insurer.
37. QualiedNurse means a person who holds a valid registration from
the Nursing Council of India or the Nursing Council of any state in
India.
38. Reasonable and Customary Charges means the charges for
servicesor supplies,which arethe standardcharges forthespecic
provider and consistent with the prevailing charges in the geographical
area for identical or similar services, taking into account the nature of
the illness / injury involved.
39. Renewal means the terms on which the contract of insurance can be
renewed on mutual consent with a provision of grace period for treating
the renewal continuous for the purpose of gaining credit for pre-existing
diseases, time-bound exclusions and for all waiting periods.
40. Room Rent Room Rent means the amount charged by a Hospital
towards Room and Boarding expenses and shall include the associated
medical expenses.
41. Surgery or Surgical Procedure means manual and / or operative
procedure (s) required for treatment of an illness or injury, correction of
deformities and defects, diagnosis and cure of diseases, relief from
suffering and prolongation of life, performed in a hospital or day care
centre by a medical practitioner
42. Unproven/Experimentaltreatmentmeans the treatment including
drug experimental therapy which is not based on established medical
practice in India, is treatment experimental or unproven.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
B.II.SpecicDenitions
1. Age or Aged is the age at last birthday, and which means completed
years as at the date of Inception of the Policy.
2. Ambulance means a road vehicle operated by a licenced authorised
service provider and equipped for the transport and paramedical
treatment of the person requiring medical attention.
3. Annexure means a document attached and marked as Annexure to
this Policy
4. Associated Medical Expenses. shall include Room Rent, nursing
charges, operation theatre charges, fees of Medical Practitioner/
surgeon/ anesthetist/ Specialist, excluding cost of pharmacy and
consumables, cost of implants and medical devices, cost of diagnostics
conducted within the same Hospital where the Insured Person has
been admitted. It shall not be applicable for Hospitalization in ICU.
Associated Medical Expenses shall be applicable for covered
expenses, incurred in Hospitals which follow differential billing based on
the room category.
5. AYUSH treatment refers to the medical and /or hospitalization
treatments given under Ayurveda, Yoga and Naturopathy, Unani,
Siddha and Homeopathy Systems.
6. InceptionDatemeanstheInceptiondateofthisPolicyasspeciedin
the Schedule
7. CosmeticSurgerymeansSurgeryorMedicalTreatmentthatmodies,
improves, restores or maintains normal appearance of a physical
feature, irregularity, or defect.
8. CoveredRelationshipsshallinclude spouse, children, brother and
sister of the Policyholder who are children of same parents, father,
mother, grandparents, grandchildren, parent in laws, son in law,
daughter in law, Uncle, Aunt, Niece and Nephew.
9. DependentChild A dependent child refers to a child (natural or legally
adopted),whoisnanciallydependentonthePolicyHolder,doesnot
have his / her independent source of income, is up to the age of 17
years.
10. Emergency shall mean a serious medical condition or symptom
resulting from injury or sickness which arises suddenly and
unexpectedly, and requires immediate care and treatment by a medical
practitioner, generally received within 24 hours of onset to avoid
jeopardy to life or serious long term impairment of the insured person’s
health, until stabilisation at which time this medical condition or
symptom is not considered an emergency anymore.
11. Indian Resident - An individual will be considered to be resident of
India, if he is in India for a period or periods amounting in all to one
hundred and eighty-two days or more, in the immediate preceding 365
days.
12. In-patient means an Insured Person who is admitted to hospital and
stays for at least 24 consecutive hours for the sole purpose of receiving
treatment.
13. InsuredPerson means the person (s) named in the Schedule to this
Policy, who is / are covered under this Policy, for whom the insurance is
proposed and the appropriate premium paid.
14. Policy means this Terms & Conditions document, the Proposal Form,
PolicySchedule,Add-OnBenetDetails(ifapplicable)andAnnexures
which form part of the Policy contract including endorsements, as
amended from time to time which form part of the Policy Contract and
shall be read together.
15. PolicyPeriod means the period between the inception date and the
expirydateofthepolicyasspeciedintheScheduletothisPolicyor
the date of cancellation of this policy, whichever is earlier.
16. PolicyYear means a period of 12 consecutive months within the Policy
Period commencing from the Policy Anniversary Date / Commencement
Date.
17. PolicySchedule means Schedule attached to and forming part of this
Policy mentioning the details of the Policy Holder, Insured Persons, the
Sum Insured, the period and the limits to which benets under
the Policy are subject to, Premium Paid (including taxes), including any
annexures and/or endorsements, made to or on it from time to time,
and if more than one, then the latest in time.
18. RestoredSumInsured means the amount restored in accordance with
Section D.I.8 of this Policy
19. SinglePrivateA/CRoom means a single Hospital room with any rating
and of most economical category available at the time of hospitalization
with air-conditioning facility where a single patient is accommodated
and which has an attached toilet (lavatory and bath). The room should
have the provision for accommodating an attendant. This excludes a
suite or higher category.
20. Sum Insured means, subject to terms, conditions and exclusions of
this Policy, the amount representing Our maximum liability for any or
all claims during the Policy Period specied in the Schedule to this
Policy separately in respect of that Insured Person.
i. In case where the Policy Period for 2/3 years, the Sum Insured
speciedon thePolicyisthelimitforthe rstPolicyYear.These
limitswilllapseattheendoftherstyearandthefreshlimitsupto
the full Sum Insured as opted will be available for the second/third
year.
ii. In the event of a claim being admitted under this Policy, the Sum
Insured for the remaining Policy Period shall stand correspondingly
reduced by the amount of claim paid (including ’taxes’) or admitted
and shall be reckoned accordingly.
21. TPA Third Party Administrator (TPA) means a company registered
with the Authority, and engaged by Us, for a fee or, by whatever name
called and as may be mentioned in the health services agreement, for
providing health services as mentioned under TPA Regulations.
22. We/Our/Us/Insurer means ManipalCigna Health Insurance Company
Limited
23. You/Your/PolicyHolder means the person named in the Schedule as
the policyholder and who has concluded this Policy with Us.
C. Benetscoveredunderthepolicy
C.I. Basiccovers
C.I.1.InpatientHospitalization
We will cover Medical Expenses of an Insured Person in case of
Medically Necessary Hospitalization arising from a Disease/ Illness or
Injury provided such Medically Necessary Hospitalization is for more
than 24 consecutive hours provided that the admission date of the
Hospitalization due to Disease/ Illness or Injury is within the Policy
Year. We will pay Medical Expenses as mentioned in the Policy
Schedule for:
a. Reasonable and Customary Charges for Room Rent for
accommodation in Hospital room up to Category as per opted Sum
InsuredandasspeciedinthePolicySchedule.
b. Intensive Care Unit charges for accommodation in ICU,
c. Operation theatre charges,
d. Fees of Medical Practitioner/ Surgeon,
e. Anaesthetist,
f. QualiedNurses,
g. Specialists,
h. Cost of diagnostic tests,
i. Medicines,
j. Drugs and consumables, blood, oxygen, surgical appliances and
prosthetic devices recommended by the attending Medical
Practitioner and that are used intra operatively during a Surgical
Procedure.
Room category coverage for Sum Insured under each plan will be up
tothelimitaspertheSumInsuredoptedandasspeciedinthePolicy
Schedule. For ICU accommodation, we will cover up to Sum Insured

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
optedandasspeciedinthePolicySchedule.
If the Insured Person is admitted in a room category that is higher than
theonethatisspeciedinthePolicySchedule,thenthePolicyholder/
Insured Person shall bear a ratable proportion of the total Associated
Medical Expenses (including surcharge or taxes thereon) in the
proportion of the difference between the room rent of the entitled room
category to the room rent actually incurred.
Under In-patient Hospitalization expenses, when availed under
In-patient care, we will cover the expenses towards articial life
maintenance, including life support machine use, even where such
treatment will not result in recovery or restoration of the previous state
of health under any circumstances unless in a vegetative state, as
certiedbythetreatingMedicalPractitioner.
We will indemnify the Medical Expenses incurred by an Insured Person
in respect of the below listed ailments / procedures (refer the table
below) up to the limits specied against each and every ailment /
procedure for the applicable Sum Insured options:
Sum Insured (in `) `3 Lacs `5 Lacs `7.5 and
`10Lacs
>`10
Lacs
Treatment for each
ailment / procedure
mentioned below:
1. Surgery for
treatment of all
types of Hernia
2. Hysterectomy
3. Surgeries for
benign Prostate
Hyper trophy
4. Surgical treatment
of stones of renal
system
`50,000 `65,000 `80,000
NA
Treatment of
Cataract (Per Eye)
`20,000 `30,000 `30,000
NA
Treatment of Total
Knee replacement
(Per knee)
`80,000 `1,00,000 `1,20,000
NA
Treatment for
breakage of bones
`2,00,000 `2,50,000 `3,00,000
NA
Wherever the above mentioned Sub-limits are applied, the Mandatory
Co-payment under section F.II.6 shall not be applicable. The following
procedures will be covered (wherever medically indicated) either as
In-patientoraspartofDayCareTreatmentinahospitalupto50%of
theSumInsuredasspeciedinthePolicySchedule,duringthePolicy
Year:
a. Uterine Artery Embolization and HIFU (High intensity focused
ultrasound)
b. Balloon Sinuplasty
c. Deep Brain stimulation
d. Oral chemotherapy
e. Immunotherapy - Monoclonal Antibody to be given as injection
f. Intra vitreal injections
g. Robotic surgeries
h. Stereotactic radio surgeries
i. Bronchial Thermoplasty
j. Vaporization of the prostrate (Green laser treatment or holmium
laser treatment)
k. IONM - (Intra Operative Neuro Monitoring)
l. Stem cell therapy: Hematopoietic stem cells for bone marrow
transplant for hematological conditions to be covered.
Medical Expenses incurred towards Medically Necessary Treatment of
the Insured Person for In-patient Hospitalization due to a condition
caused by or associated with Human Immunodeciency Virus (HIV)
or HIV related Illnesses, including Acquired Immune Deciency
Syndrome (AIDS) or AIDS Related Complex (ARC) and/or any mutant
derivative or variations thereof, sexually transmitted diseases (STD), in
respect of an Insured Person, will be covered up to the Sum Insured as
speciedinthePolicyScheduleduringthePolicyYear.Thenecessity
of the Hospitalization is to be certied by an authorized Medical
Practitioner.
Medical Expenses incurred towards Medically Necessary treatment
taken during In-patient Hospitalization of the Insured Person, arising
out of a condition caused by or associated to a Mental illness, or a
medicalconditionimpactingmentalhealthwillbecoveredupto50%
oftheSumInsuredasspeciedinthePolicyScheduleduringthePolicy
Year. For the below mentioned ICD Codes, the Insured Person should have
been continuously covered under this Policy for at least 24 months before
availingthisbenet.
ICD 10
CODES
DISEASES
F05 Delirium due to known physiological condition
F06 Other mental disorders due to known physiological condition
F07
Personality and behavioural disorders due to known
physiological condition
F10 Mental and behavioural disorders due to use of alcohol
F20 Schizophrenia
F23 Brief psychotic disorders
F25 Schizoaffective disorders
F29
Unspeciedpsychosisnotduetoasubstanceorknown
physiological condition
F31 Bipolar disorder
F32 Depressive episode
F39 Unspeciedmood[affective]disorder
F40 Phobic Anxiety disorders
F41 Other Anxiety disorders
F42 Obsessive-compulsive disorder
F44 Dissociative and conversion disorders
F45 Somatoform disorders
F48 Other nonpsychotic mental disorders
F60 Specicpersonalitydisorders
F84 Pervasive developmental disorders
F90 Attention-decithyperactivitydisorders
F99 Mentaldisorder,nototherwisespecied
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 and G.I.5.
C.I.2 Pre-hospitalization
We will, on a reimbursement basis cover Medical Expenses of an
Insured Person which are incurred due to a Disease/ Illness or Injury
that occurs during the Policy Year immediately prior to the Insured
Person’s date of Hospitalization up to the limits as specied in the
Policy Schedule, provided that a Claim has been admitted under
In-patientbenetunderSectionD.I.1andisrelatedtothesameillness/
condition.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5 & G.I.9.
C.I.3 Post-hospitalization
We will, on a reimbursement basis cover Medical Expenses of an
Insured Person which are incurred due to a Disease/ Illness or Injury
that occurs during the Policy Year immediately post discharge of the
InsuredPersonfromthe Hospital uptothelimits as speciedinthe
Policy Schedule, provided that a Claim has been admitted under
In-patientbenetunderSectionD.I.1andisrelatedtothesameillness/
condition.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5 & G.I.9.
C.I.4 DayCareTreatment
We will cover payment of Medical Expenses of an Insured Person in
case of Medically Necessary Day Care Treatment or Surgery that
requires less than 24 hours of Hospitalization due to advancement in
technology and which is undertaken in a Hospital / nursing home/ Day
Care Centre on the recommendation of a Medical Practitioner, up to
theSumInsuredasspeciedinthePolicySchedule,providedthat:

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
a. The Day Care Treatment is Medically Necessary and follows the
written advice of a Medical Practitioner.
b. The Medical Expenses incurred are Reasonable and Customary
Charges for any procedure where such procedure is undertaken by
an Insured Person as Day Care Treatment.
c. We will not cover any OPD Treatment and Diagnostic Services
underthisbenet.
Coverage will also include pre-post hospitalization expenses as per the
limitsapplicableandspeciedunderthePlanopted.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.5 DomiciliaryHospitalization
We will cover Medical Expenses of an Insured Person up to the limits
speciedinthePolicySchedule,whicharetowardsaDisease/Illness
or Injury which in the normal course would otherwise have been covered
for Hospitalization under the policy but is taken at home on the advice
of the attending Medical Practitioner, under the following circumstances:
i. The condition of the Insured Person does not allow a Hospital
transfer; or
ii. A Hospital bed was unavailable;
Provided that, the treatment of the Insured Person continues for at
least 3 days, in which case the reasonable cost of any Medically
Necessary treatment for the entire period shall be payable.
a) We will pay for Pre-hospitalization, Post-hospitalization Medical
Expensesupto30dayseach.
b) RestorationofSumInsuredshallnotbeavailableunderthisbenet
c) We shall not be liable under this Policy for any Claim in connection
with or in respect of the following:
i. Asthma, COPD, bronchitis, tonsillitis and upper & lower
respiratory tract infection including laryngitis and pharyngitis,
coughandcold,inuenza,
ii. Arthritis, gout and rheumatism including the rheumatism of
bones, joints and also rheumatic heart disease,
iii. Chronic nephritis and nephritic syndrome,
iv. All types of Diarrhea and dysenteries, including gastroenteritis,
v. Diabetes mellitus and Diabetes Insipidus,
vi. Epilepsy / Seizure disorder,
vii. Hypertension,
viii. Pyrexia of unknown origin.
All Claims under this benet can be made as per the process
denedunderSectionG.I.5.
C.I.6. RoadAmbulance
We will provide for reimbursement of Reasonable and Customary
expensesuptotheSumInsuredasspeciedinthePolicySchedule
that are incurred towards road transportation of an Insured Person by a
registered Healthcare or Ambulance Service Provider to a nearest
Hospital for treatment of an Illness or Injury covered under the Policy
in case of an Emergency, necessitating the Insured Person’s admission
to the Hospital, provided that a Claim has been admitted under In-
patientbenetunderSectionD.I.1andisrelatedtothesameillness/
condition.
ThenecessityofuseofanAmbulancemustbecertiedbythetreating
Medical Practitioner.
a. Reasonable and Customary expenses shall include:
(i) Costs towards transferring the Insured Person from one
Hospital to another Hospital or diagnostic centre for advanced
diagnostic treatment where such facility is not available at the
existing Hospital; or
(ii) When the Insured Person requires to be moved to a better
Hospital facility due to lack of super speciality treatment in the
existing Hospital.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5.
C.I.7.DonorExpenses
We will cover In-patient Hospitalization Medical Expenses towards the
donorforharvestingtheorganuptotheSumInsuredasspeciedin
the Policy Schedule, subject to the below mentioned conditions:
a. The organ donor is any person in accordance with the Transplantation
of Human Organs Act 1994 (amended) and other applicable laws and
rules, provided that -
i. The organ donated is for the use of the Insured Person who has
been asked to undergo an organ transplant on Medical Advice.
b. We have admitted a claim under Section D.I.1 - towards In-patient
Hospitalization
c. We will not cover expenses towards the Donor in respect of:
i. Any Pre or Post-hospitalization Medical Expenses,
ii. Cost towards donor screening,
iii. Cost associated to the acquisition of the organ,
iv. Any other medical treatment or complication in respect of the
donor, consequent to harvesting.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.8 RestorationofSumInsured:
We will provide for a 100% restoration of the Sum Insured for any
number of times in a Policy Year, provided that:
a. The Sum Insured inclusive of earned Cumulative Bonus (if any) is
insufcientasaresultofpreviousclaimsinthatPolicyYear.
b. The Restored Sum Insured shall not be available for claims towards
an Illness/ disease/ Injury (including its complications) for which a
claim has been paid in the current Policy Year for the same Insured
Person.
c. The Restored Sum Insured will be available only for claims made
by Insured Persons in respect of future claims that become
payableunderSectionDofthePolicyandshallnotapplytotherst
claim in the Policy Year. Restoration of the Sum Insured will only
be provided for coverage under Section D.I.1 ‘In-patient
Hospitalization’, Section D.I.2 ‘Pre-Hospitalization’, Section D.I.3
‘Post-Hospitalization’, Section D.I.4 ‘Day Care Treatment’, Section
D.I.6 ‘Road Ambulance’, Section D.I.7 ‘Donor Expenses’, Section
D.I.9 ‘AYUSH Treatment (In-patient Hospitalization)’ Section D.III.1
‘Non-Medical Items’.
d. The Restored Sum Insured will not be considered while calculating
the Cumulative Bonus.
e. Such restoration of Sum Insured will be available for any number of
times, during a Policy Year to each insured in case of an Individual
Policy and can be utilized by Insured Persons who stand covered
under the Policy before the Sum Insured was exhausted.
f. If the Restored Sum Insured is not utilized in a Policy Year, it shall
not be carried forward to subsequent Policy Year.
g. For any single claim during a Policy Year the maximum claim
amount payable shall be sum of:
i. The Sum Insured
ii. Cumulative Bonus (if earned)
iii. Restored Sum Insured
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.9AYUSHTreatment(In-patientHospitalization)
We will pay the Medical Expenses incurred during the Policy Year, up
totheSumInsured,asspeciedinthePolicySchedule,foranInsured
Person in case of Medically Necessary Treatment taken during In-
patient Hospitalization for AYUSH Treatment for an Illness or Injury that
occurs during the Policy Year, provided that:
The Insured Person has undergone treatment in an AYUSH Hospital
where AYUSH Hospital is a healthcare facility wherein medical/
surgical/ para-surgical treatment procedures and interventions are
carried out by AYUSH Medical Practitioner (s) comprising any of the
following:
i) Central or State Government AYUSH Hospital; or
ii) Teaching hospitals attached to AYUSH College recognized by
Central Government / Central Council of Indian Medicine and
Central Council of Homeopathy; or
iii) AYUSH Hospital, standalone or co-located with in-patient
healthcare facility of any recognized system of medicine, registered
with the local authorities, wherever applicable, and is under the
supervision of a qualied registeredAYUSH Medical Practitioner
and must comply with all the following criterion:
a) Havingatleastvein-patientbeds;

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
b) Having qualiedAYUSHMedicalPractitioner inchargeround
the clock;
c) Having dedicated AYUSH therapy sections as required and/or
has equipped operation theatre where surgical procedures are
to be carried out;
d) Maintaining daily record of the patients and making them
accessible to the insurance company’s authorized
representative.
The following exclusions will be applicable in addition to the other
Policy exclusions:
Facilities and services availed for pleasure or rejuvenation or as a
preventiveaid,likebeautytreatments,Panchakarma,purication,
detoxicationandrejuvenation.
AllclaimsunderthisBenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.I.10 ConvalescenceBenet:
We will pay, a lump sum amount as per the Sum Insured opted and as
specied in the Policy Schedule against this benet, if the Insured
PersonhasbeenHospitalizedforatleast10consecutivedaysforAny
one illness or Accident, provided that:
i. The Hospitalization is only for In-patient care for the Insured
Person; and
ii. The benets payable under this cover are for each
Hospitalization
iii. Benets payable under this cover are over and above Sum
Insured.
iv. We have accepted claim under Section D.I.1 In-patient
Hospitalization during the Policy Year
All claims under this benet can be made as per the process
denedunderSectionG.I.5.
C.I.11 DailyCashforSharedAccommodation
WewillpayadailycashamountasspeciedinthePolicyScheulefor
the Insured Person for each continuous and completed period of 24
hours of Hospitalization provided that,
a. We have accepted claim under Section D.I.1 In-patient
Hospitalization during the Policy Year
b. The Insured Person has occupied a shared room accommodation
during such Hospitalization
c. The Insured Person has been admitted in a Hospital for a minimum
period of 48 hours continuously.
d. Sum Insured opted under the Policy and mentioned in Policy
Schedule is Rs. 5 Lacs and above.
What is not covered:
This benet will not be payable if the Insured Person stays in an
Intensive Care Unit or High Dependency Units / wards.
AllClaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.5
C.II.Valueaddedcovers
C.II.1 DomesticSecondOpinion:
You may choose to secure a second opinion from Our Network of
Medical Practitioners in India, if an Insured Person is diagnosed with the
covered Critical Illness during the Policy Year. The expert opinion would
be directly sent to the Insured Person.
You understand and agree that You can exercise the option to secure
an expert opinion, provided:
(a) We have received a request from You to exercise this option.
(b) That the expert opinion will be based only on the information and
documentation provided by You that will be shared with the Medical
Practitioner
(c)This benet can be availed by each Insured Person only once
during a Policy Year for one Critical Illness and multiple times for
different Critical Illness/es with the same limitation of one opinion
per critical illness
(d)ThisbenetisonlyavalueaddedserviceprovidedbyUsanddoes
not deem to substitute the Insured Person’s visit or consultation to
an independent Medical Practitioner.
(e) The Insured Person is free to choose whether or not to obtain the
expert opinion, and if obtained then whether or not to act on it.
(f) We shall not, in any event be responsible for any actual or alleged
errors or representations made by any Medical Practitioner or in
any expert opinion or for any consequence of actions taken or not
taken in reliance thereon.
(g) The expert opinion under this Policy shall be limited to covered
Critical Illnesses and not be valid for any medico legal purposes.
(h) We do not assume any liability towards any loss or damage arising
out of or in relation to any opinion, advice, prescription, actual or
alleged errors, omissions and representations made by the Medical
Practitioner.
(i) AnyclaimunderthisbenetwillnotimpacttheSumInsuredand/
or Cumulative Bonus.
For the purpose of this benet, covered Critical Illnesses shall
include as below:
1. CancerofSpeciedSeverity
A malignant tumour characterised by the uncontrolled growth & spread
of malignant cells with invasion & destruction of normal tissues. This
diagnosis must be supported by histological evidence of malignancy.
The term cancer includes leukemia, lymphoma and sarcoma.
The following are excluded -
i. All tumors which are histologically described as carcinoma in situ,
benign, pre-malignant, borderline malignant, low malignant
potential, neoplasm of unknown behavior, or non-invasive,
including but not limited to: Carcinoma in situ of breasts, Cervical
dysplasia CIN-1, CIN -2 and CIN-3.
ii. Any non - melanoma skin carcinoma unless there is evidence of
metastases to lymph nodes or beyond;
iii. Malignant melanoma that has not caused invasion beyond the
epidermis;
iv. Alltumorsoftheprostateunlesshistologicallyclassiedashaving
a Gleason score greater than 6 or having progressed to at least
clinicalTNMclassicationT2N0M0
v. All Thyroid cancers histologically classied as T1N0M0 (TNM
Classication)orbelow;
vi. Chronic lymphocytic leukaemia less than RAI stage 3
vii. Non - invasive papillary cancer of the bladder histologically
describedasTaN0M0orofalesserclassication,
viii.All Gastro-Intestinal Stromal Tumors histologically classied as
T1N0M0 (TNM Classication) or below and with mitotic count of
lessthanorequalto5/50HPFs;
ix. All tumors in the presence of HIV infection.
2. MyocardialInfarction(FirstHeartAttackofSpeciedSeverity)
I The rst occurrence of heart attack or myocardial infarction, which
means the death of a portion of the heart muscle as a result of
inadequate blood supply to the relevant area. The diagnosis for this
will be evidenced by all of the following criteria:
i. a history of typical clinical symptoms consistent with the diagnosis
of Acute Myocardial Infarction (for e.g. typical chest pain)
ii. new characteristic electrocardiogram changes
iii. elevation of infarction specic enzymes, Troponins or other
specicbiochemicalmarkers.
II The following are excluded:
1. Other acute Coronary Syndromes
2. Any type of angina pectoris.
3. A rise in cardiac biomarkers or Troponin T or I in absence of
overt ischemic heart disease OR following an intra - arterial cardiac
procedure.
3. OpenChestCABG
I The actual undergoing of heart surgery to correct blockage or
narrowing in one or more coronary artery (s), by coronary artery bypass
grafting done via a sternotomy (cutting through the breast bone) or
minimally invasive keyhole coronary artery bypass procedures. The
diagnosis must be supported by a coronary angiography and the
realisationofsurgeryhastobeconrmedbyacardiologist.
II The following are excluded:
a. Angioplasty and/or any other intra-arterial procedures

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
4. OpenHeartReplacementorRepairofHeartValves
The actual undergoing of open-heart valve surgery is to replace or
repair one or more heart valves, as a consequence of defects in,
abnormalities of, or disease-affected cardiac valve (s). The diagnosis
of the valve abnormality must be supported by an echocardiography
and the realization of surgery has to be conrmed by a specialist
medical practitioner. Catheter based techniques including but not
limited to, balloon valvotomy/valvuloplasty are excluded.
5. ComaofSpeciedSeverity
1. A state of unconsciousness with no reaction or response to external
stimuli or internal needs.
This diagnosis must be supported by evidence of all of the following:
i. no response to external stimuli continuously for at least 96 hours;
ii. life support measures are necessary to sustain life; and
iii. permanent neurological decit which must be assessed at least
30daysaftertheonsetofthecoma.
2. Theconditionhastobeconrmedbyaspecialistmedicalpractitioner.
Coma resulting directly from alcohol or drug abuse is excluded.
6. KidneyFailureRequiringRegularDialysis
End stage renal disease presenting as chronic irreversible failure of
both kidneys to function, as a result of which either regular
renaldialysis (haemodialysis or peritoneal dialysis) is instituted or renal
transplantation is carried out. Diagnosis has to be conrmed by a
specialist medical practitioner.
7. StrokeResultinginPermanentSymptoms
Any cerebrovascular incident producing permanent neurological
sequelae. This includes infarction of brain tissue, thrombosis in an
intracranial vessel, haemorrhage and embolization from an extra
cranialsource.Diagnosishastobeconrmedbyaspecialistmedical
practitioner and evidenced by typical clinical symptoms as well as
typical ndings in CT Scan or MRI of the brain. Evidence of
permanentneurologicaldecitlastingforatleast3monthshastobe
produced.
The following are excluded:
1. Transient ischemic attacks (TIA)
2. Traumatic injury of the brain
3. Vascular disease affecting only the eye or optic nerve or vestibular
functions.
8. MajorOrgan/BoneMarrowTransplant
The actual undergoing of a transplant of:
1. One of the following human organs: heart, lung, liver, kidney,
pancreas, that resulted from irreversible end - stage failure of the
relevant organ, or
2. Human bone marrow using haematopoietic stem cells. The
undergoing of a transplant has to be conrmed by a specialist
medical practitioner.
The following are excluded:
i. Other stem-cell transplants
ii. Where only islets of langerhans are transplanted
9. PermanentParalysisofLimbs
Total and irreversible loss of use of two or more limbs as a result of
injury or disease of the brain or spinal cord. A specialist medical
practitioner must be of the opinion that the paralysis will be permanent
with no hope of recovery and must be present for more than 3 months.
10.MotorNeuronDiseasewithPermanentSymptoms
Motor neuron disease diagnosed by a specialist medical practitioner
as spinal muscular atrophy, progressive bulbar palsy, amyotrophic
lateral sclerosis or primary lateral sclerosis. There must be
progressive degeneration of corticospinal tracts and anterior horn
cellsorbulbarefferentneurons.Theremustbecurrentsignicantand
permanent functional neurological impairment with objective evidence
of motor dysfunction that has persisted for a continuous period of at
least 3 months.
11 MultipleSclerosiswithPersistingSymptoms
I. TheunequivocaldiagnosisofDeniteMultipleSclerosisconrmedand
evidenced by all of the following:
1. investigations including typical MRI ndings which unequivocally
conrmthediagnosistobemultiplesclerosis;
2. there must be current clinical impairment of motor or sensory
function, which must have persisted for a continuous period of at
least 6 months, and
II. Other causes of neurological damage such as SLE and HIV are
excluded.
12. Primary(Idiopathic)PulmonaryHypertension
I. An unequivocal diagnosis of Primary (Idiopathic) Pulmonary
Hypertension by a Cardiologist or specialist in respiratory medicine with
evidence of right ventricular enlargement and the pulmonary arterypres
sureabove30mmofHgonCardiacCauterization.
There must be permanent irreversible physical impairment to the
degree of at least Class IV of the New York Heart Association
Classicationofcardiacimpairment.
II. TheNYHAClassicationofCardiacImpairmentareasfollows:
i. Class III: Marked limitation of physical activity. Comfortable at rest,
but less than ordinary activity causes symptoms.
ii. Class IV: Unable to engage in any physical activity without
discomfort. Symptoms may be present even at rest.
III. Pulmonary hypertension associated with lung disease, chronichy
poventilation, pulmonary thromboembolic disease, drugs and toxins,
diseases of the left side of the heart, congenital heart disease and any
secondarycausearespecicallyexcluded.
13. AortaGraftSurgery
The actual undergoing of major Surgery to repair or correct aneurysm,
narrowing, obstruction or dissection of the Aorta through surgical
opening of the chest or abdomen.
Forthepurposeofthisbenet,Aortameansthethoracicandabdomnal
aorta but not its branches.
You understand and agree that We will not cover:
a. Surgery performed using only minimally invasive or intra-arterial
techniques.
b. Angioplasty and all other intra-arterial, catheter based techniques,
“keyhole” or laser procedures.
c. Congenital narrowing of the aorta and traumatic injury of the aorta
arespecicallyexcluded.
14. Deafness
Total and irreversible Loss of hearing in both ears as a result of Illness
or accident.
This diagnosis must be supported by pure tone audiogram test and
certiedbyanEar,NoseandThroat(ENT)specialist.Totalmeans“the
lossofhearingtotheextentthatthelossisgreaterthan90decibels
across all frequencies of hearing” in both ears.
15. Blindness
I. Total, permanent and irreversible loss of all vision in both eyes as a
result of illness or accident.
II. The Blindness is evidenced by:
i. correctedvisualacuitybeing3/60orlessinbotheyesor;
ii. theeldofvisionbeinglessthan10degreesinbotheyes.
III. The diagnosis of blindness must be conrmed and must not be
correctable by aids or surgical procedure.
16. AplasticAnemia
Chronic persistent bone marrow failure which results in anemia,
neutropenia and thrombocytopenia requiring treatment with at least
one of the following:
a. Blood product transfusion;
b. Marrow stimulating agents;
c. Immunosuppressive agents; or
d. Bone marrow transplantation.
The diagnosis must be conrmed by a hematologist Medical
Practitioner using relevant laboratory investigations including Bone
MarrowBiopsyresultinginbone marrowcellularityoflessthan 25%

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
which is evidenced by any two of the following:
a.Absoluteneutrophilcountoflessthan500/mm³orless;
b. Plateletscountlessthan20,000/mm³orless;
c. Reticulocytecountoflessthan20,000/mm³orless.
We will not cover temporary or reversible Aplastic Anemia under this
Section.
17. CoronaryArteryDisease
The rst evidence of narrowing of the lumen of at least one
coronaryarterybyaminimumof75%andoftwoothersbyaminimum
of 60%, regardless of whether or not any form of coronaryartery
Surgery has been performed. Coronary arteries herein refer to left
main stem, left anterior descending circumex and right coronary
artery and not its branches which is evidenced by the following:
a. evidence of ischemia on Stress ECG (NYHA Class III symptoms)
b. coronary arteriography (Hearth Cath)
18. EndStageLungFailure
End Stage Lung Disease, causing chronic respiratory failure, as
conrmedandevidencedbyallofthefollowing:
i. FEV1 test results consistently less than 1 liter measured on 3
occasions 3 months apart; and
ii. Requiring continuous and permanent supplementary oxygen
therapy for hypoxemia; and
iii. Arterial blood gas analysis with partial oxygen pressure of
55mmHgor less (PaO2 < 55 mm Hg); and
iv. Dyspnea at rest.
19. EndStageLiverFailure
Permanent and irreversible failure of liver function that has resulted in
all three of the following:
a. Permanent jaundice;
b. Ascites; and
c. Hepatic Encephalopathy.
Liver failure secondary to drug or alcohol abuse is excluded.
20. ThirdDegreeBurns
Theremustbethird-degreeburnswithscarringthatcoveratleast20%
ofthebody’ssurfacearea.Thediagnosismustconrmthetotalarea
involved using standardized, clinically accepted, body surface
areachartscovering20%ofthebodysurfacearea.
21. FulminantHepatitis
A sub-massive to massive necrosis of the liver by the Hepatitis virus,
leading precipitously to liver failure. This diagnosis must be supported
by all of the following:
a. Rapid decreasing of liver size;
b. Necrosis involving entire lobules, leaving only a collapsed reticular
framework;
c. Rapid deterioration of liver function tests;
d. Deepening jaundice; and
e. Hepatic encephalopathy.
Acute Hepatitis infection or carrier status alone does not meet the
diagnostic criteria.
22. Alzheimer’sDisease
Alzheimer’s disease is a progressive degenerative Illness of the
brain, characterized by diffuse atrophy throughout the cerebral cortex
with distinctive histopathological changes. Deterioration or loss of
intellectualcapacity, as conrmed byclinicalevaluationandimaging
tests, arising from Alzheimer’s disease, resulting in progressive
signicant reduction in mental and social functioning, requiring the
continuous supervision of the Insured Person. The diagnosis must be
supported by the clinical conrmation of a Neurologist Medical
Practitioner and supported by Our appointed Medical Practitioner.
The following conditions are however not covered:
a. non-organic diseases;
b. alcohol related brain damage; and
c. any other type of irreversible organic disorder/dementia.
23. BacterialMeningitis
Bacterialinfectionresultinginsevereinammationofthemembranes
of the brain or spinal cord resulting in signicant, irreversible and
Permanentneurologicaldecit.Theneurologicaldecitmustpersistfor
atleast6weeks.Thisdiagnosismustbeconrmedby:
a. Thepresenceofbacterialinfectionincerebrospinaluidbylumbar
puncture; and
b. A consultant neurologist Medical Practitioner.
We will not cover Bacterial Meningitis in the presence of HIV infection
under this Section.
24. BenignBrainTumor
a. Benignbraintumorisdenedasalifethreatening,non-cancerous
tumor in the brain, cranial nerves or meninges within the skull.
The presence of the underlying tumor must be conrmed by
imaging studies such as CT scan or MRI.
b. This brain tumor must result in at least one of the following and
mustbeconrmedbytherelevantmedicalspecialist.
i. Permanent Neurological decit with persisting clinical
symptoms for a continuous period of at least 90consecutive
days or
ii. Undergone surgical resection or radiation therapy to treat the
brain tumor.
The following conditions are however not covered by Us:
a. cysts;
b. granulomas;
c. malformations in the arteries or veins of the brain;
d. hematoma;
e. Abscesses
f. Pituitary Tumors
g. tumors of skull bones and
h. tumors of the spinal cord
25. ApallicSyndrome
Universal necrosis of the brain cortex with the brainstem remaining
intact. The diagnosis must be conrmed by a Neurologist Medical
Practitioner acceptable to Us and the condition must be documented
by such Medical Practitioner for at least one month.
26. Parkinson’sDisease
The unequivocal diagnosis of progressive, degenerative idiopathic
Parkinson’s disease by a Neurologist Medical Practitioner acceptable
to Us.
The diagnosis must be supported by all of the following conditions:
a. the disease cannot be controlled with medication;
b. signs of progressive impairment; and
c. inability of the Insured Person to perform at least 3 of the 6 activities
of daily living as listed below (either with or without the use of
mechanical equipment, special devices or other aids and
adaptations in use for disabled persons) for a continuous period of
at least 6 months:
Activities of daily living:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the shower) or wash satisfactorily by other means
and maintain an adequate level of cleanliness and personal
hygiene;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garmentsand,asappropriate,anybraces,articiallimbsorother
surgical appliances;
iii. Transferring: The ability to move from a lying position in a bed to a
sitting position in an upright chair or wheel chair and vice versa;
iv. Toileting: the ability to use the lavatory or otherwise man age
bowel and bladder functions so as to maintain a satisfactory level
of personal hygiene;
v. Feeding: the ability to feed oneself, food from a plate or bowl to the
mouth once food has been prepared and made available.
vi. Mobility: The ability to move indoors from room to room on level

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
surfaces at the normal place of residence.
We will not cover Parkinson’s disease secondary to drug and/or
alcohol abuse under this Section.
27. MedullaryCysticDisease
A progressive hereditary disease of the kidneys characterized by the
presenceofcystsinthemedulla,tubularatrophyandinterstitialbrosis
with the clinical manifestations of anemia, polyuria and renal loss
of sodium, progressing to chronic renal failure. The diagnosis must be
supported by renal biopsy.
28. MuscularDystrophy
A group of hereditary degenerative diseases of muscle characterized
by progressive and permanent weakness and atrophy of certain
muscle groups. The diagnosis of muscular dystrophy must be
unequivocal and made by a Neurologist Medical Practitioner acceptable
toUs,withconrmationofatleast3ofthefollowing4conditions
a. Family history of muscular dystrophy;
b. Clinical presentation including absence of sensory disturbance,
normalcerebrospinaluidandmildtendonreexreduction;
c. Characteristic electromyogram;
d. Clinicalsuspicionconrmedbymusclebiopsy.
The condition must result in the inability of the Insured Person to
perform at least 3 of the 6 activities of daily living as listed below (either
with or without the use of mechanical equipment, special devices or
other aids and adaptations in use for disabled persons) for a continuous
period of at least 6 months:
Activities of daily living:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the shower) or wash satisfactorily by other means
and maintain an adequate level of cleanliness and personal
hygiene;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garmentsand,asappropriate,anybraces,articiallimbsorother
surgical appliances;
iii. Transferring: The ability to move from a lying position in a bed to a
sitting position in an upright chair or wheel chair and vice versa;
iv. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of
personal hygiene;
v. Feeding: the ability to feed oneself, food from a plate or bowl to the
mouth once food has been prepared and made available;
vi. Mobility: The ability to move indoors from room to room on level
surfaces at the normal place of residence.
29. LossofSpeech
a. Total and irrecoverable loss of the ability to speak as a result of
injury or disease to the vocal cords. The inability to speak must be
established for a continuous period of 12 months. This diagnosis
must be supported by medical evidence furnished by an Ear, Nose,
Throat (ENT) specialist.
b. All psychiatric related causes are excluded.
30. SystemicLupusErythematous
A multi-system, multifactorial, autoimmune disorder characterized by
the development of auto-antibodies directed against various self -
antigens. Only those forms of systemic lupus erythematous which
involve the kidneys (Class III to Class V lupus nephritis, established by
renal biopsy, and in accordance with the World Health Organization
(WHO) classication) will be covered by Us under this Section. The
naldiagnosismustbeconrmedbyaregisteredMedicalPractitioner
specializing in Rheumatology and Immunology acceptable to Us.
Other forms of systemic lupus erythematous, discoid lupus and those
forms with only hematological and joint involvement are however not
covered:
TheWHOlupusclassicationisasfollows:
• Class I: Minimal change – Negative, normal urine.
• Class II: Mesangial – Moderate proteinuria, active sediment.
• Class III: Focal Segmental – Proteinuria, active sediment.
• Class IV: Diffuse – Acute nephritis with active sediment and/or
nephritic syndrome.
• Class V: Membranous – Nephrotic Syndrome or severe proteinria.
31. LossofLimbs
a. The physical separation of two or more limbs, at or above the wrist
or ankle level limbs as a result of injury or disease. This will include
medically necessary amputation necessitated by injury or disease.
The separation has to be permanent without any chance of surgical
correction. Loss of Limbs resulting directly or indirectly from self-
inictedinjury,alcoholordrugabuseisexcluded.
32. MajorHeadTrauma
a. Accidental head injury resulting in permanent Neurological decit
to be assessed no sooner than 3 months from the date of the accident.
This diagnosis must be supported by unequivocal ndings on
Magnetic Resonance Imaging, Computerized Tomography, or other
reliable imaging techniques. The accident must be caused solely and
directly by accidental, violent, external and visible means and
independently of all other causes.
b. The Accidental Head injury must result in an inability to perform
at least three (3) of the following Activities of Daily Living either with or
without the use of mechanical equipment, special devices or other aids
and adaptations in use for disabled persons. For the purpose of this
benet,theword“permanent”shallmeanbeyondthescopeofrecovery
with current medical knowledge and technology.
c. The Activities of Daily Living are:
i. Washing: the ability to wash in the bath or shower (including getting
into and out of the bath or shower) or wash satisfactorily by other
means;
ii. Dressing: the ability to put on, take off, secure and unfasten all
garmentsand,asappropriate,anybraces,articiallimbsorother
surgical appliances;
iii. Transferring: the ability to move from a bed to an upright chair or
wheelchair and vice versa;
iv. Mobility: the ability to move indoors from room to room on level
surfaces;
v. Toileting: the ability to use the lavatory or otherwise manage bowel
and bladder functions so as to maintain a satisfactory level of
personal hygiene;
vi. Feeding: the ability to feed oneself once food has been prepared
and made available.
d. The following are excluded:
a) Spinal cord injury
33. BrainSurgery
The actual undergoing of surgery to the brain, under general
anesthesia, during which a Craniotomy is performed. Burr hole and
brain surgery as a result of an accident is excluded. The procedure
mustbeconsiderednecessarybyaqualiedspecialistandthebenet
shall only be payable once corrective surgery has been carried out.
34. Cardiomyopathy
The unequivocal diagnosis by a consultant cardiologist of
Cardiomyopathy causing impaired ventricular function suspeced by
ECGabnormalitiesandconrmedbycardiacechoofvariableetiology
and resulting in permanent physical impairments to the degree of at
least Class IV of the NewYorkAssociation (NYHA) Classication of
cardiac impairment.
The NYHA Classication of Cardiac Impairment (Source: “Current
Medical Diagnosis and Treatment – 39th Edition”):
a. Class I: No limitation of physical activity. Ordinary physical activity
does not cause undue fatigue, dyspnea, or angina pain.
b. Class II: Slight limitation of physical activity. Ordinary physical
activity results in symptoms.
c. Class III: Marked limitation of physical activity. Comfortable at rest,
but less than ordinary activity causes symptoms.
d. Class IV: Unable to engage in any physical activity without
discomfort. Symptoms may be present even at rest.
We will not cover Cardiomyopathy related to alcohol abuse under this
Section.
35. Creutzfeldt-JacobDisease(CJD)

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
A Diagnosis of Creutzfeldt-Jakob disease must be made by a Specialist
Medical Practitioner (Neurologist). There must be permanent clinical
loss of the ability in mental and social functioning for a minimum period
of30daystotheextentthatpermanentsupervisionorassistancebya
third party is required.
Socialfunctioningisdenedastheabilityoftheindividualtointeractin
the normal or usual way in society.
Mental functioning would mean functions /processes which we can do
with our minds.
36. TerminalIllness
An Insured Person shall be regarded as terminally ill only if he/ she is
diagnosed as suffering from a condition which, in the opinion of two
appropriate independent Medical Practitioners, is highly likely to lead
to death within 12 months from the date of the diagnosis and the
Insured Person is not receiving any active treatment for the terminal
illness, other than that of the pain relief. The terminal illness must be
diagnosedandconrmedbyMedicalPractitionersregisteredwiththe
Indian Medical Association and approved by Us.
Any claim under this benet will not impact the Sum Insured and/or
Cumulative Bonus.
Allclaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.12
C.II.2 TeleConsultation
Insured Person may avail tele-consultations with our Medical
Practitioner(s) through our network in India. These consultations would
be available through tele/chat mode.
Any claim under this benet will not impact the Sum Insured and/or
Cumulative Bonus.
Allclaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.13.
C.II.3.CumulativeBonus
a) On Sum Insured
WewillincreaseYourSumInsured@10%oftheBaseSumInsured,
as specied under Policy Schedule, at the end of every claim free
Policy Year, if the Policy is renewed with Us without any break:
a) No Cumulative Bonus will be added if the Policy is not renewed
with Us by the end of the Grace Period.
b) TheCumulativeBonuswillnotbeaccumulatedinexcessof100%of
the Sum Insured under the current Policy with Us under any
circumstances.
c) Any Cumulative Bonus that has accrued for a Policy Year will be
credited at the end of that Policy Year if the policy is renewed with
us within grace period and will be available for any claims made in
the subsequent Policy Year.
d) If a cumulative bonus has been applied and a claim is made, then in
the subsequent Policy Year We will automatically decrease the
accumulated Cumulative Bonus by same rate at which it has
accrued i.e.@10% of the Base Sum Insured. There will be no
impact on the Base Sum In sured, only the accumulated Cumulative
Bonus will be reduced.
e) IfaclaimismadeintheexpiringPolicyYear,andisnotiedtous
after the acceptance of Renewal premium, in such cases any
awarded Cumulative Bonus shall be withdrawn.
f) Reduction in Sum Insured: If the Sum Insured has been reduced at
the time of Renewal, the applicable Cumulative Bonus shall be
calculated on the revised Sum Insured on pro-rata basis.
g) Increase in Sum Insured: If the Sum Insured under the Policy has
been increased at the time of Renewal the Cumulative Bonus shall
be calculated on the Sum Insured of the last completed Policy Year.
h) This clause does not alter Our right to decline a Renewal or
cancellation of the Policy for reasons as mentioned under Section
F.I.6
C.II.4 WellnessProgram
Whocanavailthesewellnessprograms:
If You have been suffering from one or more of the following conditions
such as Asthma, Diabetes, Hypertension, Dyslipidaemia, Obesity and
thesamehasbeendeclared/identiedatthetimeofbuyingthepolicy
or subsequently in any policy year, You can be a part of Wellness
Program based on the covered conditions as per the applicability of the
opted plan and earn rewards based on adherence to program metrics.
The details of the Wellness Programs are as below:
PlanType ActivePlan
Wellness Program Condition Management Program
Conducted By ManipalCigna along with its Network Partners
Program Compo-
nents
- Health Risk Assessment
- Baseline assessment (Medical test)
- Coaching by experts
- Improvement assessment (Medical test)
Medical Tests
Diabetes HbA1c+Lipidprole+Serumcreatinine+Microal-
buminuria + MER + Ophthalmologist Consultation
+ ECG
Hypertension Lipidprole+Serumcreatinine+Microalbuminuria
+ Uric acid + MER + ECG
Obesity Lipidprole+Serumcreatinine+ThyroidProle+
HbA1c + MER
Dyslipidaemia Lipidprole+Serumcreatinine+HbA1c+MER
Asthma MER + Spirometry
More than 1
disease
Combination of tests pertaining to each condition
(No repetition of tests)
Program Metric - Health Risk Assessment completion
- Medical tests undertaken at the beginning of the
program in the policy year
- Coaching completion
- Improvements achieved at the end of the program
in the policy year
Reward Accrual
– 1 year Policy
Tenure
(Refer Annexure
A for illustration,
provided as part
ofthebenet)
Maximum reward points which could be accrued is
upto15%oftheexistingbasepremium(excluding
Premium for optional cover(s), Rider(s) and taxes)
applicable for the respective insured
Reward Accrual
– 2/3 years Policy
Tenure
(Refer Annexure
A for illustration,
provided as part
ofthebenet)
Maximum reward points which could be accrued is
upto15%oftheapplicableexistingbasepremium
for the respective policy year (excluding Premium
for optional cover(s), Rider(s) and taxes)
Applicable for the respective insured, earned each
policy year and shall be accumulated till the next
renewal
In order to be eligible for the rewards, You shall adhere to all the
components of the programs as specied under program metric, as
per the applicability of opted plan.
At the end of the policy year, ‘Health Scores’ shall be calculated based
on the nal test values and improvement in health parameters
(wherever applicable). Thereafter, ‘Weighted Health Score’ shall be
calculated provided there was no hospitalization during the Policy
Period for the covered conditions and/or its complications.
RewardAccrualMethodologyunderActivePlan:
Disease-wiseHealthScoreforActivePlan:
Final Test Values and Improvement will be considered for health score
allocation.
Diabetes:
Diabetes
(HbA1c
Final Test
Value)
<or=
6.5%
Final value <or=6.5
Health Score 100
>6.5% Final Value
Reduced by
(improvement by)
0.50% 0.51%
to1%
>1%
Health Score 25 50 75
Reward Principle:
1. Reward points will be allocated for improvement in HbA1C values
only
2. No rewards will be allocated for increase in HbA1c value or

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
reduction<0.5%(forHbA1c>6.5)
3. Eligible for rewards provided there is no hospitalization for
diabetes or its complications
Hypertension:
Hyperten-
sion
(SBP/
DBP
Final Test
Value)
SBP<or=140
mm Hg
andDBP<or=
90mmHg
(AND)
Final value SBP<or=140andDBP
<or=90
Health
Score
100
SBP>140mm
Hg and /or
DBP>90mm
Hg (AND / OR)
Final Value
Reduced by
(improve-
ment by)
5 mm
Hg
6to10
mm Hg
>10
mm
Hg
Health
Score
25 50 75
Reward Principle:
1. Reward points will be allocated for improvement in BP values only
2. Increase in any one marker (SBP/DBP) will disqualify the rewards
3. No rewards will be allocated for improvement in BP values <5 mm
Hg(forSBP>140mmHgand/orDBP>90mmHg)
4. Eligible for rewards provided there is no hospitalization for
hypertension or its complications
Obesity:
Obesity
(BMI)
Final BMI
upto 29
Final value BMI upto 29
Health Score 100
Final BMI
above 29
Final Value Reduced
by (improvement by)
1 >1 to 2 >2
Health Score 25 50 75
Reward Principle:
1. Reward points will be allocated for improvement in BMI values only
2. No rewards will be allocated for increase in BMI value and reduction
in BMI <1 (for Final BMI above 29)
3. Eligible for rewards provided there is no hospitalization for obesity
or its complications
Dyslipidaemia:
Dyslipi-
daemia
Total
Cho-
lesterol
(TC) and
Triglycer-
ides (TG)
TCupto200
and TG upto
150
Final value TCupto200and
TGupto150
Health Score 100
TC>200
and/or TG >
150
Final Value Reduced
by (improvement by)
20 21
to
40
>40
Health Score 25 50 75
Reward Principle:
1. Reward points will be allocated for improvement in both TC and TG
value only
2. Increase in any one marker (TC / TG) will disqualify the rewards
3. No rewards will be allocated for increase in TC and TG and
reductioninTCand/orTGvalues<20mg/dl(forTC>200and/or
TG>150)
4. Eligible for rewards provided there is no hospitalization for
Dyslipidaemia or its complications
Asthma:
Asthma Treatment
type
Final
Value
On oral
medications
except
steroids/
immunodi-
lators
On Inhal-
ers
Not on
treat-
ment
Health
Score
50 75 100
Reward Principle:
1. Reward points will be allocated for improvement or status quo in
type of treatment only
2. No rewards will be allocated for change in line of treatment to a
higher category
3. Hierarchy for type of treatment: Category 1:Not on treatment;
Category 2: On Inhalers; Category 3: On oral medications;
Category 4: On steroids/immunomodilators
4. Eligible for rewards provided there is no hospitalization for asthma
or its complications
HealthScoreandRewardAllocation:
a. Health Score will be allocated against the nal value of each
ailment
b. In case of more than one ailment, a weighted average of all health
scores will be calculated. The weights will be assigned for
ailments in decreasing order as follows: Diabetes, Hypertension,
Obesity, Dyslipidaemia, Asthma
RewardAllocationGrid:
Weighted Health Score <25 >25to50 >50to75 >75
Rewards-%ofpremium
paid (Excluding Optional
Covers/Rider and taxes) in
the existing Policy
0% 5% 10% 15%
Conditionsunderthisbenet:
i. The reward points earned will be at eligible member level.
ii. Maximum reward points that can be earned in a single Policy Year
willbelimitedto15%ofpremiumpaid(excludingOptionalcovers,
Riders and taxes) in the existing Policy. In case of 2 or 3 year
policies, maximum reward points that can be earned shall not
exceed15%ofthetotalpremiumpaid(excludingOptionalcovers,
Riders and taxes) for 2 years or 3 years as applicable.
iii. Each earned reward point will be valued at 1 Rupee. Accrued
rewards can be redeemed against payable premium (excluding
premium for Optional covers, Riders and Taxes) from 1st Renewal
of the Policy.
iv. The earned reward points can be utilized as Discount in the renewal
premium falling due immediately after the accrual. Carry forward of
earned reward points shall not be allowed.
v. Redemption against renewal premium will be available only at the
time such renewal is due. Any earned rewards will lapse at the end
of the grace period if the policy is not renewed with us.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Refer Annexure- A below on the Illustration of Reward Points.
Annexure–A–IllustrationofRewardPoints
ReductionofRenewalPolicyYear
PolicyTerm-3years
(Premium indicated here is just for illustration purposes in case of 1
Adult policy and may not be the actual premium.)
Each earned reward point will be valued at 1 Rupee
Year Premi-
umPaid
(Excluding
Optional
covers,
Riderand
taxes)
Weight-
ed
Health
Score
Re-
ward
%
RewardPoints
Earned
Year 1 10000 80 15% 1500
Year 2 11000 78 15% 1650
Year 3 12000 65 10% 1200
Total 33000
4350
The earned reward points could be redeemed as discount as per
the below process to pay a portion of the renewal premium
RenewalofPolicyasperbelowtable
IfRenewed
Policy
Termis
Renewal
Premium
(Excluding
Optional
Covers,
Riderand
taxes)
Rewarddiscount
utilized
RenewalPre-
miumPayable
afteradjusting
Rewarddis-
count
1 Year
Policy
13000 1450(4350*1/3as
Insured is renew-
ing 3 Year policy to
1 Year Policy)
11550
2 Years
Policy
27000 2900(4350*2/3as
Insured renewing
3 Year policy to 2
Year Policy)
24100
3 Years
Policy
42000 4350(Insured
renewing to the
same policy tenure
of 3 years)
37650
IncreaseofRenewalPolicyYear
PolicyTerm-1year
(Premium indicated here is just for illustration purposes and may
not be the actual premium.)
Each earned reward point will be valued at 1 Rupee
Year Premium
(Ex-
cluding
Optional
Cover,
Riderand
taxes)
Weighted
Health
Score
Rewards% Points
Earned
Year 1 10000 40 5% 500
Total 10000 500
The earned reward points could be redeemed as discount as per
the below process to pay a portion of the renewal premium
RenewalofPolicyasperbelowtable
IfRenewed
Policy
Termis
Renewal
Premium
(Ex-
cluding
Optional
Cover/
Riderand
taxes)
Rewardsdiscount
utilized
Renewal
Premium
Payable
after
adjusting
Rewards
discount
1 Year
Policy
11000 500(asInsuredisre-
newing 1 Year policy to 1
Year Policy)
10500
2 Year
Policy
21000 500(asInsuredisre-
newing 1 Year policy to 2
Year Policy)
20500
3 Year
Policy
33000 500(asInsuredisre-
newing 1 Year policy to 3
Year Policy)
32500
The notications related to wellness programs will be communicated via
SMS, email and the program specic phone / web application. Details
about reward points will be available on the program app (if any) or would
be shared through SMS and/or Renewal Notice which would be sent to
customers.
C.II.5 DiscountfromNetworkProviders
The Insured Person can avail discount on Diagnostic, Pharmacy
and Health Supplements offered through Our Network Providers.
C.II.6 PremiumWaiverBenet
In case, the Policyholder who is also an Insured Person under the
Policy suffers Death due to an injury caused by an Accident within
365 days from the date of the event or he/she is diagnosed with a
Critical Illness, listed under this section, We will pay the next one full
Policy Year’s Renewal Premium (including Optional covers, Riders and
Taxes) of the Policy, for a policy tenure of 1 year. The premium shall be
paid towards existing Insured Persons covered under the same policy,
withbenetssameastheexpiringPolicy.
IncaseofanychangeinPolicybenets,completepremiumwillbepaid
by the Policyholder.
The cover is available subject to below conditions:
• If only one person is covered under the Policy, policy will not be
renewed in case of death of the Policyholder.
• The Policyholder is not added in the Policy in the middle of the
PolicyYear. There is no change in covers, Sum Insured, benet
structure, limits and conditions applicable under the Policy, at the
time of renewal.
• No new member is being added under the renewed Policy.
• In case of a policy with existing tenure of 2 or 3 years, it will be
renewed only for one year, provided all the terms and conditions,
benetsandpolicylimitsremainsame.
Forthepurposeof this benet, CriticalIllnessesshallincludeas
below-
1. CancerofSpeciedSeverity
2. MyocardialInfarction(FirstHeartAttackofSpecicSeverity)
3. Open Chest CABG

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
4. Open Heart Replacement or Repair of Heart Valves
5. ComaofSpeciedSeverity
6. Kidney Failure Requiring Regular Dialysis
7. Stroke Resulting in Permanent Symptoms
8. Major Organ/Bone Marrow Transplant
9. Permanent Paralysis of Limbs
10.MotorNeuronDiseasewithPermanentSymptoms
11. Multiple Sclerosis with Persisting Symptoms
Onceaclaimhasbeenacceptedandpaidunderthisbenet,this
cover will automatically terminate in respect of that Insured Person.
AnyclaimunderthisbenetwillnotimpacttheSumInsuredand/or
Cumulative Bonus.
C.III.Optionalcovers
The following optional covers shall apply under the Policy for an
Insured Person if specically mentioned on the Schedule and shall
apply to all Insured Persons under a single policy without any individual
selection.
C.III.1 Non-MedicalItems
We will cover the cost of Non-Medical items, listed under Annexure III
List 1 of the Policy, incurred towards Medically Necessary
Hospitalization of the insured person, arising out of Disease/ Illness or
Injury.
The cover is available subject to the claim being admissible under
Section D.I.1 In-patient Hospitalization and/ or Section D.I.4 Day Care
Treatment cover under this policy and the expenses on Non-medical
items are related to the same Illness/ Injury.
ExclusionE.II.13shallnotbeapplicableforthisbenet.
Any claim made under this optional benet will reduce the Sum
Insured.
Allclaimsunderthisbenetcanbemadeaspertheprocessdened
under Section G.I.4 & G.I.5.
C.III.2.WaiverofMandatoryCo-pay
The Policyholder shall have an option to remove the Mandatory Co-
paymentwhichisapplicableforallinsuredpersonsasspeciedunder
section F.II.6 and available on payment of additional premium.
C.III.3 WorldwideAccidentalEmergencyHospitalizationCover:
We will cover Medical Expenses incurred during the Policy Year, for
Emergency In-patient Hospitalization Treatments of the Insured
Person, due to an Injury arising out of an Accident, incurred outside
India,covereduptotheSum Insured and as specied inthePolicy
Schedule, provided that:
(a)The treatment is Medically Necessary and has been certied as
an Emergency by a Medical Practitioner, where such treatment
cannot be postponed until the Insured Person has returned to India
and is payable under Section D.I.1 In-patient Hospitalization of the
Policy.Ourmaximumliabilityunderthisbenet,inasinglePolicy
Year shall not exceed the limit available under this cover age and
asspeciedinthePolicySchedule.
(b) The Medical Expenses payable shall be limited to In-patient
Hospitalization only.
(c)AnypaymentunderthisbenetwillonlybemadeinIndia,inIndian
rupees on a re-imbursement basis and subject to availability of
limits under this coverage. Insured Person can contact Us at the
numbers provided on the Health Card for any claim assistance.
(d) Thepaymentofanyclaimunderthisbenetwillbebasedonthe
rate of exchange as on the date of payment to the Hospital
published by Reserve Bank of India (RBI) and shall be used for
conversion of foreign currency into Indian rupees for payment of
claim.You further understand and agree that where on the date of
discharge, if RBI rates are not published, the exchange rate next
published by RBI shall be considered for conversion.
(f) You have given Us, intimation of such hospitalization within 48
hours of admission.
(g)Any claim made under this benet will be as per the claims
procedure provided under Clause G.I.5 & G.I.14 of this Policy.
(h)Anyclaim payableunderthisbenetis overandabovetheSum
Insured.
(i) ExclusionE.II.8doesnotapplytothisbenet.
(j) RestorationofSumInsuredshallnotbeavailableunderthisbenet
(k) This cover is available to all Insured Persons provided they are
Indian resident at inception of the Policy and at subsequent
renewals of this Policy.
C.III.4 HealthCheckUp
(a) Health Check Up benet can be availed only in case where the
WellnessBenetisnotchosenbytheInsuredperson.
(b) If the Insured Person has completed 18 years of Age, the Insured
Person may avail a comprehensive health check-up with Our
Network Provider as per the eligibility details mentioned in the table
below. Health Check Ups will be arranged by Us and conducted at
Our Network Providers.
(c)Thisbenetis available once every third policy year.And all the
tests must have been done on the same date
(d) Original Copies of all reports will be provided to You.
HealthCheckUp
SumInsured Agegroup Listoftests–Cashless
For All Sum
Insured
Upto40Years ECG,FBS,LipidProle,
Sr. Creatinine, CBC-ESR,
SGOT, SGPT, GGT, TSH,
USG - Abdomen & pelvis
Above40
years
ECG,FBS,LipidProle,
Sr. Creatinine, CBC-ESR,
SGOT, SGPT, GGT, HbA1c,
USG Abdomen & Pelvis,
PSA (for Males)/ Mammogram/
PAP Smear (for females)
Full explanation of Tests is provided here: FBS - Fasting Blood
Sugar, ECG - Electrocardiogram, CBC-ESR - Complete Blood Count-
Erythrocyte Sedimentation Rate, Sr. Creatinine - Serum Creatinine,
HbA1c - Glycosylated Hemoglobin, SGOT - Serum Glutamate
oxaloacetate transaminase, SGPT - Serum Glutamate Pyruvate
Transaminase, GGT - Gamma Glutamyl Transferase, PSA - Prostate
Specic Antigen, USG - Ultrasound Sonography, TSH - Thyroid
Stimulating Hormone, CBC - Complete Blood Count
(e) Thisbenetshallbeoverandabovethesuminsured.
(f) Opting this cover shall mean that the coverage under section D.II.4
Wellness Program shall not be applicable for the Insured members
for the lifetime of the Policy. The Insured members shall not be able
to participate in any of the wellness programs and shall not be able
to earn any rewards under the coverage section D.II.4 Wellness
Program.
(g) We shall cover Health Check Up only on cashless basis within
MCHI Network.
(h)ThisbenetshallonlybeoptedatthetimeofrenewalofthePolicy
or at inception and once opted, cannot be removed.
(i) RestorationofSumInsuredshallnotbeavailableunderthisbenet
(j) All Claims under this benet can be made as per the process
denedunderSectionG.I.13&G.I.5
C.III.5 WaiverofDiseaseSpecicSublimit
ThePolicyholdershallhaveanoptiontoremovetheDiseaseSpecic
Sublimitwhichisapplicableforlistedailments/proceduresasspecied
under section D.I.1 and available on payment of additional premium.
D. Exclusions
We shall not be liable to make any payment under this Policy caused
by, based on, arising out of or howsoever attributable to any of the
followingunlessotherwisecoveredorspeciedunderthePolicyorany
Cover opted under the Policy. All the waiting period shall be applicable
individually for each Insured Person and claims shall be assessed
accordingly.
D.I.StandardExclusions
D.I.1.Pre-existingDisease-Code-Excl.01
a. Expenses related to the treatment of a Pre-existing Disease (PED) and

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
its direct complications shall be excluded until the expiry of 24 months
ofcontinuouscoverageafterthedateofinceptionoftherstpolicywith
Us.
b. In case of enhancement of sum insured the exclusion shall apply afresh
to the extent of sum insured increase.
c. If the Insured Person is continuously covered without any break as
dened under the portability norms of the extant IRDAI (Health
Insurance) Regulations then waiting period for the same would be
reduced to the extent of prior coverage.
d. Coverage under the policy after the expiry of Pre-existing disease
waiting period for any pre-existing disease is subject to the same being
declared at the time of application and accepted by us.
Any condition or illness, complication or ailment as specied in the
Policy Schedule out of any of the below mentioned conditions, shall not
be considered as part of this waiting period. Wherein, they shall be
coveredafterthe rst90daysfrom theInceptionDateof rstpolicy
with Us.
a. Asthma
b. Diabetes
c. Dyslipidaemia
d. Obesity
e. Hypertension
D.I.2.Specieddisease/procedureWaitingPeriod-Code-E.I.2
a. Expenses related to the treatment of the listed Conditions, surgeries/
treatments shall be excluded until the expiry of 24 months of continuous
coverage after the date of inception of the rst policy with us. This
exclusion shall not be applicable for claims arising due to an accident.
b. In case of enhancement of sum insured the exclusion shall apply afresh
to the extent of sum insured increase.
c. Ifanyofthespecieddisease/procedurefallsunderthewaitingperiod
speciedforpre-Existingdiseases,thenthelongerofthetwowaiting
periods shall apply.
d. The waiting period for listed conditions shall apply even if contracted
afterthepolicyordeclaredandacceptedwithoutaspecicexclusion.
e. If the Insured Person is continuously covered without any break as
denedundertheapplicablenormsonportabilitystipulatedbyIRDAI,
then waiting period for the same would be reduced to the extent of prior
coverage.
f. Listofspecicdiseases/procedures:
i. Cataract,
ii. Hysterectomy for Menorrhagia or Fibromyoma or prolapse of
Uterus or myomectomy for broids unless necessitated by
malignancy,
iii. Knee Replacement Surgery (other than caused by an Accident),
Non-infectious Arthritis, Gout, Rheumatism, Oestoarthritis and
Osteoposrosis, Joint Replacement Surgery (other than caused by
Accident), Prolapse of Intervertibral discs (other than caused by
Accident), all Vertibrae Disorders, including but not limited to
Spondylitis, Spondylosis, Spondylolisthesis, Congenital Internal,
iv. Varicose Veins and Varicose Ulcers,
v. Stones in the urinary uro-genital and biliary systems including
calculus diseases and complications thereof,
vi. Benign Prostate Hypertrophy, all types of Hydrocele,
vii. Fissure, Fistula in anus, Piles, all types of Hernia, Pilonidal sinus,
Hemorrhoids and any abscess related to the anal region.
viii. Chronic Suppurative Otitis Media (CSOM), Deviated Nasal
Septum, Sinusitis and related disorders, Surgery on tonsils/
Adenoids, Tympanoplasty and any other benign ear, nose and
throat disorder or surgery.
ix. gastric and duodenal ulcer, any type of Cysts/Nodules/Polyps/
internal tumors / skin tumors, and any type of Breast lumps (unless
malignant), Polycystic Ovarian Diseases,
x. Any surgery of the genito-urinary system unless necessitated by
malignancy.
If these diseases are pre-existing at the time of proposal or
subsequently found to be pre-existing the highest between the
Specied disease/procedure Waiting Period or Pre-existing
Diseases waiting period as mentioned in the Policy Schedule shall
apply.
D.I.3.30daysWaitingPeriod-Code-E.I.3
a) Expenses related to the treatment of any illness within 30 days of
continuouscoveragefromtherstpolicycommencementdateshallbe
excluded except claims arising due to an accident, provided the same
are covered.
b) This exclusion shall not, however, apply if the Insured Person has
Continuous Coverage for more than twelve months.
c) The within referred waiting period is made applicable to the enhanced
sum insured in the event of granting higher sum insured subsequently
D.I.4.Investigation&Evaluation-Code-Excl04
a. Expenses related to any admission primarily for diagnostics and
evaluation purposes only are excluded.
b. Any diagnostic expenses which are not related or not incidental to the
current diagnosis and treatment are excluded.
D.I.5.RestCure,rehabilitationandrespitecare-Code-Excl05
a) Expenses related to any admission primarily for enforced bed rest and
not for receiving treatment. This also includes:
i. Custodial care either at home or in a nursing facility for personal
care such as help with activities of daily living such as bathing,
dressing, moving around either by skilled nurses or assistant or
non-skilled persons.
ii. Any services for people who are terminally ill to address physical,
social, emotional and spiritual needs.
D.I.6.Obesity/WeightControlCode-Excl06
Expensesrelatedtothesurgicaltreatmentofobesitythatdoesnotfull
all the below conditions:
1. Surgery to be conducted is upon the advice of the Doctor
2. The surgery/Procedure conducted should be supported by clinical
protocols
3. The member has to be 18 years of age or older and
4. Body Mass Index (BMI);
a. greaterthanorequalto40or
b. greater than or equal to 35 in conjunction with any of the
following severe comorbidities following failure of less invasive
methods of weight loss:
i. Obesity-related cardiomyopathy
ii. Coronary heart disease
iii. Severe Sleep Apnea
iv. Uncontrolled Type 2 Diabetes
D.I.7.Change-of-GendertreatmentsCode-Excl07
Expenses related to any treatment, including surgical management, to
change characteristics of the body to those of the opposite sex.
D.I.8.CosmeticorPlasticSurgeryCode-Excl08
Expenses for cosmetic or plastic surgery or any treatment to change
appearance unless for reconstruction following an Accident, Burn (s) or
Cancer or as part of medically necessary treatment to remove a direct
and immediate health risk to the insured. For this to be considered a
medical necessity, it must be certied by the attending Medical
Practitioner.
D.I.9.HazardousorAdventuresportsCode-Excl09
Expenses related to any treatment necessitated due to participation
as a professional in hazardous or adventure sports, including but not
limited to, para-jumping, rock climbing, mountaineering, rafting, motor
racing, horse racing or scuba diving, hand gliding, sky diving, deep-sea
diving.
D.I.10.BreachoflawCode-Excl10
Expenses for treatment directly arising from or consequent upon any
Insured Person committing or attempting to commit a breach of law
with criminal intent.
D.I.11.ExcludedProvidersCode-Excl11
Expenses incurred towards treatment in any hospital or by any Medical
PractitioneroranyotherproviderspecicallyexcludedbytheInsurer
and disclosed in its website / notied to the policyholders are not

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
admissible. However, in case of life threatening situations or following
an accident, expenses up to the stage of stabilization are payable but
not the complete claim.
D.I.12. Treatment for Alcoholism, drug or substance abuse or any addictive
condition and consequences thereof. Code-Excl12
D.I.13. Treatments received in heath hydros, nature cure clinics, spas or
similar establishments or private beds registered as a nursing home
attached to such establishments or where admission is arranged
wholly or partly for domestic reasons. Code-Excl13
D.I.14. Dietary supplements and substances that can be purchased
without prescription, including but not limited to Vitamins, minerals
and organic substances unless prescribed by a Medical Practitioner
as part of hospitalization claim or day care procedure.
Code-Excl14
D.I.15.RefractiveErrorCode-Excl15
Expenses related to the treatment for correction of eye sight due to
refractive error less than 7.5 dioptres.
D.I.16.UnprovenTreatmentsCode-Excl16
Expenses related to any unproven treatment, services and
supplies for or in connection with any treatment. Unproven
treatments are treatments, procedures or supplies that lack
signicantmedicaldocumentationtosupporttheireffectiveness.
D.II.SpecicExclusions
D.II.1.PersonalWaitingperiod
A special Waiting Period not exceeding 48 months, may be applied
to individual Insured Persons for the list of acceptable Medical
Ailments listed under the Underwriting Manual of the Product,
depending upon declarations on the proposal form and existing
healthconditions.Suchwaitingperiodsshallbespecicallystated
intheScheduleandwillbeappliedonlyafterreceivingYourspecic
consent.
D.II.2. Dental Treatment, orthodontic treatment, dentures or Surgery of any
kind unless necessitated due to an Accident and requiring minimum 24
hours Hospitalization. Treatment related to gum disease or tooth
disease or damage unless related to irreversible bone disease
involving the jaw which cannot be treated in any other way, unless
specicallycoveredunderthePolicy.
D.II.3. Circumcision unless necessary for treatment of a disease, illness or
injury not excluded hereunder or due to an accident.
D.II.4. Instrument used in treatment of Sleep Apnea Syndrome (C.P.A.P.)
and Continuous Peritoneal Ambulatory Dialysis (C.P.A.D.) and
Oxygen Concentrator for Bronchial Asthmatic condition, Infusion
pump or any other external devices used during or after treatment.
D.II.5. External Congenital Anomaly or defects or any complications or
conditions arising therefrom.
D.II.6. Prostheses, corrective devices and medical appliances, which are
not required intra-operatively for the disease/ illness/ injury for which
the Insured Person was Hospitalised.
D.II.7. Any stay in Hospital without undertaking any treatment or any other
purpose other than for receiving eligible treatment of a type that
normally requires a stay in the hospital.
D.II.8 Treatment received outside India other than for coverage under
Worldwide Accidental Emergency Hospitalization Cover (if opted).
D.II.9. Costs of donor screening or costs incurred in an organ transplant
surgery involving organs not harvested from a human body.
D.II.10. Any form of Non-Allopathic treatment (except AYUSH In-patient
Treatment),Hydrotherapy,Acupuncture,Reexology,Chiropractic
treatment or any other form of indigenous system of medicine.
D.II.11. All Illness/expenses caused by ionizing radiation or contamination
by radioactivity from any nuclear fuel (explosive or hazardous form) or
from any nuclear waste from the combustion of nuclear fuel nuclear,
chemical or biological attack or in any other sequence to the loss.
D.II.12. All expenses caused by or arising from or attributable to foreign
invasion, act of foreign enemies, hostilities, warlike operations
(whether war be declared or not or while performing duties in the
armed forces of any country), participation in any naval, military
or air-force operation, civil war, public defense, rebellion, revolution,
insurrection, military or usurped power, active participation in riots,
conscation or nationalization or requisition of or destruction of
or damage to property by or under the order of any government or
local authority.
D.II.13. All non-medical expenses including convenience items for personal
comfort not consistent with or incidental to the diagnosis and
treatment of the disease/illness/injury for which the Insured Person
was hospitalized - belts, collars, splints, slings, braces, stockings of
any kind, diabetic footwear, thermometer and any medical
equipment that is subsequently used at home except when they
form part of room expenses, procedure charges and cost of
treatment.For complete list of Non-medical expenses, please refer
to the Annexure III List – I “Items for which Coverage is not available
in the Policy”
D.II.14. Any percentage of admissible claim under co-payment if applicable
andasspeciedinthePolicySchedule.
D.II.15. Existing diseases disclosed by the Insured Person (limited to the
extent of the ICD codes mentioned in line with Chapter IV,
Guidelines on Standardization of Exclusions in Health Insurance
Contracts,2019),providedthesameisappliedattheunderwriting
and consented by You/ Insured Person.
E. GeneralTermsandClauses
E.I. StandardGeneralTermsandClauses
E.I.1. DisclosureofInformation
The Policy shall be null and void and all premium paid thereon shall be
forfeited to the Company in the event of misrepresentation, mis-
description or non-disclosure of any material fact by the policyholder.
(“Material facts” for the purpose of this policy shall mean all relevant
information sought by the company in the proposal form and other
connected documents to enable it to take informed decision in the
context of underwriting the risk)
E.I.2. ConditionPrecedenttoAdmissionofLiability
The terms and conditions of the Policy must be fullled by the
Insured Person for the Company to make any payment for claim (s)
arising under the policy.
E.I.3. ClaimSettlement(provisionforPenalInterest)
i. The Company shall settle or reject the claim, as the case may be, within
30daysfromthedateofreceiptoflastnecessarydocument.
ii. In the case of delay in the payment of a claim, the Company shall be
liable to pay interest to the policyholder from the date of receipt of last
necessarydocumenttothedateofpaymentofclaimatarate2%above
the bank rate.
iii. However, where the circumstances of a claim warrant an investigation
in the opinion of the Company, it shall initiate and complete such
investigationattheearliest,inanycasenotlaterthan30daysfromthe
date of receipt of last necessary document. In such cases, the
Company shall settle or reject the claim within 45 days from the date of
receipt of last necessary document.
iv. In case of delay beyond stipulated 45 days, the Company shall be liable
topayinteresttothepolicyholderatarate2%abovethebankratefrom
the date of receipt of last necessary document to the date of payment
of claim.
“Bank rate” shall mean the rate xed by the Reserve Bank of lndia
(RBl)atthebeginningofthenancial yearinwhichclaimhas fallen
due.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
E.I.4. CompleteDischarge
Any payment to the policyholder, insured person or his/her nominees or
his/her legal representative or assignee or to the Hospital, as the case
may be, for any benet under the policy shall be a valid discharge
towards payment of claim by the Company to the extent of that amount
for the particular claim.
E.I.5. MultiplePolicies
- In case of multiple policies taken by an insured person during a period
from one or more insurers to indemnify treatment costs, the insured
person shall have the right to require a settlement of his/her claim in
terms of any of his/her policies. In all such cases, the insurer chosen by
the insured person shall be obliged to settle the claim as long as the
claim is within the limits of and according to the terms of the chosen
policy.
- Insured person having multiple policies shall also have the right to
prefer claims under this policy for the amounts disallowed under any
other policy / policies even if the sum insured is not exhausted. Then
the insurer shall independently settle the claim subject to the terms and
conditions of this policy.
- If the amount to be claimed exceeds the sum insured under a single
policy, the insured person shall have right to choose insurer from whom
he/she wants to claim the balance amount.
- Where an insured person has policies from more than one insurer to
cover the same risk on indemnity basis, the insured person shall only
beindemniedthetreatmentcostsinaccordancewiththetermsand
conditions of the chosen policy.
E.I.6. Fraud
If any claim made by the insured person, is in any respect fraudulent,
or if any false statement, or declaration is made or used in support
thereof, or if any fraudulent means or devices are used by the insured
personoranyoneactingonhis/herbehalftoobtainanybenetunder
thispolicy,allbenetsunderthispolicyshallbeforfeited.
Any amount already paid against claims made under this policy
but which are found fraudulent later shall be repaid by all recipient(s) /
policyholder(s), who has made that particular claim, who shall be
jointly and severally liable for such repayment to the Insurer.
For the purpose of this clause, the expression “fraud” means any of
the following acts committed by the Insured Person or by his agent or
the hospital / doctor / any other party acting on behalf of the insured person,
with intent to deceive the insurer or to induce the insurer to issue an
insurance Policy
a) the suggestion, as a fact of that which is not true and which the
Insured Person does not believe to be true;
b) the active concealment of a fact by the Insured Person having
knowledge or belief of the fact;
c) anyotheractttedtodeceive;and
d) any such act or omission as the law specially declares to be
fraudulent
The company shall not repudiate the claim and / or forfeit the policy
benets on the ground of Fraud, if the insured person / beneciary
can prove that the misstatement was true to the best of his knowledge
and there was no deliberate intention to suppress the fact or that such
mis-statement of or suppression of material fact are within the
knowledge of the insurer.
E.I.7. Cancellation
i. The policyholder may cancel this policy by giving 15 days written notice
and in such an event, the Company shall refund premium for the
unexpired policy period as detailed below.
RefundGridasa%ofPremium
PolicyCancelation
Within(Days)
PolicyYear-1
Policy
Year-2
Policy
Year-3
0-30Days 85.00% 87.50% 89.00%
31-90Days 75.00% 80.00% 82.50%
91 - 181 Days 50.00% 70.00% 75.00%
182 - 272 Days 30.00% 60.00% 70.00%
273 - 365 Days 0.00% 50.00% 60.00%
366 - 456 Days
NIL
35.00% 55.00%
457 - 547 Days 25.00% 45.00%
548 - 638 Days 15.00% 40.00%
639-730Days 0.00% 30.00%
731 - 821 Days
NIL
25.00%
822 - 912 Days 15.00%
913-1003Days 5.00%
1004andmore
Days
0.00%
No refund will be processed for cancellation of policies with Premium
Payment Mode as Half-yearly, Quarterly or Monthly.
Notwithstanding anything contained herein or otherwise, no refunds of
premium shall be made in respect of Cancellation where, any claim has
beenadmittedorhasbeenlodgedoranybenethasbeenavailedby
the insured person under the policy.
ii. The Company may cancel the policy at any time on grounds of
misrepresentation, non- disclosure of material facts, fraud by
the insured person by giving 15 days written notice. There would
be no refund of premium on cancellation on grounds of
misrepresentation, non-disclosure of material facts or fraud.
E.I.8. Migration
The Insured Person will have the option to migrate the Policy to other
health insurance products/plans offered by the company by applying
for migration of the policy at least 30 days before the policy
renewal date as per IRDAI guidelines on Migration. If such person is
presently covered and has been continuously covered without any
lapses under any health insurance product/plan offered by the
company,theInsuredPersonwillgettheaccruedcontinuitybenetsin
waiting periods as per IRDAI guidelines on migration.
For Detailed Guidelines on Migration, kindly refer IRDAI Guidelines
RefNo:IRDAI/HLT/REG/CIR/003/01/2020
E.I.9. Portability
The insured person will have the option to port the policy to other
insurers by applying to such insurer to port the entire policy along with
all the members of the family, if any, at least 45 days before, but not
earlier than 60 days from the policy renewal date as per IRDAI
guidelines related to portability. If such person is presently covered and
has been continuously covered without any lapses under any health
insurance policy with an Indian General/Health insurer, the proposed
insured person will get the accrued continuity benets in waiting
periods as per IRDAI guidelines on portability.
For detailed Guidelines on Portability, kindly refer IRDAI Guidelines Ref
No:IRDAI/HLT/REG/CIR/003/01/2020andScheduleIofIRDAI(Health
Insurance)Regulations2016forthePortabilitynorms
E.I.10. RenewalofPolicy
The policy shall ordinarily be renewable except on grounds of fraud,
misrepresentation by the insured person.
i. The Company shall endeavour to give notice for renewal. However,
the Company is not under obligation to give any notice for renewal.
ii. Renewal shall not be denied on the ground that the insured person
had made a claim or claims in the preceding policy years.
iii. Request for renewal along with requisite premium shall be received
by the Company before the end of the policy period.
iv. At the end of the policy period, the policy shall terminate and can
be renewed within the Grace Period of 30/15 days, to maintain
continuity of benets without break in policy. Coverage is not
available during the grace period.
v. No loading shall apply on renewals based on individual claims
experience.
E.I.11. WithdrawalofPolicy
i. In the likelihood of this product being withdrawn in future, the Company
willintimatetheinsuredpersonaboutthesame90dayspriortoexpiry
of the policy.
ii. Insured person will have the option to migrate to similar health

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
insurance product available with the Company at the time of renewal
with all the accrued continuity benets such as cumulative bonus,
waiver of waiting period, as per IRDAI guidelines, provided the policy
has been maintained without a break.
E.I.12. MoratoriumPeriod
After completion of eight continuous years under the policy no look
back to be applied. This period of eight years is called as moratorium
period. The moratorium would be applicable for the sums insured of the
rstpolicyandsubsequentlycompletionof8continuousyearswould
be applicable from date of enhancement of sums insured only on the
enhanced limits. After the expiry of Moratorium Period no health
insurance claim shall be contestable except for proven fraud and
permanent exclusions specied in the policy contract. The policies
would however be subject to all limits, sub limits, co-payments,
deductibles as per the policy contract.
E.I.13. PremiumPaymentinInstalments(Whereverapplicable)
If the insured person has opted for Payment of Premium on an
Instalment basis i.e. Half Yearly, Quarterly or Monthly, as mentioned in
thePolicySchedule/CerticateofInsurance,thefollowingConditions
shall apply (notwithstanding any terms contrary elsewhere in the
policy)
i. Grace Period of 30 days would be given for Half-yearly and
Quarterly mode of payment and grace period of 15 days for
monthly mode of payment would be given to pay the instalment
premium due for the Policy.
ii. During such grace period, coverage will not be available from the
due date of instalment premium till the date of receipt of premium
by Company.
iii. The insured person will get the accrued continuity benet in
respectofthe“WaitingPeriods”,“SpecicWaitingPeriods”inthe
event of payment of premium within the stipulated grace Period.
iv. No interest will be charged if the instalment premium is not paid on
due date.
v. In case of instalment premium due not received within the grace
period, the policy will get cancelled.
vi. In the event of a claim, all subsequent premium instalments shall
immediately become due and payable.
vii. The company has the right to recover and deduct all the pending
instalments from the claim amount due under the policy
E.I.14. Possibility of Revision of Terms of the Policy Including the
PremiumRates
The Company, with prior approval of IRDAI, may revise or modify the
terms of the policy including the premium rates. The insured person
shallbenotiedthreemonthsbeforethechangesareeffected.
E.I.15. FreeLookperiod
The Free Look period shall be applicable on new individual health
insurance policies and not on renewals or at the time of porting/
migrating the policy.
Theinsuredpersonshallbeallowedafreelookperiodoffteendays
from date of receipt of the policy document to review the terms and
conditions of the policy and to return the same if not acceptable.
If the insured has not made any claim during the Free Look Period, the
insured shall be entitled to
a. a refund of the premium paid less any expenses incurred by the
Company on medical examination of the insured person and the
stamp duty charges or;
b. where the risk has already commenced and the option of return
of the policy is exercised by the insured person, a deduction
towards the proportionate risk premium for period of cover or;
c. Where only a part of the insurance coverage has commenced,
such proportionate premium commensurate with the insurance
coverage during such period.
E.I.16. RedressalofGrievance
If you have a grievance that you wish us to redress, you may contact us
with the details of the grievance through:
Our website: www.manipalcigna.com
Email: [email protected],
Senior Citizens may write to us at -
TollFree:1800-102-4462
ContactNo.:+912261703600
Courier:AnyofOurBranchofceorcorporateofceduringbusiness
hours.
Insured Person may also approach the grievance cell at any of
company’s branches with the details of the grievance.
IfInsuredPersonisnotsatisedwiththeredressalofgrievancethrough
one of the above methods, insured person may contact the grievance
ofcer at, ‘The Grievance Cell, ManipalCigna Health Insurance
Company Limited, 401/402, Raheja Titanium, Western Express
Highway, Goregaon East, Mumbai - 400063, India or email -
For updated details of grievance ofcer, kindly refer link -
https://www.manipalcigna.com/grievance-redressal
IfInsuredpersonisnotsatisedwiththeredressalofgrievancethrough
abovemethods,theInsuredPersonmayalsoapproachtheofceof
Insurance Ombudsman of the respective area/region for redressal of
grievance as per Insurance Ombudsman Rules 2017. The contact
details of Ombudsman ofces attached asAnnexure I to this Policy
document.
Grievance may also be lodged at IRDAI Integrated Grievance
Management System - https://igms.irda.gov.in/
You may also approach the Insurance Ombudsman if your complaint is
openformorethan30daysfromthedateoflingthecomplaint.
E.I.17. Nomination
The policyholder is required at the inception of the policy to make a
nomination for the purpose of payment of claims under the policy in
the event of death of the policyholder. Any change of nomination shall
be communicated to the company in writing and such change shall be
effective only when an endorsement on the policy is made. In the event
of death of the policyholder, the Company will pay the nominee {as
namedinthePolicySchedule/PolicyCerticate/Endorsement(ifany)}
and in case there is no subsisting nominee, to the legal heirs or legal
representatives of the Policyholder whose discharge shall be treated as
fullandnaldischargeofitsliabilityunderthePolicy.
E.II. SpecicTermsandClauses
E.II.1. MaterialChange
Material information to be disclosed includes every matter that You are
aware of, that relates to questions in the Proposal Form and which is
relevant to Us in order to accept the risk of insurance and if so on what
terms. You must exercise the same duty to disclose those matters to Us
before the Renewal, extension, variation, endorsement or reinstatement
of the contract.
E.II.2. AlterationsinthePolicy
This Policy constitutes the complete contract of insurance. No change
or alteration will be effective or valid unless approved in writing which
will be evidenced by a written endorsement, signed and stamped by
Us.
E.II.3. ChangeofPolicyholder
The policyholder may be changed only at the time of Renewal of the
Policy. The new policyholder must be a member of the Insured Person’s
immediate family. Such change would be solely subject to Our
discretion and payment of premium by You. The renewed Policy shall
be treated as having been renewed without break.
The policyholder may be changed upon request in case of his demise,
his moving out of India or in case of divorce during the Policy Period.
E.II.4. NoConstructiveNotice
Any knowledge or information of any circumstance or condition in
relation to the Policyholder/ Insured Person which is in Our possession
andnotspecicallyinformedbythePolicyholder/InsuredPersonshall
not be held to bind or prejudicially affect Us notwithstanding
subsequent acceptance of any premium.
E.II.5. Geography
The geographical scope of this policy applies to events within India
other than for D.III.3 Worldwide Accidental Emergency Hospitalization
Cover (if opted) and which are specically covered in the Policy

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Schedule. However all admitted or payable claims shall be settled in
India in Indian rupees.
E.II.6. MandatoryCo-payment
A compulsory Co-payment of 10% is applicable on all claims
irrespective of Age of entry in to the Policy under Active Plan. Co-
payment will be applied on the admissible claim amount.
In case the claim amount is processed as per the sub-limits for the
named ailments/procedures as mentioned under section D.I.1 In-
patient Hospitalization, the Mandatory Co-payment shall not be
applicable.
E.II.7. Recordstobemaintained
You or the Insured Person, as the case may be shall keep an accurate
record containing all medical records pertaining to claim and shall allow
Us or our representative (s) to inspect such records. You or the Insured
Person as the case may be, shall furnish such information as may be
required by Us under this Policy at any time during the Policy Period
anduptothreeyearsafterthePolicyexpiration,oruntilnaladjustment
(if any) and resolution of all Claims under this Policy.
E.II.8. GracePeriod
The Policy may be renewed by mutual consent and in such event the
Renewal premium should be paid to Us on or before the date of expiry
ofthePolicyandinnocaselaterthantheGracePeriodof30daysfrom
the expiry of the Policy. We will not be liable to pay for any claim arising
out of an Illness/ Injury / Accident / Condition that occurred during the
Grace Period. The provisions of Section 64VB of the Insurance Act
shall be applicable. All policies Renewed within the Grace Period shall
be eligible for continuity of cover.
E.II.9. RenewalTerms
a. The Policy is ordinarily renewable on mutual consent for life, subject to
application of Renewal and realization of Renewal premium. The Policy
with Optional cover Worldwide Accidental Emergency Hospitalization
Cover shall be renewed subject to the Insured Person being an Indian
resident at the time of renewal.
b. We, shall not be liable for any claim arising out of an ailment suffered or
Hospitalization commencing or disease/illness/condition contracted
during the period between the expiry of previous policy and date of
inception of subsequent policy.
c. Renewals will not be denied except on grounds of misrepresentation,
moral hazard, fraud, non-disclosure of material facts or non-co-operation
by You.
d. Where We have discontinued or withdrawn this product/plan You
will have the option to renewal under the nearest substitute Policy
being issued by Us, provided however benets payable shall be
subject to the terms contained in such other policy which has been
approved by IRDAI.
e. Insured Person shall disclose to Us in writing of any material change
in the health condition at the time of seeking Renewal of this Policy,
irrespective of any claim arising or made. The terms and condition of
the existing policy will not be altered.
f. We may, revise the Renewal premium payable under the Policy or the
terms of cover, provided that all such changes are approved by IRDAI
and in accordance with the IRDAI rules and regulations as applicable
from time to time. Renewal premium will not alter based on individual
claimsexperience.WewillintimateYouofanysuchchangesatleast90
dayspriortodateofsuchrevisionormodication.
g. Alterations like increase/ decrease in Sum Insured or Change in Plan/
Product, addition/deletion of members, addition deletion of Medical
Condition existing prior to policy inception will be allowed at the time of
Renewal of the Policy. You can submit a request for the changes by
lling the proposal form before the expiry of the Policy. We reserve
Our right to carry out underwriting in relation to acceptance of request
for change of Sum Insured or addition/deletion of members, addition
deletion of Medical Condition existing prior to policy inception, on
renewal. The terms and conditions of the existing policy will not be
altered.
h. Any enhanced Sum Insured during any policy renewals will not be
available for an illness, disease, injury already contracted under the
preceding Policy Periods. All waiting periods as mentioned below shall
apply afresh for this enhanced limit from the effective date of such
enhancement.
i. Wherever the Sum Insured is reduced on any Policy Renewals, the
waiting periods shall be waived only up to the lowest Sum Insured of
the last 24 consecutive months as applicable to the relevant waiting
periods of the Plan opted.
j. Where an Insured Person is added to this Policy, either by way of
endorsement or at the time of renewal, all waiting periods under
Section E.I.1 to E.I.3 and E.II.1 will be applicable considering such
PolicyYearastherstyearofPolicywiththeCompany.
k. Applicable Cumulative Bonus shall be accrued on each renewal as per
eligibility under the plan opted.
III. You may pay the premium through Standing Instruction (SI)
providedthat:
i. Standing Instruction Mandate form is completely lled & signed
by You.
ii. The Premium amount which would be auto debited & frequency of
instalmentisdulylledinthemandateform.
iii. NewMandateFormisrequiredtobelledincaseofanychangeinthe
Policy Terms and Conditions whether or not leading to change in
Premium.
iv. You need to inform us at least 15 days prior to the due date of
instalment premium if You wish to discontinue with the Standing
Instruction facility.
Non-payment of premium on due date as opted by You in the mandate
form subject to an additional renewal/ revival period will lead to
termination of the policy.
E.II.10.Premiumcalculation
Premium will be calculated based on the Sum Insured opted, Plan,
Age,GenderandriskclassicationandZoneofCover.
All Premiums are age band based and will vary as per the change in age
group.
Premium can be paid on Single, Yearly, Half yearly, Quarterly and
Monthly basis. Premium payment mode can only be selected at the
inception of the Policy or at the renewal of the Policy.
In case of premium payment modes other than Single and Yearly, a
loading will be applied on the premium.
Loading grid applicable for Half yearly, Quarterly and Monthly payment
mode.
Premiumpaymentmode %Loadingonpremium
Monthly 5.50
Quarterly 3.50
Half yearly 2.50
ZoneClassication
ZoneI: Mumbai, Thane & Navi Mumbai, Gujarat and Delhi & NCR
ZoneII: Bangalore, Hyderabad, Chennai, Chandigarh, Ludhiana,
Kolkata, Pune
ZoneIII: Rest of India excluding the locations mentioned under
Zone I & Zone II
IdenticationofZonewillbebasedonthelocation-Cityoftheproposed
Insured Persons.
(a) Persons paying Zone I premium can avail treatment all over India
without any Co-pay.
(b) Persons paying Zone II premium
i) Can avail treatment in Zone II and Zone III without any Co-pay.
ii) AvailingtreatmentinZoneIwillhavetobear10%ofeachand
every claim.
(c) Person paying Zone III premium
i) Can avail treatment in Zone III, without any Co-pay.
ii) AvailingtreatmentinZoneIIwillhavetobear10%ofeachand
every claim.
iii)AvailingtreatmentinZoneIwillhavetobear20%ofeachand
every claim.
***OptiontoselectZone1iftheactualZoneisZone2orZone3and
would be available on payment of applicable premium at the time of
buying the First Policy and on subsequent renewals
Aforesaid Co-payments for claims occurring outside of the Zone will
not apply in case of Hospitalization due to Accident. The aforesaid
Co-payments applicable are in addition to the Mandatory Co-payment

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
under section F.II.6 and will be applied in conjunction to section F.II.6
E.II.11.DiscountsunderthePolicy
You can avail of the following discounts on the premium on Your policy.
i. LifetimeDiscounts:
a. Standing Instruction Discount: 3% discount on the renewal
premium, if the renewal premium is received through standing
instruction.
b. Long Term policy discount - Long term discount of 7.5% for
selectinga2yearpolicyand10%forselectinga3yearpolicy.This
discount is available only with ‘Single’ Premium Payment mode.
ii. ShorttermDiscounts:
a. WorksiteMarketingDiscount-Adiscountof10%willbeavailable
on polices which are sourced through worksite marketing channel.
This discount is applicable once, only at inception of the Policy.
Maximum discount applicable as per this section on a single policy
shallnotexceed40%.
E.II.12.Loadings&SpecialConditions
We may apply a risk loading on the premium payable(excluding
Statutory Levis and Taxes) or Special Conditions on the Policy based
upon the health status of the persons proposed for insurance and
declarations made in the Proposal Form.These loadings will be applied
frominceptiondateoftherstPolicyincludingsubsequentRenewal(s)
with Us. There will be no loadings based on individual claims
experience.
We may apply a specic sub-limit on a medical condition/ailment
depending on the past history and declarations or additional waiting
periods(amaximum of48months fromthedate ofinceptionof rst
policy) on pre-existing diseases as part of the special conditions on the
Policy.
We shall inform You about the applicable risk loading or special
condition through a counter offer letter or through an electronic mode,
as the case may be and You would need to revert with consent and
additionalpremium(ifany),withinthedurationspeciedinthecounter
offer letter.
In case, You neither accept the counter offer nor revert to Us within the
duration specied, We shall cancel Your application and refund the
premium paid. Your Policy will not be issued unless We receive Your
consent.
E.II.13.Communications&Notices
Any communication or notice or instruction under this Policy shall be in
writing and will be sent to:
a. Thepolicyholder’s,attheaddressasspeciedinSchedule
b. ToUs,attheaddressspeciedintheSchedule.
c. No insurance agents, brokers, other person or entity is authorised
to receive any notice on the behalf of Us unless explicitly stated in
writing by Us.
d. Notice and instructions will be deemed served 10 days after
posting or immediately upon receipt in the case of hand delivery,
facsimile or e-mail.
E.II.14.ElectronicTransactions
You agree to comply with all the terms, conditions as We shall
prescribe from time to time, and conrms that all transactions
effected facilities for conducting remote transactions such as the
internet, World Wide Web, electronic data interchange, call centres,
tele-service operations (whether voice, video, data or combination
thereof) or by means of electronic, computer, automated machines
network or through other means of telecommunication, in respect of
this Policy, or Our other products and services, shall constitute legally
binding when done in compliance with Our terms for such facilities.
Sales through such electronic transactions shall ensure that all
conditions of Section 41 of the Insurance Act, 1938 prescribed for the
proposal form and all necessary disclosures on terms and conditions
and exclusions are made known to You. A voice recording in case of
tele-sales or other evidence for sales through the World Wide Web shall
be maintained and such consent will be subsequently validated /
conrmedbyYou.
All terms and conditions in respect of Electronic Transactions shall be
within the approved Terms and Conditions of the Policy.
E.II.15.LimitationofLiability
If a claim is rejected or partially settled and is not the subject of any
pending suit or other proceeding or arbitration, as the case may be,
within twelve months from the date of such rejection or settlement, the
claim shall be deemed to have been abandoned and Our liability shall
be extinguished and shall not be recoverable thereafter.
E.II.16.TermsandconditionsofthePolicy
The terms and conditions contained herein and in the Policy Schedule
shall be deemed to form part of the Policy and shall be read together as
one document.
E.II.17.DisputeResolution
Any and all disputes or differences under or in relation to this Policy
shall be determined by the Indian Courts and subject to Indian law
without reference to any principle which would result in the application
of the law of any other jurisdiction.
F. Othertermsandconditions
F.I. Claimprocess&management
F.I.1. ConditionPreceding
ThefullmentofthetermsandconditionsofthisPolicy(includingthe
realization of premium by their respective due dates) in so far as they
relate to anything to be done or complied with by You or any Insured
Person, including complying with the following steps, shall be the
condition precedent to the admissibility of the claim.
Completed claim forms and processing documents must be furnished
to Us within the stipulated timelines for all reimbursement claims.
Failure to furnish this documentation within the time required shall not
invalidate nor reduce any claim if You can satisfy Us that it was not
reasonably possible for You to submit / give proof within such time.
The due intimation, submission of documents and compliance with
requirements as provided under the Claims Process under this Section,
by You shall be essential failing which We shall not be bound to accept
a claim.
Cashless and Reimbursement Claim processing and access to
network hospitals is through our service partner/TPA, details of the
same will be available on the Health Card issued by Us as well as on
our website. For the latest list of network hospitals you can log on to
our website. Wherever a TPA is used, the TPA will only work to facilitate
claim processing. All customer contact points will be with Us including
claim intimation, submission, settlement and dispute resolutions.
F.I.2. PolicyHolder’s/InsuredPersonsDutyatthetimeofClaim
You are required to check the applicable list of Network Providers, at
Our website or call center before availing the Cashless services.
On occurrence of an event which may lead to a Claim under this Policy,
You shall:
(a)Forthwithintimate,leandsubmittheClaiminaccordancetothe
ClaimProceduredenedunderSectionG.I.3,G.I.4,andG.I.5as
mentioned below.
(b) If so requested by Us, You or the Insured Person must submit
himself/ herself for a medical examination by Our nominated
Medical Practitioner as often as We consider reasonable and
necessary. The cost of such examination will be borne by Us.
(c) Allow the Medical Practitioner or any of Our representatives to
inspect the medical and Hospitalization records, investigate the
facts and examine the Insured Person.
(d) Assist and not hinder or prevent Our representatives in pursuance
of their duties for ascertaining the admissibility of the claim, its
circumstances and its quantum under the provisions of the Policy.
F.I.3. ClaimIntimation
Upon the discovery or occurrence of any Illness / Injury that may give
rise to a Claim under this Policy, You / Insured Person shall undertake
the following:
In the event of any Illness or Injury or occurrence of any other
contingency which has resulted in a Claim or may result in a claim
covered under the Policy, You/the Insured Person, must notify Us either
at the call center or in writing, in the event of:
• Planned Hospitalization, You/the Insured Person will intimate such
admission at least 3 days prior to the planned date of admission.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
• Emergency Hospitalization, You /the Insured Person will intimate
such admission within 48 hours of such admission.
The following details are to be provided to Us at the time of intimation
of Claim:
• Policy Number
• Name of the Policyholder
• Name of the Insured Person in whose relation the Claim is being
lodged
• Nature of Illness / Injury
• Name and address of the attending Medical Practitioner and
Hospital
• Date of Admission
• Any other information as requested by Us
F.I.4. CashlessFacility
Cashless facility is available only at our Network Hospital. The Insured
Person can avail Cashless facility at the time of admission into any
Network Hospital, by presenting the health card as provided by Us with
thisPolicy,alongwithavalidphotoidenticationproof(VoterIDcard
/ Driving License / Passport / PAN Card / any other identity proof as
approved by Us).
(a) ForPlannedHospitalization:
i. The Insured Person should at least 3 days prior to admission to the
Hospital approach the Network Provider for Hospitalization for medical
treatment.
ii. The Network Provider will issue the request for authorization letter for
Hospitalization in the pre-authorization form prescribed by the IRDA.
iii. The Network Provider shall electronically send the pre-authorization
form along with all the relevant details to the 24 (twenty four) hour
authorization/cashless department along with contact details of the
treating Medical Practitioner and the Insured Person.
iv. Upon receiving the pre-authorization form and all related medical
information from the Network Provider, We will verify the eligibility of
cover under the Policy.
v. Wherever the information provided in the request is sufcient to
ascertain the authorisation We shall issue the authorisation Letter to
the Network Provider. Wherever additional information or documents
are required We will call for the same from the Network provider and
upon satisfactory receipt of last necessary documents the authorisation
will be issued. All authorisations will be issued within a period of 4 hours
from the receipt of last complete documents.
vi. The Authorisation letter will include details of sanctioned amount, any
speciclimitationon theclaim,anyco-pays ordeductiblesandnon-
payable items if applicable.
vii. The authorisation letter shall be valid only for a period of 15 days from
the date of issuance of authorization.
In the event that the cost of Hospitalization exceeds the authorized limit
as mentioned in the authorization letter:
i. The Network Provider shall request Us for an enhancement of
authorisation limit as described under Section G.I.4 (a) including details
ofthespeciccircumstanceswhichhaveledtotheneedforincreasein
the previously authorized limit. We will verify the eligibility and evaluate
the request for enhancement on the availability of further limits.
ii. We shall accept or decline such additional expenses within 24
(twenty-four) hours of receiving the request for enhancement from You.
In the event of a change in the treatment during Hospitalization to the
Insured Person, the Network Provider shall obtain a fresh authorization
letter from Us in accordance with the process described under G.I.4 (a)
above.
At the time of discharge:
i. theNetworkProvidermayforwardanalrequestforauthorizationfor
any residual amount to us along with the discharge summary and the
billing format in accordance with the process described at G.I.4 (a)
above.
ii. Upon receipt of the nal authorisation letter from us, You may be
discharged by the Network Provider.
(b) IncaseofEmergencyHospitalization
i. The Insured Person may approach the Network Provider for
Hospitalization for medical treatment.
ii. The Network Provider shall forward the request for authorization within
48 hours of admission to the Hospital as per the process under
Section.G.I.4 (a).
iii. It is agreed and understood that we may continue to discuss the Insured
Person’s condition with the treating Medical Practitioner till Our
recommendations on eligibility of coverage for the Insured Person are
nalised.
iv. In the interim, the Network Provider may either consider treating the
Insured Person by taking a token deposit or treating him as per their
norms in the event of any lifesaving, limb saving, sight saving,
Emergency medical attention requiring situation.
v. The Network Provider shall refund the deposit amount to You barring a
token amount to take care of non-covered expenses once the pre-
authorization is issued.
Note: Cashless facility for Hospitalization Expenses shall be limited
exclusively to Medical Expenses incurred for treatment undertaken in
a Network Hospital for Illness or Injury which are covered under the
Policy and shall not be available to the Insured Person for coverage
under Worldwide Accidental Emergency Hospitalization Cover
(Section D.III.3), Convalescence Benet (Section D.I.10) and Daily
Cash for Shared Accommodation (Section D.I.11). For all Cashless
authorisations, You will, in any event, be required to settle all non-
admissible expenses, Co-payment and / or Deductibles (if applicable),
directly with the Hospital.
The Network Provider will send the claim documents along with the
invoice and discharge voucher, duly signed by the Insured Person
directly to us. The following claim documents should be submitted to
Us within 15 days from the date of discharge from Hospital -
• Claim Form Duly Filled and Signed
• Original pre-authorisation request
• Copy of pre-authorisation approval letter (s)
• CopyofPhotoIDofPatientVeriedbytheHospital
• Original Discharge/Death Summary
• Operation Theatre Notes (if any)
• Original Hospital Main Bill and break up Bill
• Original Investigation Reports, X Ray, MRI, CT Films, HPE
• Doctors Reference Slips for Investigations/Pharmacy
• Original Pharmacy Bills
• MLC/FIR Report/Post Mortem Report (if applicable and conducted)
We may call for any additional documents as required based on the
circumstances of the claim
There can be instances where We may deny Cashless facility for
Hospitalization due to insufcient Sum Insured or insufcient
information to determine admissibility in which case You/ Insured
Person may be required to pay for the treatment and submit the claim
for reimbursement to Us which will be considered subject to the Policy
Terms & Conditions.
We in our sole discretion, reserves the right to modify, add or restrict
any Network Hospital for Cashless services available under the Policy.
Before availing the Cashless service, the Policyholder / Insured Person
is required to check the applicable/latest list of Network Hospital on the
Company’s website or by calling our call centre.
F.I.5. ClaimReimbursementProcess
(a) CollectionofClaimDocuments
i. Wherever You have opted for a reimbursement of expenses, You may
submit the following documents for reimbursement of the claim to Our
branchorheadofceatyourownexpensenotlaterthan15daysfrom
the date of discharge from the Hospital. You can obtain a Claim Form
fromanyofourBranchOfcesordownloadacopyfromourwebsite
www.manipalcigna.com
ii. List of necessary claim documents to be submitted for reimbursement
are as following:
Claim form duly signed
Copy of photo ID of patient
Hospital Discharge summary
Operation Theatre notes
Hospital Main Bill
ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Hospital Break up bill
Investigation reports
Originalinvestigationreports,XRay,MRI,CTlms,HPE,ECG
Doctors reference slip for investigation
Pharmacy Bills
MLC/ FIR report, Post Mortem Report if applicable and conducted
KYC documents (Photo ID proof, address proof, recent passport
size photograph)
Cancelled cheque for NEFT payment
Payment receipt.
We may call for any additional documents/information as required
based on the circumstances of the claim.
iii. Our branch ofces shall give due acknowledgement of collected
documents to You.
In case You/ Insured Person delay submission of claim documents as
specied in G.I.5 (a) above, then in addition to the documents
mentioned in G.I.5 (a) above, You are also required to provide Us the
reason for such delay in writing. In case You delay submission of claim
documents, then in addition to the documents mentioned above, You
are also required to provide Us the reason for such delay in writing.
Wewillacceptsuchrequestsfordelayuptoanadditionalperiodof30
days from the stipulated time for such submission.We will condone
delay on merit for delayed Claims where the delay has been proved to
befor reasons beyond Your/Insured Persons control.
F.I.6. ScrutinyofClaimDocuments
a. We shall scrutinize the claim and accompanying documents. Any
deciency of documents shall be intimated to You and the Network
Provider, as the case may be within 5 days of their receipt.
b. Ifthedeciencyinthenecessaryclaimdocumentsisnotmetor are
partiallymetin10workingdaysoftherstintimation,Weshallremind
Youofthesameandevery10(ten)daysthereafter.
c. We will send a maximum of 3 (three) reminders.
d. We shall settle the claim payable amount arrived post scrutinizing the
claimdocumentsexcludingthedeciencyintimatedtoYou.
e. In case a reimbursement claim is received when a Pre-Authorization
letter has been issued, before approving such claim a check will be
made with the provider whether the Pre-authorization has been
utilized as well as whether the Policyholder has settled all the dues
with the provider. Once such check and declaration is received from
the Provider, the case will be processed.
F.I.7. ClaimAssessment
We will assess all admissible claims under the Policy in the following
progressive order -
a)
i) Where a room accommodation is opted for higher than the
eligible room category under the plan, the room rent for the
applicable accommodation will be apportioned on pro rata basis.
Such apportioned amount will apply to all “Associated Medical
Expenses”. [(a). Cost of Pharmacy & consumables, (b). Cost of
implant and medical device, (c). Cost of diagnostic test, will not be
partofassociatedmedicalexpenses)]
ii) Any Sub-limits, Mandatory or Zonal Co-payment shall be applicable
on the amount payable after applying the Section G.I.7 (i)
b) The Claim amount assessed under Section G.I.7 will be deducted from
the following amounts in the following progressive order –
i) Mandatory Co-payment
ii) Zonal Co-Payment (if applicable)
iii) Sum Insured
iv) Cumulative Bonus
v) Restored Sum Insured
Note: Wherever the disease specic Sub-limits as mentioned under
In-patient Hospitalization (section D.I.1) are applied, the Mandatory
Co-payment shall not be applicable and they are mutually exclusive.
ClaimAssessmentforBenetPlans:
WewillpayxedbenetamountsasspeciedinthePolicySchedule
in accordance with the terms of this Policy. We are not liable to make
any reimbursements of Medical Expenses or pay any other amounts
notspeciedinthePolicy.
Claimassessment forpolicies withMonthly,QuarterlyandHalf-
YearlyPremiumPaymentMode:
In case of a claim (Cashless/Re-imbursement), an amount equivalent
to the balance of the instalment premiums payable, in that policy year,
would be recoverable from the admissible claim amount payable in
respect of the Insured person.
F.I.8. ClaimsInvestigation
We may investigate claims at Our own discretion to determine the
validity of claim. Such investigation shall be concluded within 15 days
from the date of assigning the claim for investigation and not later
than30daysfromthedateofreceiptoflastnecessarydocument.
Verication carried out, if any, will be done by individuals or entities
authorisedbyUstocarryoutsuchverication/investigation(s)and
thecostsforsuchverication/investigationshallbebornebytheUs.
F.I.9. PreandPost-hospitalizationclaims
You should submit the Post-hospitalization claim documents at Your
own expense within 15 days of completion of Post-hospitalization
treatment or eligible post hospitalization period of cover, whichever is
earlier.
We shall receive Pre and Post- hospitalization claim documents either
along with the inpatient Hospitalization papers or separately and
process the same based on merit of the claim subject to Policy terms
and conditions, derived on the basis of documents received.
F.I.10. RepresentationagainstRejection:
Where a rejection is communicated by Us, You may if so desired within
15 days represent to Us for reconsideration of the decision.
F.I.11 PaymentTerms
The Sum Insured opted under the Plan shall be reduced by the amount
payable/paidundertheBenet(s)andthebalanceshallbeavailable
as the Sum Insured for the unexpired Policy Year.
If You/ Insured Person suffers a relapse within 45 days of the date of
discharge from the Hospital for which a claim has been made, then
such relapse shall be deemed to be part of the same claim and all the
limits for “Any One Illness” under this Policy shall be applied as if they
were under a single claim.
For Cashless Claims, the payment shall be made to the Network
Hospitalwhosedischargewouldbecompleteandnal.
For Reimbursement Claims, the payment will be made to you. In the
unfortunate event of Your death, We will pay the nominee (as named
in the Policy Schedule) and in case of no nominee to the Legal Heir who
holds a succession certicate or Indemnity Bond to that effect,
whichever is available and whose discharge shall be treated as full and
naldischargeofitsliabilityunderthePolicy.
ClaimprocessApplicabletothefollowingSections:
F.I.12 DomesticSecondOpinion
(a) Receive Request for Expert Opinion on Critical Illness
You can submit Your request for an expert opinion by calling Our call
centre or register request through email.
(b) Facilitating the Process
We will schedule an appointment or facilitate delivery of Medical
Records of the Insured Person to a Medical Practitioner. The expert
opinion is available only in the event of the Insured Person being
diagnosed with Covered Critical Illness.
F.I.13 HealthCheckupandTele-Consultation
(a) You or The Insured Person shall seek appointment by calling Our
call centre.
(b) We will facilitate Your appointment and We will guide You to the
nearest Network Provider for conducting the medical examination.
Reports of the Medical Tests can be collected directly from the
centre.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
F.I.14 WorldwideAccidentalEmergencyHospitalizationCover
a) In an unlikely event of You or the Insured Person requires
Emergency medical treatment outside India, You or Insured
Person, must notify Us either at Our call centre or in writing within
48 hours of such admission.
b) YoushallleaclaimforreimbursementinaccordancewithSection
G.I.5 of the Policy.
F.I.15. ApplicationofMultiplepoliciesclause
In case this clause is invoked in accordance to the terms and conditions
as provided under this Policy, the Claim will be adjudicated as under:
a) Retail policy of the Company & any other Policy from other
insurers:
i) Cashless hospitalization: In case the Insured avail Cashless
Facility for Hospitalization then Insured / Hospital will intimate us of
the admission through a pre-authorisation request with all details &
estimated amount for the Hospitalization. The policyholder having
multiple policies shall also have the right to prefer claims from other
policy / policies for the amounts disallowed under the earlier
chosen policy / policies, even if the sum insured is not exhausted.
Then the Insurer (s) shall settle the claim subject to the terms and
conditions of the other policy / policies so chosen. Post discharge,
the hospital will send all the original documents to one of the
insurer & certied copies of all documents to other insurers for
settlement along with authorisation letter. The Company will
evaluate the entire bill & arrive at the total payable amount &
deduct the amount already settled by the other insurers & settle the
difference payable amount to the hospital as per AL issued.
ii) Reimbursementclaim: In case the Insured gets admitted & pays
theentirebill&thenlesforreimbursementclaimthenhewillhave
to intimate us of the admission 48 hours before admission
for planned admissions & within 24 hours post hospitalization for
emergency hospitalization but in no case later than discharge from
the Hospital. Insured will need to submit details of the other
insurance policies to the Company. Post discharge insured will send
all the original documents along with bills & claim form to one of
theinsurer& certied copies of all documents & bills along with
dulylledclaimformtotheotherinsurers.Thepolicyholderhaving
multiple policies shall also have the right to prefer claims from other
policy / policies for the amounts disallowed under the earlier
chosen policy / policies, even if the sum insured is not exhausted.
Then the Insurer (s) shall settle the claim subject to the terms and
conditions of the other policy / policies so chosen.
b) Retailpolicy&grouppolicyfromtheCompany:
i). Cashlessprocess: In case the insured needs to utilize cashless
facility for hospitalization then the insured / hospital will intimate
the Company about the hospitalization through pre-authorisation
process. The policyholder having multiple policies shall also have
the right to prefer claims from other policy / policies for the amounts
disallowed under the earlier chosen policy / policies, even if the
sum insured is not exhausted. Then the Insurer (s) shall settle the
claim subject to the terms and conditions of the other policy /
policies so chosen.
Post discharge hospital will send as many separate claims as no.
of policies with the Company with attached authorisation letters &
original documents with the 1st claim & copy of documents with the
other claims for settlement to the Company. The Company will
settle all the claims as per policy terms & conditions & authorisation
letter issued.
ii). Reimbursement Claim process: In case the Insured gets
admitted&paystheentirebill&thenlesforreimbursementclaim
then he will have to intimate the Company of the admission 48
hours before admission for planned admissions & within 24 hours
post hospitalization for emergency hospitalization along with all the
policy numbers.
Post discharge insured will send all original documents & bills
alongwithdulylledclaimform.Thepolicyholderhavingmultiple
policies shall also have the right to prefer claims from other policy/
policies for the amounts disallowed under the earlier chosen policy/
policies, even if the sum insured is not exhausted. Then the Insurer
(s) shall settle the claim subject to the terms and conditions of the
other policy / policies so chosen.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
F.II.Annexure–I:
Ombudsman
ThecontactdetailsoftheInsuranceOmbudsmanofcesareasbelow:
NameoftheOfceofInsuranceOmbudsman State-wiseAreaofJurisdiction
AHMEDABAD
OfceoftheInsuranceOmbudsman,
Jeevan Prakash Building, 6
th
oor,
Tilak Marg, Relief Road,
Ahmedabad-380001.
Tel.:079-25501201/02/05/06
Email:- [email protected]
State of Gujarat and Union Territories of Dadra and Nagar Haveli and
Daman and Diu.
BENGALURU
OfceoftheInsuranceOmbudsman,
Jeevan Soudha Building, PID No. 57-27-N-19
Ground Floor, 19/19, 24
th
Main Road,
JP Nagar, 1
st
Phase,
Bengaluru-560078.
Tel.:080-26652048/26652049
Email:- [email protected]
State of Karnataka.
BHOPAL
OfceoftheInsuranceOmbudsman,
Janak Vihar Complex,
2
nd
Floor,6,MalviyaNagar,Opp.AirtelOfce,
Near New Market,
Bhopal-462003
Tel.:0755-2769201/202
Fax:0755-2769203
Email:- [email protected]
States of Madhya Pradesh and Chhattisgarh.
BHUBANESWAR
OfceoftheInsuranceOmbudsman,
62, Forest park,
Bhubaneshwar-751009.
Tel.:0674-2596461/2596455
Fax:0674-2596429
Email:- [email protected]
State of Orissa.
CHANDIGARH
OfceoftheInsuranceOmbudsman,
S.C.O.No.101,102&103,2
nd
Floor,
Batra Building, Sector 17 - D,
Chandigarh-160017.
Tel.:0172-2706196/6468
Fax:0172-2708274
Email:- [email protected]
States of Punjab, Haryana (excluding 4 districts viz Gurugram,
Faridabad, Sonepat and Bahadurgarh), Himachal Pradesh, Union
Territories of Jammu & Kashmir, Ladakh and Chandigarh.
CHENNAI
OfceoftheInsuranceOmbudsman,
Fatima Akhtar Court,
4
th
Floor, 453 (old 312), Anna Salai, Teynampet,
CHENNAI-600018.
Tel.:044-24333668/24335284
Fax:044-24333664
Email:- [email protected]
State of Tamil Nadu and Union Territories - Puducherry Town and
Karaikal (which are part of Union Territory of Puducherry).
DELHI
OfceoftheInsuranceOmbudsman,
2/2 A, Universal Insurance Building,
Asaf Ali Road,
NewDelhi-110002.
Tel.:011-23232481/23213504
Email:- [email protected]
Delhi, 4 Districts of Haryana viz. Gurugram, Faridabad, Sonepat and
Bahadurgarh.
GUWAHATI
OfceoftheInsuranceOmbudsman,
‘Jeevan Nivesh’, 5
th
Floor,
Nr. Panbazar over bridge, S.S. Road,
Guwahati-781001(ASSAM).
Tel.:0361-2132204/2132205
Email:- [email protected]
States of Assam, Meghalaya, Manipur, Mizoram, Arunachal Pradesh,
Nagaland and Tripura.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
HYDERABAD
OfceoftheInsuranceOmbudsman,
6-2-46, 1
st
oor,“MoinCourt”
Lane Opp. Saleem Function Palace,
A. C. Guards, Lakdi-Ka-Pool,
Hyderabad-500004.
Tel.:040-65504123/23312122
Fax:040-23376599
Email:- [email protected]
State of Andhra Pradesh, Telangana and Yanam - a part of Union
Territory of Puducherry.
JAIPUR
OfceoftheInsuranceOmbudsman,
Jeevan Nidhi - II Bldg., Gr. Floor,
Bhawani Singh Marg,
Jaipur-302005.
Tel.:0141-2740363
Email:- [email protected]
State of Rajasthan.
KOCHI
OfceoftheInsuranceOmbudsman,
2
nd
Floor,CC27/2603,PulinatBldg.,
Opp. Cochin Shipyard, M. G. Road,
Ernakulam-682015.
Tel.:0484-2358759/9338
Fax:0484-2359336
Email:- [email protected]
States of Kerala and Union Territory of (a) Lakshadweep (b) Mahe-a
part of Union Territory of Puducherry.
KOLKATA
OfceoftheInsuranceOmbudsman,HindustanBldg.Annexe,4,
C.R. Avenue, 4
th
Floor,KOLKATA-700072.
TEL.:033-22124340/22124339
Fax:033-22124341
Email:- [email protected]
States of West Bengal, Sikkim and Union Territories of Andaman &
Nicobar Islands.
LUCKNOW
OfceoftheInsuranceOmbudsman,
6
th
Floor, Jeevan Bhawan,
Phase-II, Nawal Kishore Road, Hazratganj,
Lucknow-226001.
Tel.:0522-2231330/1
Fax:0522-2231310
Email:- [email protected]
Districts of Uttar Pradesh
Lalitpur, Jhansi, Mahoba, Hamirpur, Banda, Chitrakoot, Allahabad,
Mirzapur, Sonbhadra, Fatehpur, Pratapgarh, Jaunpur,Varanasi,
Gazipur, Jalaun, Kanpur, Lucknow, Unnao, Sitapur, Lakhimpur,
Bahraich, Barabanki, Raebareli, Sravasti, Gonda, Faizabad,
Amethi, Kaushambi, Balrampur, Basti, Ambedkarnagar, Sultanpur,
Maharajganj, Santkabirnagar, Azamgarh, Kushinagar, Gorakhpur,
Deoria, Mau, Ghazipur, Chandauli, Ballia, Sidharthnagar.
MUMBAI
OfceoftheInsuranceOmbudsman,
3
rd
Floor, Jeevan Seva Annexe,
S. V. Road, Santacruz (W),
Mumbai-400054.
Tel.:022-26106552/6960
Fax:022-26106052
Email:- [email protected]
State of Goa and Mumbai Metropolitan Region excluding Areas of Navi
Mumbai and Thane.
NOIDA
OfceoftheInsuranceOmbudsman,
Bhagwan Sahai Palace
4
th
Floor, Main Road,
Naya Bans, Sector 15,
Distt: Gautam Buddh Nagar,
U.P-201301.
Tel.:0120-2514252/2514253
Email:- [email protected]
State of Uttaranchal and the districts of Uttar Pradesh:
Agra, Aligarh, Bagpat, Bareilly, Bijnor, Budaun, Bulandshehar, Etah,
Kanooj, Mainpuri, Mathura, Meerut, Moradabad, Muzaffarnagar,
Oraiyya, Pilibhit, Etawah, Farukkabad, Firozbad, Gautambodhanagar,
Ghaziabad, Hardoi, Shahjahanpur, Hapur, Shamli, Rampur, Kashganj,
Sambhal, Amroha, Hathras, Kanshiramnagar, Saharanpur.
PATNA
OfceoftheInsuranceOmbudsman,
1
st
Floor,Kalpana Arcade Building,
Bazar Samiti Road,
Bahadurpur,
Patna-800006.
Tel.:0612-2680952
Email:- [email protected]
States of Bihar and Jharkhand.
PUNE
OfceoftheInsuranceOmbudsman,
Jeevan Darshan Bldg., 3
rd
Floor,
C.T.S. No.s. 195 to 198,
N.C. Kelkar Road, Narayan Peth,
Pune-411030.
Tel.:020-41312555
Email:- [email protected]
State of Maharashtra, Areas of Navi Mumbai and Thane but excluding
Mumbai Metropolitan.

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
F.lllAnnexure–II:
Title
Description
PleaserefertothePlanandSumInsuredyouhaveoptedtounderstandtheavailablebenetsunderyourplaninbrief
YourCoverage
Details:
IdentifyyourPlan Active
BasicCover
This section lists
the Basic
benets
available on
your plan
Basic Cover
Identify your Opted Sum
Insured (in `)
`3 Lacs, `5 Lacs, `7.5 Lacs, `10Lacs,`12.5 Lacs, `15 Lacs
In-patient Hospitalization
(When you are
hospitalized) (`)
Room Rent :
ForSumInsured3lacs:1%ofSumInsured
For Sum Insured 5 lacs and above: Single Private A/C Room
For ICU - Up to Sum Insured
Sum Insured (in `) `3 Lacs `5 Lacs `7.5 and `10Lacs >`10Lacs
Treatment for each ailment /
procedure mentioned below:
1. Surgery for treatment of all types
of Hernia
2. Hysterectomy
3. Surgeries for benign Prostate
Hypertrophy
4. Surgical treatment of stones
of renal system
`50,000 `65,000 `80,000
NA
Treatment of Cataract (Per Eye)
`20,000 `30,000 `30,000
NA
Treatment of Total Knee
replacement (Per knee)
`80,000 `1,00,000 `1,20,000
NA
Treatment for breakage of bones
`2,00,000 `2,50,000 `3,00,000
NA
Wherever the above mentioned Sub-limits are applied, the Mandatory Co-payment shall not be
applicable.
Thisbenetshallalsoofferthebelowcoversuptothelimitsmentioned:
a.ListedModernandAdvancedTreatments:upto50%ofSumInsured
b. HIV/AIDS & STD: up to Sum Insured
c.MentalIllness:upto50%ofSumInsured
For below mentioned ICD Codes: Waiting Period of 24 months shall apply:
ICD 10 CODES DISEASES
F05 Delirium due to known physiological condition
F06 Other mental disorders due to known physiological condition
F07 Personality and behavioural disorders due to known physiological condition
F10 Alcohol related disorders
F20 Schizophrenia
F23 Brief psychotic disorders
F25 Schizoaffective disorders
F29 Unspeciedpsychosisnotduetoasubstanceorknownphysiologicalcondition
F31 Bipolar disorder
F32 Depressive episode
F39 Unspeciedmood[affective]disorder
F40 Phobic Anxiety disorders
F41 Other Anxiety disorders
F42 Obsessive-compulsive disorder
F44 Dissociative and conversion disorders
F45 Somatoform disorders
F48 Other nonpsychotic mental disorders
F60 Specicpersonalitydisorders
F84 Pervasive developmental disorders
F90 Attention-decithyperactivitydisorders
F99 Mentaldisorder,nototherwisespecied
Pre – hospitalization
MedicalExpensesCoveredupto30daysbeforethedateofhospitalization;
Covered upto the Sum Insured
Post – hospitalization
MedicalExpensesCoveredupto60dayspostdischargefromthehospital;
Covered upto the Sum Insured

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Day Care Treatment Covered up to the Sum Insured
Domiciliary Hospitalization
(Treatment at Home)
Coveredupto10%oftheSumInsured.
PreandPostHospitalizationExpenses:30dayseach
Road Ambulance
(Reimbursement of
Ambulance Expenses)
Covered up to the Sum Insured
Donor Expenses
(Hospitalization Expenses
of the donor providing the
organ)
Covered up to the Sum Insured
Restoration of Sum
Insured
(When opted Sum Insured
isinsufcientdueto
claims)
Multiple Restoration is available in a Policy Year for unrelated illnesses, in addition to the Sum
Insured
Applicable for below covers only
1. D.I.1 – In-patient Hospitalization
2. D.I.2 – Pre - hospitalization
3. D.I.3 – Post - hospitalization
4. D.I.4 – Day Care Treatment
5. D.I.6 – Road Ambulance
6. D.I.7 – Donor Expenses
7. D.I.9 – AYUSH Treatment
8. D.III.1 – Non-Medical Items
Restoration shall not get triggered for the 1
st
claim
The maximum liability under a single claim shall not be more than Base Sum Insured + Cumulative
Bonus + Restored Sum Insured
AYUSH Treatment (In-
patient Hospitalization)
Covered up to the Sum Insured
ConvalescenceBenet
(ForHospitalization>=10
days)
Applicable for Sum Insured of `5lacsandabove:Lumpsumbenetamountingto`30,000per
hospitalizationuponcompletionofatleast10consecutivedaysof
hospitalization.
Daily Cash for Shared
Accommodation (in `)
DailyCashbenetforoccupyingsharedaccommodationwhilehospitalizedshallbecoveredas
below:-
a. For Sum Insured from `5 lacs up to `10Lacs:`800perdayuptomaximumof`5600
b. For Sum Insured above `10Lacs:`1,000perdayuptomaximumof`7000
Payable for each continuous and completed 24 Hours of Hospitalization during the Policy Year.
Thisbenetgetstriggeredpost48hoursofIn-patienthospitalizationandshallbepayablefrom1
st
day
onwards.
ValueAdded
Covers
This section lists
the additional
value added
benetsthatare
available along
with your plan
Domestic Second Opinion Available for 36 listed Critical Illness/es
Tele consultation Unlimited Tele-consultation in a Policy Year
Cumulative Bonus
Bonusof10%perclaimfreeyear,subjecttoamaximum:upto100%ofsuminsured.
Incaseofaclaim,theaccumulatedCumulativeBonusshallgetreduced@10%ofSumInsured
Wellness Program
(For Lives suffering
from one or more
of the following
conditions: Asthma,
Diabetes, Hypertension,
Dyslipidaemia, Obesity)
Rewards can be earned by adhering to Condition Management Program and
improving the Health Parameters. These earned Reward Points can be used against payable
Renewal premium (excluding optional covers, Rider and taxes) as discount from 1
st
Renewal of the
Policy.
RewardAccrual-Maxupto15%oftheexpiringbasePremium(excludingoptionalcovers,Riderand
taxes), applicable for the respective insured.
Reward Redemption:
The earned reward points could be redeemed as discount to pay a portion of the renewal premium
(excluding optional covers, Rider and taxes).
The earned rewards shall lapse, in case the same is not used at the time of
subsequent renewal (renewal falling due immediately after the accrual).
Discount from Network
Provider
Discount on Pharmacy, Diagnostics and Health Supplement offered by the Network Providers of
ManipalCigna Health Insurance Company Limited
PremiumWaiverBenet
Waives off one year Policy Premium (including premium for optional covers, rider and taxes) upon
occurrence of any of the listed contingencies (Accidental death/ listed Critical Illnesses) to the
Policyholder who is also an Insured Person in the Policy

ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
Optional
Covers
Non-Medical Items
Non-Medical items covered up to Sum Insured opted in case of In-patient
Hospitalization and/or Day Care Treatment a policy year
Waiver of Mandatory Co-payment WaiverofMandatoryCo-paymentof10%perclaimsubjecttounderwriting
Worldwide Accidental Emergency
Hospitalization Cover
(Applicable to Indian Residents only)
Covered up to Sum Insured opted for Emergency In-patient Hospitalization outside
India.ThisbenetisavailableonceinaPolicyYearforeachInsuredPerson.
Health Check Up (in `)
Available once every third policy year each policy year, to all Adult insured persons
who have completed 18 years of Age, subject to a maximum of upto `2500peradult
member in lieu of ‘Wellness Program’.
Thisbenetshallbeofferedoncashlessbasisonly.However,theeligibleinsured
may avail any health check from the MCHI Network of Health Check Up Center upto
thelimitspecied
WaiverofDiseaseSpecicSublimit
DiseaseSpecicSublimitwhichisapplicableforlistedailments/proceduresas
speciedundersectionD.I.1In-patienthospitalizationshallbewaivedsubjectto
underwriting.
ManipalCignaProHealthPrime|ActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
F.lV.Annexure-III
ListI-ItemsforwhichCoverageisnotavailableinthePolicy
Sl.
No.
Item
1. BABY FOOD
2. BABY UTILITIES CHARGES
3. BEAUTY SERVICES
4. BELTS / BRACES
5. BUDS
6. COLD PACK / HOT PACK
7. CARRY BAGS
8. EMAIL I INTERNET CHARGES
9. FOOD CHARGES (OTHER THAN PATIENT’s DIET PROVIDED
BY HOSPITAL)
10. LEGGINGS
11. LAUNDRY CHARGES
12. MINERAL WATER
13. SANITARY PAD
14. TELEPHONE CHARGES
15. GUEST SERVICES
16. CREPE BANDAGE
17. DIAPER OF ANY TYPE
18. EYELET COLLAR
19. SLINGS
20. BLOOD GROUPING AND CROSS MATCHING OF DONORS
SAMPLES
21. SERVICE CHARGES WHERE NURSING CHARGE ALSO
CHARGED
22. TELEVISION CHARGES
23. SURCHARGES
24. ATTENDANT CHARGES
25. EXTRA DIET OF PATIENT (OTHER THAN THAT WHICH
FORMS PART OF BED CHARGE)
26. BIRTH CERTIFICATE
27. CERTIFICATE CHARGES
28. COURIER CHARGES
29. CONVEYANCE CHARGES
30. MEDICAL CERTIFICATE
31. MEDICAL RECORDS
32. PHOTOCOPIES CHARGES
33. MORTUARY CHARGES
34. WALKING AIDS CHARGES
35. OXYGEN CYLINDER (FOR USAGE OUTSIDE THE
HOSPITAL)
36. SPACER
37. SPIROMETRE
38. NEBULIZER KIT
39. STEAM INHALER
40. ARMSLING
41. THERMOMETER
42. CERVICAL COLLAR
43. SPLINT
44. DIABETIC FOOT WEAR
45. KNEE BRACES (LONG / SHORT / HINGED)
46. KNEE IMMOBILIZER / SHOULDER IMMOBILIZER
47. LUMBO SACRAL BELT
48. NIMBUS BED OR WATER OR AIR BED CHARGES
49. AMBULANCE COLLAR
50. AMBULANCE EQUIPMENT
51. ABDOMINAL BINDER
52. PRIVATE NURSES CHARGES - SPECIAL NURSING
CHARGES
53. SUGAR FREE Tablets
54. CREAMS POWDERS LOTIONS (Toiletries are not payable,
only prescribed medical pharmaceuticals payable)
55. ECG ELECTRODES
56. GLOVES
57. NEBULISATION KIT
58. ANYKITWITHNODETAILSMENTIONED[DELIVERYKIT,
ORTHOKIT,RECOVERYKIT,ETC]
59. KIDNEY TRAY
60. MASK
61. OUNCE GLASS
62. OXYGEN MASK
63. PELVIC TRACTION BELT
64. PAN CAN
65. TROLLY COVER
66. UROMETER, URINE JUG
67. AMBULANCE
68. VASOFIX SAFETY
ListII-ItemsthataretobesubsumedintoRoomCharges
SI.
No.
Item
1. BABY CHARGES (UNLESS SPECIFIED / INDICATED)
2. HAND WASH
3. SHOE COVER
4. CAPS
5. CRADLE CHARGES
6. COMB
7. EAU-DE-COLOGNE I ROOM FRESHNERS
8. FOOT COVER
9. GOWN
10. SLIPPERS
11. TISSUE PAPER
12. TOOTH PASTE
13. TOOTH BRUSH
14. BED PAN
15. FACE MASK
16. FLEXI MASK
17. HAND HOLDER
18. SPUTUM CUP
19. DISINFECTANT LOTIONS
20. LUXURY TAX
21. HVAC
22. HOUSE KEEPING CHARGES
23. AIR CONDITIONER CHARGES
24. IM IV INJECTION CHARGES

1. CLEAN SHEET
2. BLANKET / WARMER BLANKET
3. ADMISSION KIT
4. DIABETIC CHART CHARGES
5. DOCUMENTATION CHARGES I ADMINISTRATIVE
EXPENSES
6. DISCHARGE PROCEDURE CHARGES
7. DAILY CHART CHARGES
8. ENTRANCE PASS I VISITORS PASS CHARGES
9. EXPENSES RELATED TO PRESCRIPTION ON DISCHARGE
10. FILE OPENING CHARGES
11. INCIDENTAL EXPENSES I MISC. CHARGES (NOT
EXPLAINED)
12. PATIENT IDENTIFICATION BAND I NAME TAG
13. PULSEOXYMETER CHARGES
ListIII-ItemsthataretobesubsumedintoProcedureCharges
1. HAIR REMOVAL CREAM
2. DISPOSABLES RAZORS CHARGES (for site preparations)
3. EYE PAD
4. EYE SHEILD
5. CAMERA COVER
6. DVD, CD CHARGES
7. GAUSE SOFT
8. GAUZE
9. WARD AND THEATRE BOOKING CHARGES
10. ARTHROSCOPY AND ENDOSCOPY INSTRUMENTS
11. MICROSCOPE COVER
12. SURGICAL BLADES, HARMONICSCALPEL, SHAVER
13. SURGICAL DRILL
14. EYE KIT
15. EYE DRAPE
16. X-RAY FILM
17. BOYLES APPARATUS CHARGES
18. COTTON
19. COTTON BANDAGE
20. SURGICAL TAPE
21. APRON
22. TORNIQUET
23. ORTHOBUNDLE, GYNAEC BUNDLE
ListIV-Itemsthataretobesubsumedintocostsoftreatment
SI.
No.
Item
1. ADMISSION / REGISTRATION CHARGES
2. HOSPITALIZATION FOR EVALUATION / DIAGNOSTIC
PURPOSE
3. URINE CONTAINER
4. BLOOD RESERVATION CHARGES AND ANTE NATAL
BOOKING CHARGES
5. BIPAP MACHINE
6. CPAP / CAPO EQUIPMENTS
7. INFUSION PUMP - COST
8. HYDROGEN PEROXIDE \SPIRIT \ DISINFECTANTS ETC
9. NUTRITION PLANNING CHARGES - DIETICIAN
CHARGES - DIET CHARGES
10. HIV KIT
11. ANTISEPTIC MOUTHWASH
12. LOZENGES
13. MOUTH PAINT
14. VACCINATION CHARGES
15. ALCOHOL SWABES
16. SCRUB SOLUTIONISTERILLIUM
17. GLUCOMETER & STRIPS
18. URINE BAG
ManipalCignaProHealthPrime|ProtectPlan,AdvantagePlanandActivePlan|Terms&Conditions|UIN:MCIHLIP22224V012122|April2022
1800-102-4462
For any assistance contact:
www.manipalcigna.co
m
Corporate Oce: ManipalCigna Health Insurance Company Limited (Formerly known as CignaTTK Health Insurance Company Limited)
401/402, Raheja Titanium, Western Express Highway, Goregaon East, Mumbai - 400063. IRDAI Registration No. 151
