
National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 1 of
42
Prepared By: Road Safety & Public Health Research Team, Department of
Emergency Medicine, Faculty of Medicine, University of British Columbia
Alberta Drug Driving Study Progress Report 2024
Edmonton
Calgary
Alberta
National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 2 of
42
Acknowledgment
This study has been made possible through funding from:
Alberta Ministry of Justice and Solicitor (2022-2024)
Alberta Ministry of Transportation and Economic Corridors (2018-2023)
Public Safety Canada (2023-2025)
Transport Canada (2020-2023)
Health Canada (2019-2022)
Canadian Institutes of Health Research (2011-2024)
Canadian Centre on Substance Use and Addiction (2019-2022)
The views expressed herein do not necessarily represent the views of the funders.
Suggested Citation: Brubacher JR, Chan H, Erdelyi S, Simmons S, Rowe B, Wishart I and the National Drug
Driving Research Group. The 2024 Alberta Drug Driving Study Report. Vancouver, BC. Department of Emergency
Medicine, University of British Columbia.
Canadian Drug Driving Study Research Group:
Dr. Paul Atkinson
Dalhousie University (Dalhousie Medicine New Brunswick)
Dr. Floyd Besserer
University of Northern British Columbia
Dr. Jeff Brubacher
University of British Columbia
Dr. Herbert Chan
University of British Columbia
Dr. David Clarke
Dalhousie University
Dr. Gregory Clark
McGill University
Dr. Raoul Daoust
University of Montreal
Dr. Phil Davis
University of Saskatchewan
Dr. Jeff Eppler
University of British Columbia
Dr. Marcel Emond
Université Laval
Dr. Chrystal Horwood
Memorial University
Dr. Jacques Lee
University of Toronto
Dr. Andrew MacPherson
University of British Columbia
Dr. Kirk Magee
Dalhousie University
Dr. Éric Mercier
Université Laval
Dr. Robert Ohle
Health Sciences North Research Institute
Dr. Michael Parsons
Memorial University
Dr. Jagadish Rao
University of Saskatchewan
Dr. Brian Rowe
University of Alberta
Dr. John Taylor
University of British Columbia
Dr. Christian Vaillancourt
University of Ottawa
Dr. Ian Wishart
University of Calgary

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 3 of
42
Contributions of medical lab personnel, research assistants and coordinators at each hospital site have made this
project possible and successful across Canada.
Current Hospital Site Research Coordinators:
Hospital
City, Province
Research Coordinators
Vancouver General Hospital
(Study Coordination Site)
Vancouver, BC
Sneha Yadav, Lulu Pei
Victoria General Hospital
Victoria, BC
Ashlee de Medeiros
Royal Columbian Hospital
New Westminster, BC
Amanda Swirhun
Kelowna General Hospital
Kelowna, BC
Mackenzie Cheyne
University Hospital of Northern BC
Prince George, BC
Celia Belamour
Foothills Hospital
Calgary, AB
Christina Cherian
University Hospital
Edmonton, AB
Stephanie Couperthwaite
Royal University Hospital
Saskatoon, SK
Taylor Weir, Meagan Larson
Regina General Hospital
Regina, SK
Andrea Stringer
Sunnybrook Health Sciences Ctr
Toronto, ON
Clotilde Ngwa
Ottawa Hospital Civic Campus
Ottawa, ON
Manya Charette
Health Science North
Sudbury, ON
Kayla Labranche
Hôpital du Sacré-Cœur
Montreal, QC
Chantal Lanthier
Hôpital de l'Enfant-Jésus
Quebec, QC
Alexandra Nadeau
Hôpital Royal Victoria
Montreal, QC
David Iannuzzi
Saint John Regional Hospital
Saint John, NB
Pamela McDougall
QEII Health Sciences Center
Halifax, NS
Nelofar Kureshi
Health Sciences Centre
Saint John’s, NL
Amanda Pearce
Road Safety and Public Health Research - Toxicology Lab
Consultant
Mahmood Khan
Technician
Aman Mohammed
We acknowledge that the Study Coordination Research Office located at the Vancouver Costal Heath Research
Institute lies on the unceded traditional homelands of the Musqueam, Squamish and Tsleil-Waututh Nations
.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 4 of
42
Table of Contents
Terminology and Definitions 5
Drug driving and Drug impaired Driving 5
Psychomotor Skills 5
Cannabinoids 5
Central Nervous System Depressants 6
Opioids 7
Central Nervous System Stimulants 7
Polysubstance Use 7
Liquid chromatography/tandem mass spectrometry (LC-MS/MS) 7
Gas Chromatography-Flame Ionization Detection 7
Phlebotomists 7
Background 8
Methods 10
Inclusion and Exclusion Criteria 10
Chart Review 10
Blood Handling 10
Toxicology Analysis 10
Results 12
Discussion 13
Strengths 14
Limitations 14
Summary 15
Appendix A: Tables 16
Appendix B: Figures 21
References 39

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 5 of
42
Terminology and Definitions
Drug driving and Drug impaired Driving
“Drug-impaired driving” means that the driver is impaired by drugs, where “impaired” means that those
drugs interfere with safe driving ability. When drivers have positive tests for drugs, we often do not know if
they were actually engaging in “drug-impaired driving.” This is because the presence of drugs in body fluids
indicates prior drug use but not necessarily impairment. When drugs are detected within a driver’s body
fluids, but we do not know whether that driver was actually impaired at the time of testing, we use the term
“drug driving.”
Psychomotor Skills
Safe driving involves the application of a number of psychomotor skills. These refer to the skills we use to
perceive sensory information, interpret its meaning, and respond through physical actions.” Examples of
psychomotor skills applied to driving include reaction time, tracking ability (e.g. ability to drive a car in a
straight line without weaving), coordination, and tasks that require attention
Cannabinoids
Cannabis and Marijuana
The term “Cannabis” refers to all products derived from the plants Cannabis sativa and Cannabis indica
that contain various amount of THC (delta-9-tetrahydrocannabinol) whereas Marijuana refers specifically to
plant products (dried flowers, leaves, stems and seeds). Throughout this report, we use the term “Cannabis”.
Cannabis contains over 60 active compounds known as cannabinoids such as THC, CBD, CBN. When
absorbed into the blood, cannabinoids exert their effects by binding to receptors in the brain and throughout
the body.
THC (delta-9-tetrahydrocannabinol)
THC is the main psychoactive compound found in cannabis and is responsible for most of its impairing effects.
THC Levels
The term “THC level” refers to the amount of THC within a person’s body after smoking, vaporizing or eating
a cannabis product. There are different ways to measure THC levels. The best way to understand if
someone has used cannabis recently is to look at the THC level in their blood. However, interpreting the
precise time that someone took cannabis – and importantly, whether or not they are still experiencing its
effects – is complicated. Immediately after smoking a “joint”, whole blood THC levels typically peak at >100
ng/mL within 15 minutes and then drop rapidly so that, in occasional users, THC is usually <2ng/mL (i.e.,
the legislated limit associated with a summary offence in Canada) within 4 hours after a single acute
exposure.
1
However, in habitual cannabis users, THC accumulates in body fat and is then slowly released
back into the blood. As a result, habitual users can have THC levels in the range of 1 -3 ng/mL for days or
even weeks after last use.
2
In most cases, however, THC > 5 ng/mL (i.e., the legislated limit associated with
a hybrid offence in Canada) indicates recent use. After smoking a marijuana joint, the psychotropic
(impairing) effects typically peak at 20–30 minutes and resolve by 4 hours. Ingesting cannabis delays the
onset and extends the duration of effect.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 6 of
42
COOH-THC (11-nor-9-carboxy-delta-9-tetrahydrocannabinol)
The main metabolite (breakdown product) of THC. COOH-THC does not cause impairment and persists in
blood and urine long after impairment has resolved. Thus COOH-THC provides evidence of previous
cannabis exposure but does not necessarily indicate impairment or recent use.
Other commonly detected Cannabinols
11-Hydroxy-delta-9-tetrahydrocannabinol, commonly known as 11-hydroxy-THC, is the major active
metabolite of THC. It has similar psychotropic effects as THC although some users claim that it is more
potent. 11-hydroxy-THC is formed in the liver after cannabis is consumed through inhalation or orally;
however, the level of 11-hydroxy-THC is generally higher when cannabis is consumed orally.
Cannabidiol (CBD) is the second most prevalent bioactive compound found in the Cannabis sativa plant.
CBD itself does not produce euphoric effects (“high”). CBD is typically used in medical cannabis
formulations for controlling refractory seizures, managing symptoms such as anxiety, depression and
arthritis, and alleviating pain from cancer or nerve damage. It is also used to treat opioid addiction in some
occasions.
Cannabinol (CBN) is less commonly used in medical cannabis formulations but has gained popularity in
recent years. It is used primarily for sleep and pain management. Similar to CBD, it does not produce
psychotropic effects.
Central Nervous System Depressants
Many prescription medications cause sedation either as a desired therapeutic effect or as an unwanted side
effect. In the Drug Evaluation and Classification System, these drugs would be classified as CNS (central
nervous system) depressants. Common sedating medications include:
Benzodiazepines
These are mild sedatives most commonly prescribed as “sleeping pills” or to treat anxiety.
Anticonvulsants
Anticonvulsants, more commonly known as antiepileptic drugs, may cause sedation, dizziness, and
cognitive changes.
Antihistamines
Antihistamines cause sedation as an unwanted side effect. Over the counter antihistamines are used to
treat allergies (e.g. diphenhydramine - “Benadryl”), or motion sickness (e.g. dimenhydrinate - “Gravol”).
Antidepressants
Antidepressants, especially the older antidepressants, have sedation as a side effect.
Antipsychotics
Sedation is a common side effect of antipsychotic drugs.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 7 of
42
Muscle relaxants
Muscle relaxants may have sedative effects such as drowsiness. People are generally advised not to drive
or operate heavy machines while under the effects of muscle relaxants.
Non-benzodiazepine hypnotics
Also known as “Z-drugs”. These drugs are sedatives that act like benzodiazepines and are prescribed
mostly as sleep aids. In Canada the most common non-benzodiazepine hypnotic is zopiclone.
Opioids
Opioids are narcotic analgesics (pain killers) that can cause marked sedation or even coma along with
respiratory depression. Opioids include prescription medications such as codeine, hydromorphone,
oxycodone, and morphine. The street drug heroin is also an opioid.
Central Nervous System Stimulants
CNS stimulants are drugs, such as cocaine or amphetamines, that cause CNS stimulation. Intoxication with
these drugs is characterized by restlessness or agitation, pressured speech, anxiety, paranoia and
aggressive behaviour. Judgement may be impaired. Blood pressure and pulse are increased and pupils are
dilated.
Polysubstance Use
People who use drugs often take more than one substance at the same time. This is referred to as
polysubstance use. Taking several drugs in combination can lead to worse impairment than would be seen
from either substance taken alone.
Liquid chromatography/tandem mass spectrometry (LC-MS/MS)
An advanced laboratory technology that is used to detect and/or quantify a wide range of drugs using
standards of known substances and concentrations.
Gas Chromatography-Flame Ionization Detection
A standard laboratory technique used for measuring blood alcohol levels.
Phlebotomists
Specially trained technicians who obtain blood samples from patients.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 8 of
42
Background
The epidemiology and risk of crashing in drinking drivers is well understood as a result of intense research
conducted over the past 50 years.
3-6
This knowledge has facilitated the development of effective measures
targeting alcohol-impaired driving. Alcohol-impaired driving and related fatalities are declining as a result of
visibly enforced laws, administrative licensing sanctions, and social marketing campaigns.
7-11
Drug driving
is also viewed as a major threat to road safety,
12
and the prevalence of drug driving may be increasing.
13
In
fact, there is evidence that drug driving has become as common as driving after drinking alcohol in
Canada.
14-18
With cannabis legalization, there is concern that the prevalence of drug driving, especially
driving after using cannabis, will increase. Cannabis legalization could also result in more drivers combining
cannabis with alcohol or other drugs, resulting in additive impairment.
19-21
The effect of alcohol on driving and road safety is well-studied and understood. Experimental and
epidemiological studies have made it possible to predict how driving will be affected at different breath and
blood alcohol concentrations. For example, the risk of crashing approximately doubled at a BAC between
0.05% and 0.08%.
6
However, drugs tend to have more complicated pharmacokinetics and
pharmacodynamics than alcohol. Unlike alcohol, it is often not possible to predict how driving will be affected
at different drug blood alcohol concentrations. This issue makes it difficult to differentiate drug-driving (i.e.,
positive for drugs but absent of impairment) from drug-impaired driving (i.e., positive for drugs and active
impairment) in epidemiological studies, and it makes it difficult to extrapolate the results of experimental
studies focused on drug-impaired driving to real world safety. For example, we know that many drugs impair
the psychomotor skills and/or judgment required for safe driving. Cannabis intoxication causes attention
deficits, slows reaction time and impairs tasks such as tracking ability (e.g., staying within a lane) or
monitoring the speedometer.
19, 22-26
Several expert panels compared experimental studies of impairment
from THC with that from alcohol, in both males and females, and concluded that a blood alcohol
concentration (BAC) of 0.05% causes a similar degree of psychomotor impairment as THC levels in whole
blood of 2-5ng/mL.
27-29
However, habitual cannabis users may develop tolerance to some of the impairing
effects of cannabis.
30-32
Differences in tolerance between users calls into question the ability to reliably infer
impairment for any given user based on a specific THC level. In particular, a conservative THC limit imposed
on all drivers may be inequitable for habitual users, who may be more likely to have cannabis in their system
at any given time, yet less likely to experience impairment at that THC level. Additionally, although
cannabis-impaired driving is very topical, it is important to realize that many other drugs also cause
psychomotor skill impairment. Stimulants, such as cocaine and amphetamines, impair judgment, impair
inhibitory control (ability to “tune out” and not react to irrelevant stimuli), and alter mood.
33-40
Sedating
medications, such as benzodiazepines, antihistamines, antidepressants, Z-drugs (non-benzodiazepine
sedatives such as zopiclone), and opioids, cause drowsiness, slow reaction time, impair cognitive function
and impair tracking ability.
41-51
For these reasons, many drugs are suspected to increase the risk of crashing.
Several recent meta-analyses all concluded that cannabis increases the risk of crashing, albeit to a lesser
extent than alcohol.
52-55
There is epidemiological evidence that other drugs (amphetamines, cocaine,
benzodiazepines, antihistamines, antidepressants and opioids) also increase crash risk. In fact, the crash
risk with many of these drugs, although lower than that with alcohol, appears to be as high as or even higher
than the risk associated with cannabis.
55-58
The prevalence of drug driving in Canada is poorly studied. Previous research on the prevalence of drug
use in Canadian drivers is based on roadside surveys, coroner’s reports, police crash reports, or self-

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 9 of
42
reported surveys.
14, 16, 59-61
These methods have significant limitations. In roadside surveys, police pull over
drivers and direct them to a safe parking spot. Researchers then ask the drivers about drug and alcohol use
and obtain samples for drug testing. Roadside surveys are limited by high refusal rates which could result
in selection bias if drivers who used drugs are more likely to refuse than other drivers. For practical reasons,
roadside surveys use saliva rather than blood. However, blood THC levels are considered more informative
than saliva THC levels because THC crosses freely from the blood into the brain,
62
whereas saliva THC
represents deposition of THC in the mouth during smoking and is poorly correlated with blood THC
concentrations.
63
For logistic reasons, roadside surveys typically sample a large number of drivers over a
few days during the summer (when weather is good) making these surveys poorly suited for long term
monitoring of drug driving. Another limitation is that, because of high cost and logistic challenges, roadside
surveys are seldom performed. Coroner’s data provide another estimate of the prevalence of drug use in
drivers. In 2016, 82.7% of fatally injured Canadian drivers were tested for drugs and 46.7% were positive
for an impairing drug other than alcohol, including 23.1% who tested positive for cannabis. Females were
less likely than males to be positive for alcohol but almost as likely to test positive for drugs (41.7% in
females versus 48.2% in males).
64
Coroner’s data are useful but can be susceptible to selection bias if drug
testing is based on suspicion of drug use and not performed routinely on all drivers. In Canada, the
percentage of fatally injured drivers tested for drugs (2008) varies by province, ranging from 10% to 100%.
The toxicology testing protocols used by coroners differ from province to province - with different protocols
detecting different drugs. Coroner’s data often fail to between distinguish between drug exposure that last
occurred within the hours, days or weeks prior to the crash because some coroners measure inactive drug
metabolites (which can persist in the body for long periods) rather than active drug. If fatally injured drivers
survive the crash for a period of time, drug levels will decline with metabolism, making toxicology testing
unreliable. Interpreting drug levels from coroner’s data is further complicated by postmortem redistribution.
For some drugs (such as cannabis), postmortem redistribution of drug concentrations within the body can
lead to significant differences between the measurable drug level immediately prior to death (which is more
representative of the actual drug level at the time of the crash) and the drug level measurable some time
later after death.
65-69
As driving while impaired by drugs is illegal, police crash reports allow police to record
their suspicion that a driver is impaired by drugs. However, these reports provide unreliable estimates of
cannabis/other drug use as police only identify a small fraction of drivers who use cannabis or other drugs.
70
Self-report surveys ask questions about driving after using cannabis or other drugs.
71
Surveys are subject
to selection, recall and reporting biases. In addition, self-report surveys typically lack precision because
they ask about drug use before driving in a given time period (e.g., previous month) instead of before a
specific driving episode.
The Alberta drug driving study is part of the Canadian national drug driving project that studies drug use in
injured drivers who present to hospital and have bloodwork obtained within six hours of a motor vehicle
collision. To address the limitations of prior research, we study a relevant population (injured drivers) and
measure a wide range of impairing drugs in blood within six hours of a crash. Hence, this research has
several advantages over other methods of studying drug driving. We aim to provide relevant data that policy
makers and injury prevention groups can use to inform policy and programs designed to prevent people
from driving after using drugs.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 10 of
42
Methods
Inclusion and Exclusion Criteria
We include all moderately or severely injured drivers of motorized vehicles (e.g. cars, motorcycles, trucks)
who visited the emergency department (ED) of a participating hospital and had blood samples obtained
within 6 hours of the crash. Injury severity is defined pragmatically as the need to obtain blood for clinical
purposes (moderate injury), or need for overnight hospital admission (severe injury). Potentially eligible
drivers are identified by daily review of ED visit logs and eligibility is confirmed through chart review. We
exclude drivers with minor injuries who do not require blood testing for clinical purposes, drivers under 16
years of age, cases in which blood was first obtained more than 6 hours after the crash, cases in which no
excess blood remains after clinical use, and cases in which the quantity of excess blood was insufficient for
toxicology testing of all substances.
Chart Review
ED records of eligible drivers are reviewed, and relevant data is abstracted and entered in REDCap, a
secure web application for building and managing online surveys and databases. ED records include
ambulance records (filled by paramedics), emergency physician notes, nursing notes, laboratory results
including blood alcohol concentration (BAC), and consultant notes (if applicable). The abstracted data
includes age, sex, first three digits of postal code, crash time and date, crash type (single vs multiple),
vehicle type, blood draw time, prescription medications used in last 30 days, medical history, documentation
of alcohol or drug use, disposition and medications given as part of clinical care prior to blood draw (we
exclude “post-crash” medications when reporting toxicology results).
Blood Handling
Blood availability is determined by research assistants through review of medical records (to identify drivers
who had blood samples drawn) followed by a visit to the hospital laboratory to see if excess blood remains.
Excess blood is relabeled with study ID number replacing the clinical label and frozen at -40º C for future
analysis. Freezing is important as significant losses of THC/other drugs will occur by two months if blood is
stored at room temperature. As blood concentrations of certain drugs, such as cocaine and THC, drop
rapidly after use, it is important that time from crash until blood draw is carefully recorded. The time of crash
is determined through chart reviews (usually recorded on the ambulance record), and phlebotomists record
the time of blood draw. Blood samples are stored in a specimen freezer at each site before shipment on dry
ice by overnight courier to the central laboratory in Vancouver where samples are stored at -40º C until
ready for analysis.
Toxicology Analysis
In participating hospitals, blood from injured drivers is usually tested for alcohol as part of routine trauma
care. When clinical alcohol levels were not available, alcohol was measured at the BC Provincial Toxicology
Centre using Gas Chromatography-Flame Ionization Detection with a detection limit of 0.01%. In addition,
broad spectrum drug screens were performed on each patient’s blood using liquid chromatography/tandem
mass spectrometry (LC-MS/MS). Beginning in April 2023, alcohol and toxicology analyses are performed
by our own Road Safety & Public Health Research Toxicology Lab. The extraction process recovers both
acidic and basic drugs and is able to detect illicit drugs and their metabolites (cannabinoids, cocaine,
amphetamines including their major analogues, and opioids) as well as psychotropic pharmaceuticals
(including antihistamines, benzodiazepines, other hypnotics, and sedating antidepressants). The method

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 11 of
42
has detection limits of 0.2 ng/mL for THC and 1 ng/mL for most other substances. When samples are
positive for cannabinoids, we quantify both the active ingredient (THC) and the metabolite (COOH-THC).
For other drugs, the LC-MS/MS screen will provide a quantitative measure of drug concentration using ISO-
certified reference calibrators. Over 95% of excess blood samples in this study consisted of whole blood.
When plasma is available but whole blood was not, we adjust plasma toxicology results to equivalent whole
blood results according to previously published studies.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 12 of
42
Results
The study received research ethics approval and hospital operational approval from 2 trauma centres in
Alberta, including Foothills Hospital, Calgary and University Hospital, Edmonton. Data collection began in
May, 2018 in Calgary and June 2018 in Edmonton. As of December 31, 2023, approximately 3170 blood
samples of eligible cases were collected in Alberta (1700 from Calgary and 1470 from Edmonton) since
2018. The most common reasons for exclusion from the study were either no blood work required or
exceeding the 6-hour time frame between crash and blood draw. For this report, chart review data from
2113 eligible cases from Alberta with ED admission date up to November 2022 were completed and their
blood samples were analyzed. Results of these 2113 cases with complete data are presented in this report.
Overall, one in seven (13.9%) drivers in this sample tested positive for THC, including one in seventeen
(5.9%) with THC ≥ 2 ng/mL and one in thirty-four (2.9%) with THC ≥ 5 ng/mL). We also found that one in
six (15.6%) drivers tested positive for alcohol, including one in eight (12.9%) with BAC ≥ 0.08%. Opiates
were detected in one in seven (14.3%) drivers, recreational drugs (cocaine, amphetamines) in one in eight
(12.9%), and sedating medications (including the common over the counter antihistamine) in one in three
(29.3%) of injured drivers.
These results, broken down by age, sex and crash characteristics are shown in Tables 1 and 2 in Appendix
A and in Figures 1 to 15 in Appendix B. For comparison purposes, Table 3 in Appendix A summarizes
results (since January 2018) from all participating hospitals in British Columbia, Alberta, Saskatchewan,
Ontario, Quebec and the Atlantic provinces. Results between provinces cannot be directly compared
without adjusting for age, sex, injury severity and type of crash (singe versus multi-vehicle). Within these
limitations, it appears that injured drivers from Alberta, compared to all other provinces combined, are less
likely to have used cannabis (13.9% VS. 16.6%) and about as likely to have been drinking (15.6% VS. 16%)
and to have a blood alcohol level exceeding the legal limit of 0.08% (12.9% VS. 12.2%). They are slightly
more likely to have used opiates (14.3% VS. 10.4%), recreational drugs (12.9% VS. 12.1%), and sedating
medications (29.3% VS. 26.9%).
Table 4 in Appendix A and Figures 16 and 17 in Appendix B show polysubstance use, the percentage of
drivers who used various combinations of alcohol and cannabis (Figure 16) or other drug combinations
(Figure 17). In Alberta, 4.2% drivers/motorcyclists used cannabis and alcohol together which is about the
same as the national prevalence of 4.5%. The prevalence of drivers who used at least two different
categories of substances at the same time was one in four in Alberta (22.4%), which is also about the same
as the national average (21%).

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 13 of
42
Discussion
In this sample of 2113 injured drivers treated in two Alberta trauma centre(s), one in two (56.7%) drivers
tested positive for at least one impairing substance. In order of prevalence, these included sedating drugs
(29.3%), alcohol (15.6%), opiates (14.3%), cannabis (13.9%) and other recreational drugs (12.9%). In the
following section, we discuss the prevalence of cannabis, alcohol, and the three other classes of substances
(i.e., recreational drugs, sedating drugs and opiates) in turn.
Cannabis. The current state of knowledge indicates that the risk of crashing after using cannabis remains
poorly defined but is lower than that for alcohol.
24, 72
Several recent meta-analyses concluded that cannabis
increases crash risk, with estimated Odds Ratios (ORs) ranging from 1.36 to 2.66
52, 54
. A recent Canadian
study suggests that drivers with THC levels < 5 ng/mL do not have an increased risk of crashing
72
. However,
it is worth monitoring the prevalence of drivers with THC ≥ 5 ng/mL over time to analyze whether cannabis
impaired driving may be an emerging problem in Alberta.
Overall, 8% had low levels (< 2 ng/mL) which does not necessarily reflect recent use of cannabis or
increased risk of crashing. However, 5.9% had THC ≥ 2 ng/mL which usually indicates recent use of
cannabis, and 2.9% had THC ≥ 5 ng/mL which indicates recent use and is often associated with impairment.
In terms of age differences, driving positive for any amount of THC was highest in the 19-24 age group
(27.7%), followed by the 16-18 age group (19.8%) and 25-34 group (17.4%). It was least common in the
55+ age group (6.5%). Similarly, driving with a blood THC concentration of 2 ng/mL or higher was more
frequent in the 19-24 group (13.3%), followed by the 16-18 group (7.2%) and 25-34 group (6%). It was least
common in the 45-54 age group (2.5%). Finally, driving with a blood THC concentration of 5 ng/mL or higher
was more frequent in the 19-24 group (5.4%), followed by the 35-44 group (3.8%) and 25-34 group (3.6%).
It was least common in the 45-54 group (0.9%).
In terms of sex differences, driving while positive for any amount of THC was higher among males (16.2%)
compared to females (9.5%). Similarly, driving with a blood THC concentration of 2 ng/mL was higher
among males (6.9%) compared to females (3.9%). Finally, driving with a blood THC concentration of 5
ng/mL or higher was more frequent among males (3.4%) compared to females (2%)
Alcohol. Overall, 15.6% had been drinking (BAC > 0), and 12.9% had a BAC ≥ 0.08%. Driving after any
alcohol was highest in the 25-34 age group (23.7%), followed by the 19-24 age group (20.9%) and 35-44
age group (18.9%). It was least common in the 55+ age group (8.1%). Similarly, driving while over the legal
limit was more frequent in the 25-34 group (19.3%), followed by the 19-24 group (17.3%) and 35-44 group
(17.3%). It was least common in the 55+ group (5.6%). It is well known that drivers with BAC > 0.08%,
especially younger drivers, have a very high crash risk
6, 72, 73
.
In terms of sex differences, driving after any alcohol was more frequent among males (17.6%) compared to
females (11.9%). Similarly, driving while over the legal limit was more frequent among males (14.2%)
compared to females (10.5%)
Recreational drugs, sedating medications, and opiates. Cocaine, amphetamines, sedating medications
and opiates are known to impair the psychomotor skills required for safe driving.
55, 74
The crash risk

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 14 of
42
associated with these substances is also poorly defined but appears to be less than that associated with
alcohol and in the range of that associated with cannabis.
72
Recreational drugs (cocaine, amphetamines) were detected in one in eight (12.9%) drivers. The highest
prevalence of recreational drugs was found in drivers between the ages of 35 and 44 (20.1%) with increased
prevalence in males (14.4%) compared to females (10%).
Sedating medications were found in one in three (29.3%) drivers with a higher prevalence in females
(37.7%) than males (24.8%). The highest prevalence of sedating medications was found in drivers aged
55+ (35.5%).
Opiates were detected in one in seven (14.3%) drivers and were similarly prevalent in male drivers (14.6%)
and female drivers (13.9%). They were most common in the 35-44 age group (15.6%). These results are
shown in Table 1 and figures 11 and 12.
Strengths
Our methods have several advantages. We measured drugs in blood, which, for THC and most other drugs,
correlates better with impairment and/or recent use than drug levels measured in saliva or urine. Our
methods quantify alcohol, THC and over 80 other impairing drugs and medications. Further, we use blood
obtained shortly after the crash, in most cases within 2.0 hours, so our toxicology results closely
approximate drug levels at time of crash.
18
This short time interval between crash and blood draw simplifies
interpretation of toxicology findings. Third, the decision to obtain blood is not based on suspicion of drug
use: blood is obtained when clinically indicated for managing the patient’s injuries, based on crash
mechanism and/or physical examination. This process eliminates the selection bias that would occur if drug
testing was based on suspicion of drug use. Also, because this study has ethics approval for waiver of
consent due to our innovative methods of anonymizing linked data, we avoid the bias that would arise if
drivers who used drugs were less likely to consent for testing, as might be the case in roadside surveys.
Most important, we study recent drug use in a relevant population (drivers injured in a crash).
Limitations
There are also several limitations to this study. Because we rely on blood that was obtained for clinical
purposes, we do not have control over which drivers are actually tested. As a result, our sample does not
include minimally injured drivers even if they caused a crash that seriously injured another road user. It is
also possible that the decision to obtain blood tests varies from hospital to hospital which may make results
from different hospitals difficult to compare. Although we aim to exclude “post-crash” medications, these
medications may not always be listed in ED records. In particular, we exclude ketamine from this report
since it is commonly administered as part of clinical care in the prehospital setting and we suspect it is not
always documented in the available medical charts. Another limitation is that our toxicology analysis is
unable to measure inhalants (such as toluene). We suspect that inhalant abuse is rare but are unable to
prove that this is the case. A final limitation is that we do not examine, or interview injured drivers and are
unable to assess their whether drivers are actually impaired.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 15 of
42
Summary
Driving after cannabis use appears to be an emerging problem in Canada; however, alcohol remained the
most commonly detected single impairing substance in Alberta in this sample of injured drivers. Given the
very high crash risk associated with alcohol, and the fact that most “cannabis positive” drivers had low THC
levels, it can be concluded that driving after drinking remains a bigger problem in Alberta. Sedating
medications, opiates, and other recreational drugs were also commonly detected. Another striking feature
of this study was the prevalence of polysubstance use, with approximately one in five drivers (22.4%) testing
positive for more than one impairing substance which is above the same of national average of 21%. Social
marketing campaigns or traffic policy designed to prevent impaired driving should continue to target alcohol
as well as cannabis and other drugs and should be sensitive to the fact that many drivers use combinations
of multiple impairing substances. The high prevalence of sedating medications, in multiple age ranges,
suggests the need for better education on prescription practices and on use of sedating medications by
drivers (including over the counter antihistamines).

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 16 of
42
Appendix A: Tables
Table 1. Count (percent) of injured drivers who test positive for impairing substances in Alberta by age
and sex. ......................................................................................................................................................... 17
Table 2. Count (percent) of injured drivers who test positive for impairing substances in Alberta by crash
characteristics. .............................................................................................................................................. 18
Table 3. Count (percent) of injured drivers who test positive for impairing substances in Alberta versus
across Canada. .............................................................................................................................................. 19
Table 4. Polysubstance Use: Count (percent) of injured drivers who test positive for one or more classes
of impairing substance in Alberta versus across Canada. ............................................................................ 20

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 17 of
42
Table 1. Count (percent) of injured drivers who test positive for impairing substances in Alberta by
age and sex.
Notes:
1. “CNS Stimulants” include cocaine, methamphetamine, and other amphetamines.
2. “CNS Depressants” include antihistamines, antidepressants, anticonvulsants, antipsychotics, benzodiazepines, muscle relaxants, tricyclic
antidepressants, and Z-drugs
3. “Any substance” refers to detection of any one (or more) of the following: Alcohol, THC (excludes COOH-THC), CNS stimulants, CNS
depressants, and opioids.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 18 of
42
Table 2. Count (percent) of injured drivers who test positive for impairing substances in Alberta by
crash characteristics.
Notes:
1. “CNS Stimulants” include cocaine, methamphetamine, and other amphetamines.
2. “CNS Depressants” include antihistamines, antidepressants, anticonvulsants, antipsychotics, benzodiazepines, muscle relaxants, tricyclic
antidepressants, and Z-drugs
3. “Any substance” refers to detection of any one (or more) of the following: Alcohol, THC (excludes COOH-THC), CNS stimulants, CNS
depressants, and opioids.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 19 of
42
Table 3. Count (percent) of injured drivers who test positive for impairing substances in Alberta
versus across Canada.
Notes:
1. “CNS Stimulants” include cocaine, methamphetamine, and other amphetamines.
2. “CNS Depressants” include antihistamines, antidepressants, anticonvulsants, antipsychotics, benzodiazepines, muscle relaxants, tricyclic
antidepressants, and Z-drugs
3. “Any substance” refers to detection of any one (or more) of the following: Alcohol, THC (excludes COOH-THC), CNS stimulants, CNS
depressants, and opioids.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 20 of
42
Table 4. Polysubstance Use: Count (percent) of injured drivers who test positive for one or more
classes of impairing substance in Alberta versus across Canada.
Notes:
1. “CNS Stimulants” include cocaine, methamphetamine, and other amphetamines.
2. “CNS Depressants” include antihistamines, antidepressants, anticonvulsants, antipsychotics, benzodiazepines, muscle relaxants, tricyclic
antidepressants, and Z-drugs
3. “Any substance” refers to detection of any one (or more) of the following: Alcohol, THC (excludes COOH-THC), CNS stimulants, CNS
depressants, and opioids.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 21 of
42
Appendix B: Figures
Figure 1. Prevalence of alcohol use among injured drivers in Alberta, by age group. ................................. 22
Figure 2. Prevalence of alcohol use among injured drivers in Alberta, by sex. ............................................ 23
Figure 3. Prevalence of alcohol use among injured drivers in Alberta, by disposition. ............................... 24
Figure 4. Prevalence of alcohol use among injured drivers in Alberta, by time of crash. ............................ 25
Figure 5. Prevalence of alcohol use among injured drivers in Alberta, by number of vehicles involved in
the crash........................................................................................................................................................ 26
Figure 6. Prevalence of cannabinoids among injured drivers in Alberta, by age group. .............................. 27
Figure 7. Prevalence of cannabinoids among injured drivers in Alberta, by sex. ......................................... 28
Figure 8. Prevalence of cannabinoids among injured drivers in Alberta, by disposition. ............................ 29
Figure 9. Prevalence of cannabinoids among injured drivers in Alberta, by time of crash. ......................... 30
Figure 10. Prevalence of cannabinoids among injured drivers in Alberta, by number of vehicles involved in
the crash........................................................................................................................................................ 31
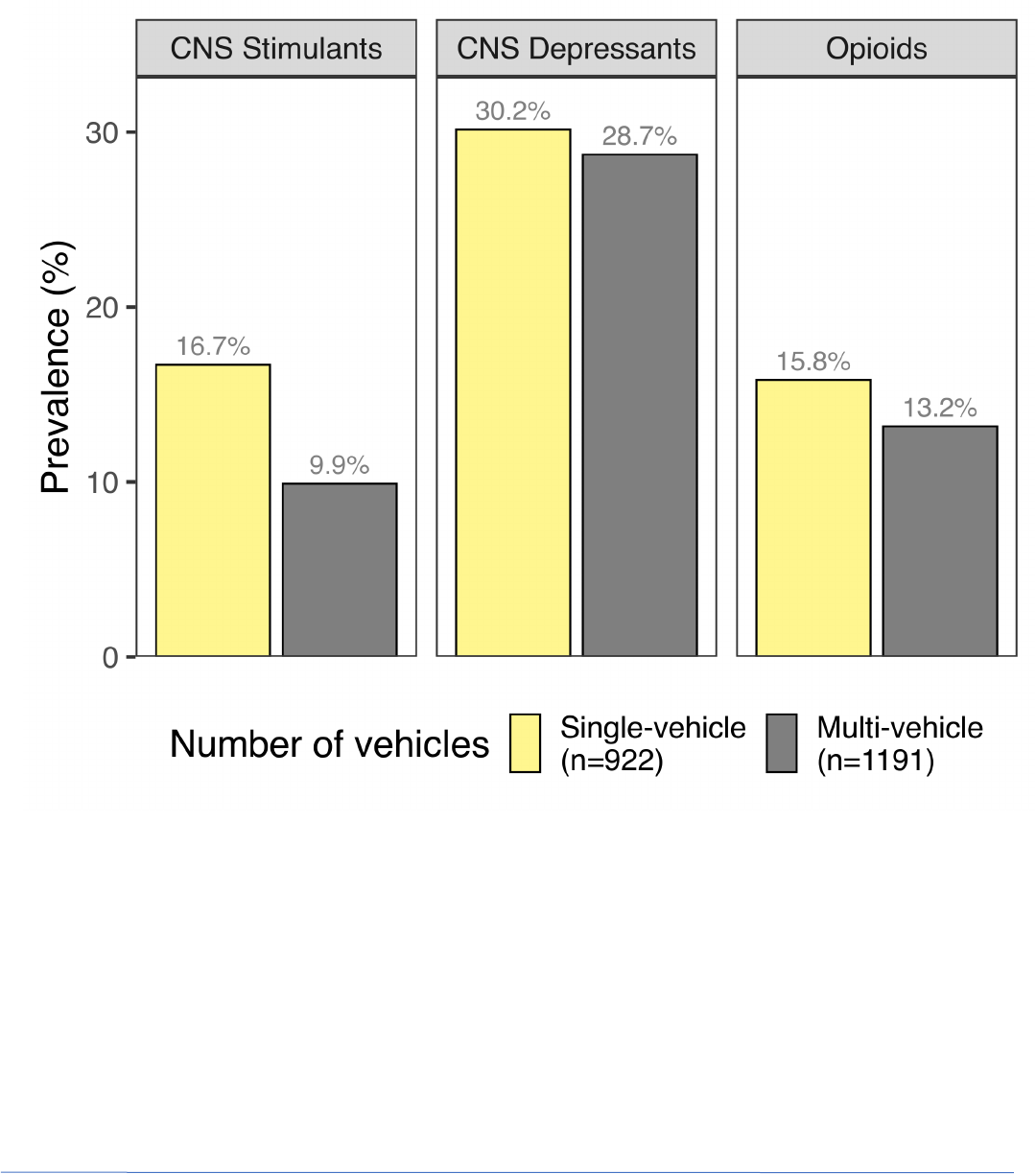
Figure 11. Prevalence of other recreational drugs, medications, and opiates among injured drivers in
Alberta, by age group.................................................................................................................................... 32
Figure 12. Prevalence of other recreational drugs, medications, and opiates among injured drivers in
Alberta, by sex............................................................................................................................................... 33
Figure 13. Prevalence of other recreational drugs, medications, and opiates among injured drivers in
Alberta, by disposition. ................................................................................................................................. 34
Figure 14. Prevalence of other recreational drugs, medications, and opiates among injured drivers in
Alberta, by time of crash. .............................................................................................................................. 35
Figure 15. Prevalence of other recreational drugs, medications, and opiates among injured drivers in
Alberta, by number of vehicles involved in the crash. ................................................................................. 36
Figure 16. Use of alcohol and cannabis among injured drivers in Alberta. .................................................. 37
Figure 17. Polysubstance use among injured drivers in Alberta. ................................................................. 38

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 22 of
42
Figure 1. Prevalence of alcohol use among injured drivers in Alberta, by age group.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 23 of
42
Figure 2. Prevalence of alcohol use among injured drivers in Alberta, by sex.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 24 of
42
Figure 3. Prevalence of alcohol use among injured drivers in Alberta, by disposition.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 25 of
42
Figure 4. Prevalence of alcohol use among injured drivers in Alberta, by time of crash.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 26 of
42
Figure 5. Prevalence of alcohol use among injured drivers in Alberta, by number of vehicles
involved in the crash.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 27 of
42
Figure 6. Prevalence of cannabinoids among injured drivers in Alberta, by age group.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 28 of
42
Figure 7. Prevalence of cannabinoids among injured drivers in Alberta, by sex.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 29 of
42
Figure 8. Prevalence of cannabinoids among injured drivers in Alberta, by disposition.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 30 of
42
Figure 9. Prevalence of cannabinoids among injured drivers in Alberta, by time of crash.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 31 of
42
Figure 10. Prevalence of cannabinoids among injured drivers in Alberta, by number of vehicles
involved in the crash.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 32 of
42
Figure 11. Prevalence of other recreational drugs, medications, and opiates among injured drivers
in Alberta, by age group.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 33 of
42
Figure 12. Prevalence of other recreational drugs, medications, and opiates among injured drivers
in Alberta, by sex.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 34 of
42
Figure 13. Prevalence of other recreational drugs, medications, and opiates among injured drivers
in Alberta, by disposition.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 35 of
42
Figure 14. Prevalence of other recreational drugs, medications, and opiates among injured drivers
in Alberta, by time of crash.
National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 36 of
42
Figure 15. Prevalence of other recreational drugs, medications, and opiates among injured drivers
in Alberta, by number of vehicles involved in the crash.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 37 of
42
Figure 16. Use of alcohol and cannabis among injured drivers in Alberta.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 38 of
42
Figure 17. Polysubstance use among injured drivers in Alberta.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 39 of
42
References
1. Hunault CC, Bocker KB, Stellato RK, Kenemans JL, de Vries I, Meulenbelt J. Acute subjective effects after
smoking joints containing up to 69 mg Delta9-tetrahydrocannabinol in recreational users: a randomized, crossover
clinical trial. Psychopharmacology (Berl). 2014;231(24):4723-33.
2. Karschner EL, Swortwood MJ, Hirvonen J, Goodwin RS, Bosker WM, Ramaekers JG, et al. Extended plasma
cannabinoid excretion in chronic frequent cannabis smokers during sustained abstinence and correlation with
psychomotor performance. Drug Testing & Analysis. 2016;8(7):682-9.
3. Smith HW, Popham RE. Blood alcohol levels in relation to driving. Canadian Medical Association Journal.
1951;65(4):325-8.
4. Borkenstein RF, Crowther RF, Shumate RP, Ziel WB, Zylman R. The role of the drinking driver in traffic
accidents (the Grand Rapids Study). Blutalcohol. 1974;11 (Suppl):7-13.
5. Zador PL, Krawchuk SA, Voas RB. Alcohol-related relative risk of driver fatalities and driver involvement in
fatal crashes in relation to driver age and gender: an update using 1996 data. Journal of studies on alcohol.
2000;61(3):387-95.
6. Blomberg RD, Peck RC, Moskowitz H, Burns M, Fiorentino D. The Long Beach/Fort Lauderdale relative risk
study. Journal of safety research. 2009;40(4):285-92.
7. Tippetts AS, Voas RB, Fell JC, Nichols JL, Tippetts AS, Voas RB, et al. A meta-analysis of .08 BAC laws in 19
jurisdictions in the United States. Accident Analysis & Prevention. 2005;37(1):149-61.
8. Tay R. The effectiveness of enforcement and publicity campaigns on serious crashes involving young male
drivers: Are drink driving and speeding similar? Accident Analysis & Prevention. 2005;37(5):922-9.
9. Tay R. Drink driving enforcement and publicity campaigns: are the policy recommendations sensitive to
model specification? Accident Analysis & Prevention. 2005;37(2):259-66.
10. Rothschild ML, Mastin B, Miller TW. Reducing alcohol-impaired driving crashes through the use of social
marketing. Accident Analysis & Prevention. 2006;38(6):1218-30.
11. Asbridge. The criminalization of impaired driving in Canada: Assessing the deterrent impact of Canada's
first per se law. Journal of studies on alcohol. 2004;65(4):450.
12. Simpson H, Singhal D, Vanlaar W, Mayhew D. The road safety monitor: Drugs and driving. Ottawa, Ontario,
Canada: Traffic Injury Research Foundation; 2006.
13. Ialomiteanu AR, Hamilton HA, Adlaf EM, Mann RE. Substance Use, Mental Health and Well Being Among
Ontario Adults. Toronto, Ontario: Centre for Addictions and Mental Health; 2016.
14. Beasley E, Beirness D. Drug use by fatally injured drivers in Canada. (2000 - 2008). Ottawa, ON: Canadian
Centre on Substance Abuse. 2011.
15. Beasley E, Beirness D. Drug and Alcohol use among Drivers - the 2010 BC Roadside Survey. BC Injury
Prevention Conference; Vancouver2010.
16. Beirness D, Beasley E, McClafferty K. Alcohol and drug use among drivers in Ontario: Findings from the
2014 roadside survey Toronto, Ontario: Ontario Ministry of Transportation; 2015.
17. Solomon R, Clarizio M. Total Crash Deaths Involving Alcohol and/or Drugs in Canada, by Jurisdiction: 2012.
London, Ontario: MADD Canada; 2016 April 19.
18. Brubacher JR, Chan H, Martz W, Schreiber W, Asbridge M, Eppler J, et al. Prevalence of alcohol and drug
use in injured British Columbia drivers. BMJ Open. 2016;6(3).
19. Hartman RL, Brown TL, Milavetz G, Spurgin A, Pierce RS, Gorelick DA, et al. Cannabis effects on driving
lateral control with and without alcohol. Drug Alcohol Depend. 2015;154:25-37.
20. Downey LA, King R, Papafotiou K, Swann P, Ogden E, Boorman M, et al. The effects of cannabis and alcohol
on simulated driving: influences of dose and experience. Accident Analysis & Prevention. 2013;50:879-86.
21. Dubois S, Mullen N, Weaver B, Bédard M. The combined effects of alcohol and cannabis on driving: Impact
on crash risk. Forensic Sci Int. 2015;248:94-100.
22. Ronen A, Gershon P, Drobiner H, Rabinovich A, Bar-Hamburger R, Mechoulam R, et al. Effects of THC on
driving performance, physiological state and subjective feelings relative to alcohol. Accid Anal Prev.
2008;40(3):926-34.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 40 of
42
23. Grotenhermen F, Leson G, Berghaus G, Drummer OH, Krüger HP, Longo M, et al. Developing Science-Based
Per Se Limits for Driving under the Influence of Cannabis (DUIC): Findings and Recommendations by an Expert
Panel. Report. Washington, DC: International Association for Cannabis as Medicine; 2005 September.
24. Sewell RA, Poling J, Sofuoglu M, Sewell RA, Poling J, Sofuoglu M. The effect of cannabis compared with
alcohol on driving. American Journal on Addictions. 2009;18(3):185-93.
25. Ramaekers JG, Berghaus G, van Laar M, Drummer OH. Dose related risk of motor vehicle crashes after
cannabis use. Drug & Alcohol Dependence. 2004;73(2):109-19.
26. Berghaus G, Scheer N, Schmidt P, editors. Effects of Cannabis on Psychomotor Skills and Driving
Performance - a Metaanalysis of Experimental Studies. International Council on Alcohol Drugs and Traffic Safety
(ICADTS); 1995; Adelaide, Australia.
27. Grotenhermen F, Leson G, Berghaus G, Drummer OH, Kruger HP, Longo M, et al. Developing limits for
driving under cannabis. Addiction. 2007;102(12):1910-7.
28. Berghaus G, Sticht G, Grellner W, Lenz D, Naumann T, Wiesenmuller S. Meta-analysis of empirical studies
concerning the effects of medicines and illegal drugs including pharmacokinetics on safe driving. 2010.
29. Vindenes V, Jordbru D, Knapskog A-B, Kvan E, Mathisrud G, Slordal L, et al. Impairment based legislative
limits for driving under the influence of non-alcohol drugs in Norway. Forensic Sci Int. 2012;219(1-3):1-11.
30. Desrosiers NA, Ramaekers JG, Chauchard E, Gorelick DA, Huestis MA. Smoked cannabis' psychomotor and
neurocognitive effects in occasional and frequent smokers. J Anal Toxicol. 2015;39(4):251-61.
31. Broyd SJ, van Hell HH, Beale C, Yucel M, Solowij N. Acute and Chronic Effects of Cannabinoids on Human
Cognition-A Systematic Review. Biol Psychiatry. 2016;79(7):557-67.
32. Colizzi M, Bhattacharyya S. Cannabis use and the development of tolerance: a systematic review of human
evidence. Neuroscience and biobehavioral reviews. 2018;93:1-25.
33. Soar K, Mason C, Potton A, Dawkins L. Neuropsychological effects associated with recreational cocaine use.
Psychopharmacology. 2012;222(4):633-43.
34. Ramaekers JG, Kuypers KPC, Bosker WM, Brookhuis KA, Veldstra JA, Simons R, et al. Effects of stimulant
drugs on actual and simulated driving: perspectives from four experimental studies conducted as part of the DRUID
research consortium. Psychopharmacology. 2012;222(3):413-8.
35. Wittmann M, Leland DS, Churan J, Paulus MP. Impaired time perception and motor timing in stimulant-
dependent subjects. Drug & Alcohol Dependence. 2007;90(2-3):183-92.
36. Fillmore MT, Rush CR, Hays L. Acute effects of oral cocaine on inhibitory control of behavior in humans.
Drug Alcohol Depend. 2002;67(2):157-67.
37. Rush CR, Baker RW, Wright K. Acute physiological and behavioral effects of oral cocaine in humans: a dose-
response analysis. Drug & Alcohol Dependence. 1999;55(1-2):1-12.
38. Foltin RW, Fischman MW, Pippen PA, Kelly TH. Behavioral effects of cocaine alone and in combination with
ethanol or marijuana in humans. Drug & Alcohol Dependence. 1993;32(2):93-106.
39. Smith JL, Mattick RP, Jamadar SD, Iredale JM. Deficits in behavioural inhibition in substance abuse and
addiction: a meta-analysis. Drug & Alcohol Dependence. 2014;145:1-33.
40. Spronk DB, van Wel JH, Ramaekers JG, Verkes RJ. Characterizing the cognitive effects of cocaine: a
comprehensive review. Neurosci Biobehav Rev. 2013;37(8):1838-59.
41. Gustavsen I, Hjelmeland K, Bernard JP, Morland J. Psychomotor performance after intake of zopiclone
compared with intake of ethanol: a randomized, controlled, double-blinded trial. J Clin Psychopharmacol.
2011;31(4):481-8.
42. Conen S, Theunissen EL, Van Oers ACM, Valiente R, Ramaekers JG. Acute and subchronic effects of bilastine
(20 and 40 mg) and hydroxyzine (50 mg) on actual driving performance in healthy volunteers. Journal of
Psychopharmacology. 2011;25(11):1517-23.
43. Zacny JP, Lichtor SA. Within-subject comparison of the psychopharmacological profiles of oral oxycodone
and oral morphine in non-drug-abusing volunteers. Psychopharmacology. 2008;196(1):105-16.
44. Leufkens TR, Vermeeren A, Smink BE, van Ruitenbeek P, Ramaekers JG, Leufkens TRM, et al. Cognitive,
psychomotor and actual driving performance in healthy volunteers after immediate and extended release
formulations of alprazolam 1 mg. Psychopharmacology (Berl). 2007;191(4):951-9.
45. Wingen M, Ramaekers JG, Schmitt JA, Wingen M, Ramaekers JG, Schmitt JAJ. Driving impairment in
depressed patients receiving long-term antidepressant treatment. Psychopharmacology. 2006;188(1):84-91.
46. Verster JC, Veldhuijzen DS, Patat A, Olivier B, Volkerts ER. Hypnotics and driving safety: meta-analyses of
randomized controlled trials applying the on-the-road driving test. Curr Drug Saf. 2006;1(1):63-71.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 41 of
42
47. Wingen M, Bothmer J, Langer S, Ramaekers JG. Actual driving performance and psychomotor function in
healthy subjects after acute and subchronic treatment with escitalopram, mirtazapine, and placebo: a crossover
trial. Journal of Clinical Psychiatry. 2005;66(4):436-43.
48. Bramness JG, Skurtveit S, Morland J. Testing for benzodiazepine inebriation--relationship between
benzodiazepine concentration and simple clinical tests for impairment in a sample of drugged drivers. European
Journal of Clinical Pharmacology. 2003;59(8-9):593-601.
49. Hill JL, Zacny JP. Comparing the subjective, psychomotor, and physiological effects of intravenous
hydromorphone and morphine in healthy volunteers. Psychopharmacology. 2000;152(1):31-9.
50. Hanks GW, O'Neill WM, Simpson P, Wesnes K. The cognitive and psychomotor effects of opioid analgesics.
II. A randomized controlled trial of single doses of morphine, lorazepam and placebo in healthy subjects. European
Journal of Clinical Pharmacology. 1995;48(6):455-60.
51. Volz HP, Sturm Y. Antidepressant drugs and psychomotor performance. A review. Neuropsychobiology.
1995;31(3):146-55.
52. Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk:
systematic review of observational studies and meta-analysis. BMJ. 2012;344.
53. Li MC, Brady JE, DiMaggio CJ, Lusardi AR, Tzong KY, Li G. Marijuana use and motor vehicle crashes.
Epidemiol Rev. 2012;34:65-72.
54. Rogeberg O, Elvik R. The effects of cannabis intoxication on motor vehicle collision revisited and revised.
Addiction. 2016;111(8):1348-59.
55. Drug use and road safety: a policy brief. Geneva, Switzerland: World Health Organization; 2016.
56. Elvik R. Risk of road accident associated with the use of drugs: A systematic review and meta-analysis of
evidence from epidemiological studies. Accid Anal Prev. 2013;60(0):254-67.
57. Hels T, Lyckegaard A, Simonsen KW, Steentoft A, Bernhoft IM. Risk of severe driver injury by driving with
psychoactive substances. Accid Anal Prev. 2013;59:346-56.
58. Compton RP, Berning A. Drug and Alcohol Crash Risk. National Highway Traffic Safety Administration.
Washington, D.C.; 2015. Report No.: DOT HS 812 117.
59. Beirness DJ, Beasley EE. A roadside survey of alcohol and drug use among drivers in British Columbia.
Traffic Inj Prev. 2010;11(3):215-21.
60. Beirness D, Swann P, Logan BK. Drugs and driving: Detection and deterrence. Paris, France: International
Transport Forum OECD; 2010.
61. Beirness D, Beasley E. An evaluation of immediate roadside prohibitions for drinking drivers in British
Columbia: Findings from roadside surveys. Traffic Inj Prev. 2014;15(3):228-33.
62. Calapai F, Cardia L, Sorbara EE, Navarra M, Gangemi S, Calapai G, et al. Cannabinoids, Blood-Brain Barrier,
and Brain Disposition. Pharmaceutics. 2020;12(3).
63. Robertson MB, Li A, Yuan Y, Jiang A, Gjerde H, Staples JA, et al. Correlation between oral fluid and blood
THC concentration: A systematic review and discussion of policy implications. Accid Anal Prev. 2022;173:106694.
64. Brown SW, Vanlaar WGM, Robertson RD. The Alcohol and Drug Crash Problem in Canada 2016 Report.
Ottawa, Canada: The Traffic Injury Research Foundation of Canada; 2021.
65. Brunet B, Hauet T, Hebrard W, Papet Y, Mauco G, Mura P. Postmortem redistribution of THC in the pig.
International journal of legal medicine. 2010;124(6):543-9.
66. Holland MG, Schwope DM, Stoppacher R, Gillen SB, Huestis MA. Postmortem redistribution of Delta9-
tetrahydrocannabinol (THC), 11-hydroxy-THC (11-OH-THC), and 11-nor-9-carboxy-THC (THCCOOH). Forensic Sci Int.
2011;212(1-3):247-51.
67. Lemos NP, Ingle EA. Cannabinoids in postmortem toxicology. J Anal Toxicol. 2011;35(7):394-401.
68. Pounder DJ, Jones GR. Post-mortem drug redistribution--a toxicological nightmare. Forensic Sci Int.
1990;45(3):253-63.
69. Yarema MC, Becker CE. Key concepts in postmortem drug redistribution. Clin Toxicol (Phila).
2005;43(4):235-41.
70. Brubacher JR, Chan H, Erdelyi S, Asbridge M, Mann RE, Purssell RA, et al. Police documentation of drug use
in injured drivers: Implications for monitoring and preventing drug-impaired driving. Accid Anal Prev. 2018.
71. Mann RE, Stoduto G, Ialomiteanu A, Asbridge M, Smart RG, Wickens CM. Self-reported collision risk
associated with cannabis use and driving after cannabis use among Ontario adults. Traffic Inj Prev. 2010;11(2):115-
22.

National Drug Driving Study
-Alberta progress report
APRIL 15, 2024 | Project Update
Page 42 of
42
72. Brubacher JR, Chan H, Erdelyi S, Macdonald S, Asbridge M, Mann RE, et al. Cannabis use as a risk factor for
causing motor vehicle crashes: a prospective study. Addiction. 2019.
73. Peck RC, Gebers MA, Voas RB, Romano E. The relationship between blood alcohol concentration (BAC),
age, and crash risk. Journal of Safety Research. 2008;39(3):311-9.
74. Schulze H, Schumacher M, Urmeew R, Alvarez J, Bernhoft IM, de Gier H, et al. Driving under the influence
of drugs, alcohol and medicines in Europe—findings from the DRUID project. Lisbon, Portugal: European
Monitoring Centre for Drugs and Drug Addiction; 2012.
