
Enhancing concurrent capability:
A toolkit for managers and staff
Addiction and Mental Health
June 2016
Integrated treatment
planning
Contents
Introduction ..................................................................... 5
Integrated treatment planning .............................................7
Clinical decision making: Integrated treatment planning ...10
Standard approach to concurrent capable practice ............11
You’re already treatment planning ..................................... 13
What is a treatment plan? .................................................15
Elements of integrated treatment planning .......................18
The steps to integrated treatment planning ......................24
Successful integrated treatment planning ..........................30
It’s not just the plan—it’s you! ...........................................29
Conclusion ........................................................................33
Appendices
1. Examples of integrated treatment models ....................34
2. Sample plan templates .................................................36
3. Cultural safety and cultural competency resources .......38
4. Understanding stages of change and
stages of treatment .....................................................39
5. HONOS adult tool ........................................................40
6. Sample case conference presentation format ..................
41
References .........................................................................42
Copyright © (2016) Alberta Health Services. This material is protected by Canadian and other international
copyright laws. All rights reserved. This material may not be copied, published, distributed or reproduced in any
way in whole or in part without the express written permission of Alberta Health Services (please contact Senior
Program Officer at Community, Seniors, Addiction and Mental Health at [email protected]).
This material is intended for general information only and is provided on an “as is”, “where is” basis. Although
reasonable efforts were made to confirm the accuracy of the information, Alberta Health Services does not
make any representation or warranty, express, implied or statutory, as to the accuracy, reliability, completeness,
applicability or fitness for a particular purpose of such information. This material is not a substitute for the
advice of a qualified health professional. Alberta Health Services expressly disclaims all liability for the use of
these materials, and for any claims, actions, demands or suits arising from such use.

Integrated treatment planning
— 3 —
Enhancing concurrent capability: A toolkit
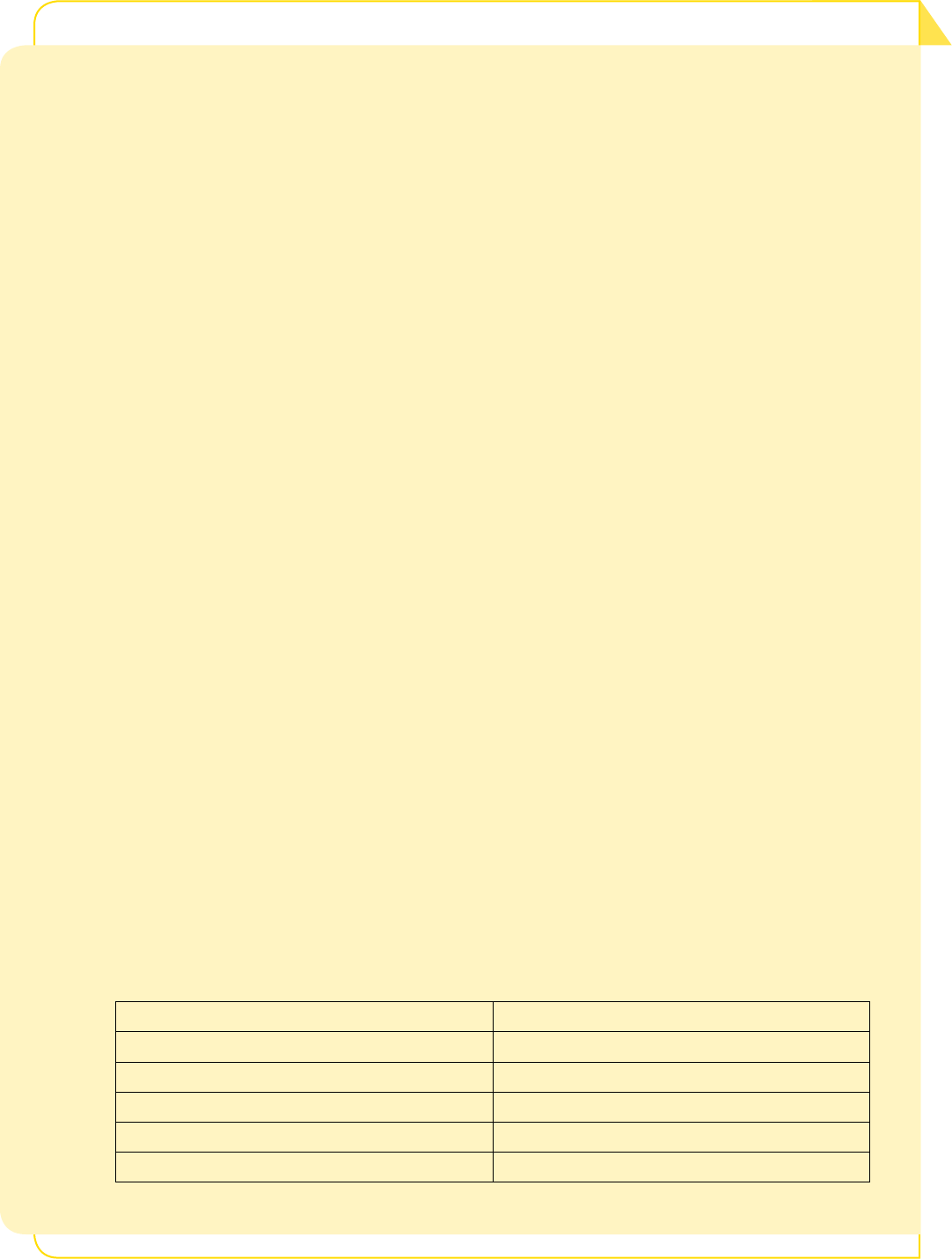
Table of Contents
Introduction .......................................................................................................5
How was this toolkit chapter created? ..................................................................5
Learning objectives ...............................................................................................6
Terms and definitions ...........................................................................................6
Integrated treatment planning ........................................................................7
What is integrated treatment planning? ...............................................................7
Goals of integrated treatment planning ................................................................8
Clinical decision making: Integrated treatment planning ...........................10
Clinical decision-making process ........................................................................10
Standard approach to concurrent capable practice .....................................11
You’re already treatment planning ...............................................................13
What is a treatment plan? ..............................................................................15
The treatment plan ............................................................................................15
Elements of integrated treatment planning .................................................18
Understanding stages of change and stages of treatment ..................................23
The steps to integrated treatment planning ...............................................24
Setting SMART goals .........................................................................................26
Successful integrated treatment planning....................................................30
It’s not just the plan—it’s you! .......................................................................31
Conclusion ........................................................................................................33
Appendix 1: Examples of integrated treatment models .............................34
The Integrated Dual Disorder Treatment (IDDT) model ........................................34
Appendix 2: Sample plan templates .............................................................. 36
Appendix 3: Cultural safety and cultural competency resources ...............38
Appendix 4: Understanding stages of change and
stages of treatment ..................................................................39
Appendix 5: HONOS – Addiction and Mental Health, AHS ........................40
Appendix 6: Sample case conference presentation format ........................41
References ........................................................................................................42

Integrated treatment planning
— 5 —
Enhancing concurrent capability: A toolkit
Introduction
How was this toolkit chapter created?
The content for this chapter was developed following a literature
review and discussions within Alberta Health Services to establish what
resources were available and what needed to be included for Addiction
and Mental Health (AMH) related to integrated treatment planning. A
number of relevant websites were reviewed related to specific addiction
and mental health associations and organizations. Content was validated
by a variety of stakeholders, who were part of a provincial reference
group and AMH clinical network. Representation on these committees
was inclusive of the various zones and provincial sectors representing
Addiction and Mental Health.
We would like to acknowledge the work of the participants who helped
create this resource and are grateful for their valuable contributions.
We are committed to matching toolkit content to the needs of the people
who will be using it. We welcome any feedback, questions or suggestions
for additions or revisions to the content. We wish to learn from the
experiences at the front line, so please let us know how well this toolkit
works for you by emailing us at concurrent.disorders@ahs.ca
Acknowledgements and special thanks
Sponsors
Barry Andres, Executive Director, Provincial Addiction and
Mental Health (AMH)
Jill Mitchell, Director, Professional Development and
Concurrent Capability, Provincial AMH
Lead
Tracey Labbie, Manager, Concurrent Capability,
Provincial AMH
Reference group participants
Tuxephoni Winsor, Manager, Professional Development,
Provincial AMH
Jennifer Gallivan, Clinical Consultant, Concurrent
Capability, Provincial AMH
Jackie Clark, Clinical Consultant, Concurrent Capability,
Provincial AMH
Peter Churchill, Senior Advisor, Addiction Counselor
Initiative, AMH
Louis Benincasa, Senior Advisor, Professional
Development, Provincial AMH
Treena Tallow, Coordinator, AMHB, Aboriginal
Health Program
Tanya Figg, Manager, AMH, South Zone
Robert Johnston, Manager, AMH, South Zone
Cheryl Korneychuk-Waddy, Clinical Supervisor,
AMH, Calgary Zone
Shannon Middlemiss, Manager, Calgary Corrections,
Calgary Zone
Kelly Orugian, Addiction Counsellor, AMH,
Edmonton Zone
Daniel Scott, Manager, Clinical Education and
Professional Practice, AMH, Edmonton Zone
Craig Staniforth, Manager, AMH, Edmonton Zone
Crystal Van Raay, Manager, Child, Adolescent and
Family AMH, South Zone

Integrated treatment planning
— 6 —
Enhancing concurrent capability: A toolkit
Learning objectives
This chapter will focus on the practical applications of integrated
treatment planning practices for managers and front-line staff that
can be applied to all scenarios. You will learn how to develop an
integrated treatment plan and consider how to improve integrated
treatment planning in your practice.
As with other chapters in this toolkit, we have tried to keep the main
part of the chapter brief. If topics are of further interest to you, there
is detailed information available in the appendices. Throughout the
chapter, you’ll find suggested activities and resources to assist in
developing an integrated treatment plan.
The following topics are covered in this chapter:
• What is integrated treatment planning (ITP)
• Integrated treatment planning as part of clinical decision-making
• Goals of integrated treatment planning
• Elements of an integrated treatment plan
• The steps in developing an integrated treatment plan
• Using motivation-based treatment techniques and setting
SMART goals
• The bigger picture of integrated treatment planning
Terms and definitions
For the purposes of this chapter, the following terms and definitions
will be used:
Family: Persons who are related in any way (biologically, legally or
emotionally), including immediate relatives, extended family, partners,
advocates, cultural supports, guardians and other individuals identified
as being in the individual’s support system.
Individual or person: The person, patient or client in question who
has a concurrent disorder and who is working with clinicians, family
and/or others on recovery, treatment or care. These two terms will be
used interchangeably.

Integrated treatment planning
— 7 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning
What is integrated treatment planning?
Treatment planning is a collaborative approach with the person
experiencing an addiction issue, mental health concern, or both, and
their family. It incorporates health-care services, community supports,
self-help groups and cultural supports (e.g., elders, cultural support
workers) to support recovery outcomes.
An integrated treatment plan should be developed with the person
and their family, and in consultation or collaboration with other
addiction and/or mental health services. If additional concurrent
concerns become apparent during the assessment or treatment
planning phases, there should be ongoing consultation and
collaboration with all services and clinicians to provide the most
appropriate care. Other areas of support that ensure basic life needs
are being met should also be part of the coordinated care and
treatment plan, such as housing and employment, and cultural and
traditional practices.
Broadly defined, integrated treatment is “any mechanism by which
treatment interventions for [concurrent disorders] are combined
within the context of a primary treatment relationship or service
setting” (SAMHSA, 2003). One clinician or treatment team takes overall
responsibility for blending treatment and support interventions into
one coherent package (Drake et al., 2004).
Historical context for integrated treatment for concurrent disorders
Historically, treatment for substance abuse disorders has been done
in isolation from other health-care systems. This forces patients and
families to have to choose which system to seek treatment in (Miller et
al., 2011).
The concept of integrated treatment was developed to respond to the
difficulties clients had when navigating between substance abuse and
mental health systems (Drake and Mueser, 2000).
Parallel treatment systems are an issue for people with concurrent
disorders. Whether patients are working with hospitals, corrections
facilities or community health services, all clinicians and treatment

Integrated treatment planning
— 8 —
Enhancing concurrent capability: A toolkit
teams should work together in a coordinated, integrated manner to
remove this treatment barrier (CCSA, 2009).
Key messages
Integrated treatment planning is a way of making sure that treatment is
seamless, coordinated and comprehensive.
It is inclusive of the person seeking treatment, the person’s family
members and the clinician and/or treatment team.
Integrated treatment planning works best when the person has a trusting
relationship with one case manager (e.g., a health-care professional or
therapist) and supports fostering a culturally safe environment. Working
with a team of professionals and programs may be required to treat the
individual, but one clinician should be responsible for coordinating and
overseeing the treatment or recovery plan.
The degree of collaboration may differ for each person depending on
their diagnosis, recovery goals and treatment strategies.
Goals of integrated treatment planning
At the service level, the goals for integrated treatment planning are to
improve access, quality of care and health outcomes. Overall benefits
of integrated treatment planning include
• meeting the person’s needs in a timely manner
• reducing the need for the person seeking services to navigate
complex health systems
• providing a measure for tracking progress and successes
•
providing a forum for engagement with the person and their family
• an opportunity for health professionals to offer information and
education
• communicating actions, intentions and goals
• ensuring treatment effectively targets the individual’s needs and is
strengths-based, building on skills and using available resources
• providing multidisciplinary staff with a common understanding
and language about the assessment and treatment planning
process

Integrated treatment planning
— 9 —
Enhancing concurrent capability: A toolkit
• providing health professionals with the sense that their work is
effective and meaningful
Alberta Health Services’s Patient First Strategy can be applied to
working with individuals with concurrent disorders. This strategy
strengthens AHS’s culture and practices to fully embrace patient- and
family-centred care (PFCC).
This model of care sees [individuals] and families
as integral members of the health-care team,
and encourages their active participation in all
aspects of care, including as partners in planning,
implementation and evaluation of existing and future
care and services (Alberta Health Services, 2015)
More information about the Patient First Strategy can be found here:
http://www.albertahealthservices.ca/assets/info/pf/first/if-pf-1-pf-strategy.
pdf.
Other evidence-informed practice for treating concurrent disorders
that have been studied and promoted as a best practice include the
following:
• Integrated dual disorder treatment (IDDT) model
The IDDT evidence-based practice involves cross-trained
practitioners providing integrated, comprehensive services to
individuals with concurrent disorders simultaneously in the same
venue, with the goal of recovery from both illnesses.
• Integrated placement and support (IPS) model
The IPS model supports employment for individuals with mental
illness who want to work in competitive settings.
More detailed information on both of these models, as well as the
history of integrated treatment planning, can be found in Appendix 1.

Integrated treatment planning
— 10 —
Enhancing concurrent capability: A toolkit
Clinical decision making: Integrated treatment planning
As discussed in the “Standard approach to screening” and
“Comprehensive assessment” chapters, screening, assessment and
treatment planning can overlap, but they also have unique qualities
and follow a progressive timeline. The sequencing of the three
activities makes sense, as each process builds on the others (see
below). Between each process is a decision point where the clinician,
in collaboration with the individual and their family, decides what to
do next. For integrated treatment planning, the decision points and the
overall process should appear seamless even when multiple clinicians
or program areas are involved.
Clinical decision-making process
SCREENING
Identifies the
possibility of
a problem
Usually done very early,
i.e. at initial contact
Outcome is often
immediate action
(assessment,
referral to services)
1
Universal (all who
enter treatment)
Usually brief
2
Can be
self-administered
ASSESSMENT
Gathers detailed
information about the
nature and extent of
the problem(s)
and strengths
Usually done after the
need for assessment
has been determined
Outcome is detailed
information that forms
the base for the
treatment plan
More selective
and targeted
Usually lengthier
2
Usually done
in person
TREATMENT
PLANNING
Develop treatment
goals, choose
interventions or
programs to attain
the goals.
Monitor progress
and adjust
treatment plan
as needed.
DECISION POINT
DECISION POINT
DECISION POINT
1
While assessment may identify immediate needs, it is usually more concerned with longer-term
treatment planning and service co-ordination.
2
Some assessment tools may actually be briefer than some screening tools if the assessment tool focuses
only on specific disorders, and the screening tool is multidimensional in its coverage.

Integrated treatment planning
— 11 —
Enhancing concurrent capability: A toolkit
Standard approach to concurrent capable practice
The Standard Approach to Concurrent Capable Practice Algorithm
outlines a process for delivering concurrent capable care. Developing
an integrated treatment plan should be person-centred, trauma-
informed and recovery-oriented. It is important to recognize that even
though the process has certain steps, it is also cyclical in nature and is
a process of ongoing re-assessment and continuous care that changes
as goals are met and priorities shift.
Integrated treatment planning requires that clinicians understand
when the process requires you to keep and consult with the person
seeking treatment, and when to provide a warm handoff to another
clinician or program. This decision will be discussed throughout
the chapter.

Integrated treatment planning
— 12 —
Enhancing concurrent capability: A toolkit
A standard approach to concurrent capable practice
First contact with person
EVERY DOOR IS THE RIGHT DOOR…
Concurrent Capable
Addiction Services
Concurrent Enhanced Programs
Integrated AMH Teams
Concurrent Capable
Mental Health Services
WELCOME AND ENGAGE
Observe and gather information on appearance, behav-
iour and cognition (ABC) and review history, while estab-
lishing rapport and engaging individual/family
SCREEN FOR CONCURRENT DISORDERS
Using a reliable tool (GAIN-SS, DSM-V CC, etc.) identify the
presence of a mental health, addiction or concurrent disorder
WARM HANDOFF
• Mental Health
• Addictions
• Concurrent Enhanced
Service
• Community supports
BRIEF
INTERVENTION
• Solution focused
• Single session or more
(5-10)
• Crisis intervention
KEEP AND CONSULT
Consultation, collaboration and
coordination with other service
(addiction or mental health) and
other involved service providers
COMPREHENSIVE
ASSESSMENT
INTEGRATED
TREATMENT
PLANNING
COMPREHENSIVE
INTERVENTIONS
• Recovery oriented,
collaborative process that
is person-centred, trauma
informed and strengths based
• Involves person/family and
other services providers in
care coordination
• Reassessment is ongoing
throughout the recovery
journey with shifts in
treatment planning as needed
CASE
MANAGEMENT
& SERVICE
COORDINATION
CONTINUOUS
CARE
Time unlimited services
using long term
strategies to support
recovery
DISCHARGE
TRANSITION
Copyright © (2016) Alberta Health Services. This material is protected by Canadian and other international copyright laws.

Integrated treatment planning
— 13 —
Enhancing concurrent capability: A toolkit
You’re already treatment planning
Integrated treatment planning is done with the person and their
family, as well as in consultation or collaboration with other service
providers. You must be mindful that you are working with the
individual to establish successful recovery outcomes as they identify
them. As these goals and needs get identified through a collaborative
process, you have already begun thinking about how you can best
support them in their recovery journey. You may also begin deciding
whether the individual requires additional services that are provided
in consultation or collaboration with other services, agencies
or programs.
For example, a person recently referred to your program by her
family physician for alcohol use discloses that she believes her family
is coming into her apartment at night and moving her belongings
around to confuse her. She is angry and refuses to see them. You
administer the GAIN-SS screening tool and identify the possibility of a
mental health disorder.
There are several different outcomes for this person:
First Scenario, (“Keep and Consult”): A risk assessment identifies
no immediate safety risk, so the person is admitted to your service
for counseling. Based on the GAIN-SS scores and the identification
of a mental health disorder, you consult with your mental health
colleague and perhaps invite them to attend the next visit to conduct
a collaborative assessment with the person and their family. The
“consult” part of this scenario means you collaborate and work
together to identify the person’s wishes, goals and desires for
treatment and support them in developing their recovery journey.
Sometimes you may be able to consult and collaborate with your
colleague by telephone, identifying treatment options and next steps;
however, it is important to remember that this involves more than one
phone call and should be ongoing as long as the mental-health issues
are present.
Second Scenario, (“Warm Handoff”): During your conversation, the
person reveals she has a diagnosis of schizoaffective disorder and has
not been taking her medications because she doesn’t like the way they
make her feel. She has not been sleeping, and her appetite and energy

Integrated treatment planning
— 14 —
Enhancing concurrent capability: A toolkit
level are low. She says that alcohol helps her fall asleep at night and
that she drinks 2–3 times per week. She has had two mental health
hospitalizations in the last 18 months. Recognizing that this individual
requires more support than your service can provide, you call the
mental health office to facilitate a referral. If your zone uses a central
intake system, you make the referral and advise that you will stay
involved with the client until she is able to assume service. You might
even accompany her to their first visit to ensure they connect with the
service before discharging her from your caseload.
A warm handoff is more than sending a referral. Here are some tips to
make it more successful:
• Meet face to face with the referral agency and the person and
their family
• Invite the person to meet at the new office next time
• Develop a collaborative relationship with internal and external
community partners
• Call the referral agency and discuss the referral prior to sending
the referral package
• Continue to support the person until their initial visit with the
referral agency

Integrated treatment planning
— 15 —
Enhancing concurrent capability: A toolkit
What is a treatment plan?
A treatment plan is a document that
• is created based on screening and assessment information
• identifies the person’s most important long- and short-term goals
for wellness and recovery through collaboration with the family
• describes SMART goals—specific, measurable, attainable, realistic
and time-limited
• reflects a verbal agreement between
the clinician and the client
A treatment plan is an evolving document.
As goals are met, new information is
acquired or the individual’s status changes,
the treatment plan must be reviewed and
adjusted regularly.
The treatment plan
Treatment plans typically include the following components:
• Name of the person who the plan is about
• Name of the clinician, and the names of any others involved in
the person’s care
• Date of treatment plan
• Presenting issues
• The person’s goals for wellness and recovery
• Actions to support recovery (e.g., employment, recreation/
exercise, suitable housing, peer-support worker, skill building)
• Specific therapies and approaches as prescribed (e.g., medication,
cognitive behavioural therapy, dialectical behavioural therapy,
motivational interviewing)
• Other involved agencies/programs
• Anticipated length treatment and frequency of contact with
the person
• Potential challenges
• Consent of the individual to share this information, as necessary
Treatment plans are also called
• care plans
• service plans
• goal plans
• recovery plans

Integrated treatment planning
— 16 —
Enhancing concurrent capability: A toolkit
• Signature of the individual and clinician, agreeing to the plan
• Timelines for review of the plan (e.g., monthly, weekly)
Ensuring that an integrated treatment plan is effectively developed
means more than just filling out a piece of paper. It requires careful
thought and collaboration with the person and their family, as well as
other team members, agencies, programs and services.
For sample treatment plans, see Appendix 2.
>| suggested activity |<
Have each team member collect
the treatment plan templates
and tools that they use with
individuals seeking treatment.
Compare each tool against the
list above and have them decide
what components are the same
and which are different.
Identify any components that could
be added to the list or any that could
be added to the tools you are already
using.

Integrated treatment planning
— 17 —
Enhancing concurrent capability: A toolkit
The Components of a Person-Centred Treatment Plan
(adapted from Mueser et al., 2003 and Center for Substance Abuse Treatment, 2006)
Acute safety needs Determines the need for immediate acute stabilization
to establish safety prior to routine assessment
Severity of concurrent
disorder
Determines the most appropriate setting for
treatment (see the Quadrant Model, as seen in the
“Comprehensive Assessment” chapter)
Appropriate care setting Determines the client’s program assignments (see the
ASAM Patient Placement Criteria, 2015: http://www.
asam.org/publications/the-asam-criteria/about)
Diagnosis Determines the recommended treatment intervention
Disability Determines case management needs and whether an
enhanced level of intervention is required
Strengths and skills Determines the areas of prior success around
which to organize future treatment interventions
and determines areas of skill-building needed for
management of either disorder
Availability and continuity
of recovery support
Determines whether continuing relationships need to
be established and whether existing relationships are
able to provide contingencies to promote learning
Cultural context Determines culturally appropriate treatment
interventions and settings
Problem priorities Determines specific problems to be solved and
opportunities for contingencies to promote treatment
participation
State of recovery/Client’s
readiness to change
Determines appropriate treatment interventions and
outcomes for a client at a given stage of recovery or
readiness to change

Integrated treatment planning
— 18 —
Enhancing concurrent capability: A toolkit
Elements of integrated treatment planning
Persons with concurrent disorders come from many diverse
groups. There are no universal methods of treatment, because each
person, diagnosis, motivation for recovery, and socio-economic and
environmental situation is unique (Novotna, 2014).
To help understand the unique nature of
integrated treatment planning for persons
with concurrent disorders, consider the
following key elements:
• Trauma-informed approaches to care
• Recovery focused
• Informed consent
• Evidence-informed practice
• Social determinants of health
• Motivation-based treatment
• Cultural competency and safety
This model of care sees patients
and families as integral members
of the health-care team,
and encourages their active
participation in all aspects of care,
including as partners in planning,
implementation and evaluation
of existing and future care and
services.
The Patient First Strategy will
enable us to advance health care
in Alberta by empowering and
enabling Albertans to be at the
centre of their health care team,
improving their own health and
wellness.
“Recovery oriented practice acknowledges the
unique nature of each person’s journey of wellness
and everyone’s right to find their own way to living
a life of value and purpose in the community of
their choice.” (Mental Health Commission of Canada,
Recovery Guidelines, 2015)

Integrated treatment planning
— 19 —
Enhancing concurrent capability: A toolkit
Elements of Integrated Treatment Planning
Element Description Tips and resources
Person-centred A person-centred plan takes into
consideration the client’s values, cultural
preferences, concerns and expectations
in order to achieve their identified goals.
Shared decision making between the
person and clinician works best.
• Use welcoming and engaging
strategies to build a relationship with
the person that makes them feel safe,
comfortable and respected.
• The individual, as well as their family,
as necessary, should be involved
in their treatment planning and
identifying goals for recovery.
Trauma-
informed
approaches to
care
Trauma-informed care recognizes that
it is common for individuals who use
mental health and addiction services to
have experienced trauma that may greatly
influence their ability or willingness to
engage with service providers or programs
for help.
Trauma-informed care does not require that
the person disclose a trauma, but it does
mean that service and care providers must
use practices based on trauma awareness;
safety and trustworthiness; opportunities
for choice, collaboration and connection;
and strengths-based and skill building
(Canadian Centre on Substance Abuse ,
2014).
• Build a trusting relationship with the
individual by being respectful, honest,
clear and responsive.
• Listen to the individual’s story,
acknowledge their emotions and
validate their experiences.
What is Trauma Informed Care? TIC
E-Learning Module A1, MyLearningLink,
Alberta Health Services
http://mylearninglink.
albertahealthservices.ca/elearning/bins/
index.asp
Canadian Centre on Substance Abuse,
Trauma-Informed Care Toolkit
www.ccsa.ca//Resource%20Library/CCSA-
Trauma-informed-Care-Toolkit-2014-en.
pdf
`Registered Nurses’ Association of Ontario.
Engaging Clients Who Use Substances
http://rnao.ca/bpg/guidelines/engaging-
clients-who-use-substances
Integrated treatment planning
— 20 —
Enhancing concurrent capability: A toolkit
Element Description Tips and resources
Recovery-
focused
A recovery-focused perspective means that
providers and clinicians acknowledge that
recovery is a person-driven process that
means different things to different people.
The U.S. Substance Abuse and Mental
Health Services Administration (SAMHSA,
2011) defines recovery from mental
disorders and substance use disorders
as “A process of change through which
individuals improve their health and
wellness, live a self-directed life, and strive
to reach their full potential.”
Recovery might also mean
• hope
• support
• personal responsibility
• dignity
• education
• self-advocacy
• Have the individual identify what
recovery means to them.
• Recognize that recovery is a journey
and is unique to each person.
• Quote the person when writing out
their goals.
• Collaborate and have the individual
sign the goals they have set.
• Have the person choose the
interventions they feel will work for
them.
Mental Health Commission of Canada,
Guidelines for Recovery-Oriented Practice
http://www.mentalhealthcommission.
ca/sites/default/files/2016-07/MHCC_
Recovery_Guidelines_2016_ENG.PDF
Informed
consent
For individuals with concurrent disorders,
their health information and/or treatment
plans are often shared with supporting
services, clinicians or agencies.
Obtaining informed consent means
• the clinician and person having a shared
discussion identifying what information
may or may not be shared with others
• allowing the person to ask questions and
make a decision about the sharing of
information
• documentation of the discussion and the
decision that was made about sharing
information and treatment
• Have the individual sign a consent
form outlining that they understand
that their treatment plan or other
information may be shared with other
programs.
• Include any specific instructions on
sharing information in the treatment
plan.

Integrated treatment planning
— 21 —
Enhancing concurrent capability: A toolkit
Element Description Tips and resources
Evidence-
informed
practice
Clinically relevant research and best practice
treatment approaches should be used to
help inform the treatment options that are
the most effective, safe and relevant.
Clinical expertise may also be required
to help guide the development of an
integrated treatment plan, bringing clinical
skills and past experience to identify and
treat each person’s unique state and
diagnosis.
• Tailor interventions to the motivational
level or stage the person is at.
• Stay up to date on best practice
guidelines and interventions for
specific concurrent disorder diagnoses.
Social
determinants
of health
Clinicians and frontline staff need to
understand the social determinants of
health
1
and health inequities
2
and how
they may affect a client’s treatment.
Ongoing support in basic life areas, such
as income and social status; social support
networks; education; employment/working
conditions; social environments; physical
environments; personal health practices and
coping skills; healthy child development;
gender; and culture helps clients
• maintain treatment successes
• ensure their basic life needs are being met
• prevent relapses
• Ask the individual about possible
barriers that might exist for them to
access treatment i.e. transportation,
availability of food, child care
• Consider that addressing basic life
needs prior to specific treatment
interventions may enable the client to
better respond to treatment.
• Addressing issues that may otherwise
impede successful recovery might
include helping the person to secure
stable housing, limiting access to
money for substance use or helping
a client achieve a goal to ‘get their
driver’s license back’ in order to
overcome transportation issues that
might prohibit them from attending
treatment services.
Motivation-
based
treatment
To treat concurrent disorders most
effectively, interventions should be related
to the person’s motivation for change.
A person’s motivation may change at
different stages of treatment for concurrent
disorders. An awareness of stage-matched
interventions helps guide the person in their
treatment options.
• Tailor interventions to the individual’s
motivational level and stage of change.
1
The conditions in which people are born, grow, live, work and age. These circumstances are shaped by the
distribution of money, power and resources at the global, national and local levels. The social determinants of
health are mostly responsible for health inequities (WHO, 2014).
2
Health inequities are the differences in the health of individuals that result largely from the social determinants
of health. They are socially produced (and therefore modifiable), systemic in their distribution across the population
and unfair (RNAO, 2015).

Integrated treatment planning
— 22 —
Enhancing concurrent capability: A toolkit
Cultural Safety and Cultural Competence
Element Description Tips and resources
Cultural
competency
and safety
Cultural competency shows a level of
demonstrated professional practice required
to provide effective clinical care to patients
from a particular ethnic or racial group. It
includes behaviours, attitudes, knowledge,
skills and policies that can come together
on a continuum to reflect the ability of a
system, agency, program or individual to
provide care to patients with diverse values,
beliefs and behaviours.
Cultural safety is about power relationships
in the health-care setting. It means setting
up systems that enable the less powerful
to monitor the attitudes and service of
the more powerful, to comment freely
and without repercussions and ultimately
to create useful and positive change that
benefits the health-care system and the
people we serve
(AHS, Aboriginal Health Team, 2015).
• You will never be completely aware of
another culture—so be safe with their
culture so that they can be safe with
yours.
• In the health-care environment, service
providers are considered to be the
more powerful person in the provider-
patient relationship. Recognizing this
dynamic is an important element of
cultural safety, especially for Aboriginal
people, who may perceive the hospital
or clinic as an intimidating setting.
For more information about cultural
competency and safety, see
Appendix 3.
>| suggested activity |<
Read the following case study and
discuss.
A 38-year-old Aboriginal woman
with a history of crystal meth use
is admitted to addiction services.
Within a few days she demands
to see her “Elder” and wants to
attend a sweat lodge ceremony
to be “cleansed.” You have
connections to the Aboriginal
community and can arrange a sweat
lodge ceremony in the future. How
would you work with this individual?
With your team? With the individual’s
family or community members?
What factors need to be considered
to ensure cultural safety and
competence?
Integrated treatment planning
— 23 —
Enhancing concurrent capability: A toolkit
Understanding stages of change and stages of treatment
Recognizing what stage a particular person is at can help you decide
which interventions are most likely to be successful at a particular
point in their treatment and recovery.
Two models can help with this:
• The Stages of Change Model, which describes the process of
behavioural change
• The Stages of Treatment Model, which describes the phases of
treatment
The Health of the Nation Outcome Scales (HoNOS) is another
instrument that can be used to help clinicians rate a problem’s
severity. The 12- to 15-item scale was designed for people with mental
illness, regardless of diagnosis, and has also been used with those
with addictions. It is intended to be easily incorporated into routine
clinical work, and to be used to track change over time in key areas of
client health and functioning.
Using the above models and scales can help understand where a
person is at in both their motivation to change and their treatment,
and can assist with integrated treatment planning.
See Appendix 4 for a chart outlining the Stages of Change and Stages
of Treatment Models.
See Appendix 5 for the HoNOS Adult tool from Addictions and Mental
Health, Alberta Health Services.

Integrated treatment planning
— 24 —
Enhancing concurrent capability: A toolkit
The steps to integrated treatment planning
Treatment planning involves combining and integrating information
obtained from the first steps of screening and comprehensive
assessment into a coherent set of actions with the person, their family
members and their treatment team.
The treatment planning process typically occurs at an interdisciplinary
case conference, which take place regularly within addiction and
mental health teams. These conferences use a collaborative and
person-centred approach with a focus on individual strengths and
recovery-oriented care.
Participants at case conferences can include
• physicians
• psychiatrists
• allied health professionals
• addiction counsellors
• nursing staff
• support staff
• peer support workers
• person seeking services
• family members/support system
• mental health clinicians/therapists
• community service providers
Example: Weekly case conference at a co-located addiction and
mental health outpatient clinic
1. The clinician who completed the intake tasks (screening and
assessment) with the person presents a description of them to the
interdisciplinary team (in person or virtually) for a case conference.
This presentation includes the person’s hopes, goals and reasons for
accessing services, as well as a list of prioritized and identified needs
through screening and assessment.
2. The team discusses best approaches and therapies to help the person
achieve their recovery goals.
3. The individual is invited into the case conference to hear the team’s

Integrated treatment planning
— 25 —
Enhancing concurrent capability: A toolkit
recommendations and to contribute their thoughts and actions that
support recovery.
4. After the case conference, a final treatment plan is written by a
clinician and co-signed by the person, who receives a copy.
5. At each conference afterward, the treatment plan is reviewed by the
team and the individual.
For a sample case conference presentation format template, see
Appendix 6.
The clinician’s role in treatment planning is
• to identify and prioritize the problem from information gathered
from screening and assessment, and present it at the case
conference
• to coach the person to identify their short- and long-term goals,
strengths and perceptions of the severity of each issue or need
• to support and empathize with the person when they encounter
challenges and barriers to achieving their goals
• to celebrate with the person as they take small steps in their
treatment plans
• to provide treatment options and interventions that will assist
them in meeting their recovery goals
• to review the treatment plan regularly at case conferences to
monitor progress and modify, as needed (in collaboration with
the person and their family)
In addition, it is your responsibility to
ensure that treatment and interventions
are delivered to the person in a way that is
coordinated and collaborative. Treatment
options depend on the services available
and the appropriate treatment required.
Mueser et al (2003) suggests that
addressing the areas in which
the disorders interact has the
most promise for improving the
outcomes of both disorders.

Integrated treatment planning
— 26 —
Enhancing concurrent capability: A toolkit
Key messages
Integrated treatment plans may involve interventions that directly or
indirectly address the concurrent disorders.
Treatment needs to be delivered in a way that is coordinated and
collaborative. This can often be managed through effective case
management, which will be discussed in an upcoming chapter.
Treatment approaches will vary in content, length and degree of ongoing
support, depending on the person’s needs and motivation level.
A person may exhibit symptoms that may be perceived as cultural, and
that may require further exploration.
“Effective [concurrent disorder] programs combine mental health and
substance abuse and addictions interventions that are tailored for the
complex needs of clients” (Substance Abuse and Mental Health Services
Administration, 2009).
The implementation of a treatment plan should be regularly reviewed,
revised and updated as necessary, with the individual celebrating small
steps toward their goals.
For more detailed steps in planning, see the treatment planning checklist
developed by the Addiction Technology Transfer Centre Network:
http://www.nattc.org/aboutUs/blendingInitiative/matrs/CHECKLISTMATRS.pdf
“Focusing on inherent and diverse strengths and abilities of each
person, rather than deficits or limitations, motivates people to feel
good about themselves and builds confidence and resilience while
helping people take action towards achieving their goals” (Mental
Health Commission of Canada, 2015)
Setting SMART goals
How do we develop goals and objectives that meet a person’s
motivation for recovery? One way is by developing SMART goals as
part of an integrated treatment plan (Addiction Messenger, 2006 and
Meyer, 2003).

Integrated treatment planning
— 27 —
Enhancing concurrent capability: A toolkit
Smart Goals
Smart goals are: Description Answers questions
S – Specific
• Make objectives and interventions that are
specific and goal-focused to allow you and the
individual to note progress.
• Target specific behaviours that can help
the person reduce symptoms and improve
functioning.
What?
Why?
Who?
Where?
Which?
M – Measurable
• Measuring progress helps you, the individual
and other staff members stay on track, reach
target dates and experience the achievement
of continued effort that is required to reach the
ultimate goal.
• Allows you and the individual to document
change.
• Provides a means of holding you, the individual
and other staff members accountable.
How much?
How many?
How will we know the
goal is accomplished?
A - Attainable
• Goals, objectives and interventions are
achievable during treatment.
• Focus on “improved functioning” rather than
the “end” of the individual’s problem.
• Identify those goals that can be attained given
the level of care provided, the individual’s
motivation and services and support available.
• Revise objectives and interventions as needed
when the individual moves from one level of
care to another.
How can the goal be
accomplished?
How realistic is the goal?
R – Relevant
• Objectives are realistic and practical.
• Goals and objectives are achievable, given
the individual’s environment, support system,
diagnosis and level of functioning.
• There is a good understanding of the steps the
person can take on their own behalf to achieve
their goals.
Does this seem
worthwhile?
Is this the right time?
Are the right people
involved to support the
goal?
T – Time-limited
• Sets a target date on the goals and objectives.
• Ensures review and evaluation of progress
towards the goals, objectives and interventions
and allows for modifications to be made in a
timely manner.
At what point will the
goals be achieved (e.g.,
today, six months from
now)?

Integrated treatment planning
— 28 —
Enhancing concurrent capability: A toolkit
>| exercise |<
Writing SMART goals
Working with a partner, or on your own, read the case study provided and write two or three
SMART goals as if you were working in collaboration with the person involved.
Remember, SMART goals are:
S – Specific
M – Measurable
A – Attainable
R – Relevant
T – Time-limited
Case study:
Jody is a married, 40-year-old woman who was recently admitted to your program. Jody says she would
like help reducing her alcohol intake and to have a better relationship with her children and husband.
Jody is currently prescribed Cymbalta (30 mg daily) by her family physician for anxiety, which she has
been taking for the last year. She smokes one half of a pack of cigarettes daily and takes medication for
hypertension.
Jody reported feeling fearful, nervous, irritable and stressed, with problems sleeping.
Jody disclosed drinking a bottle of wine daily since going on long-term disability one year ago.
She has been admitted to detox on two prior occasions; the last time was one year ago. Jody
acknowledged that she did not complete treatment, nor did she follow through with recommendations
that included counselling through Adult Addiction Services.
Jody disclosed having thoughts of suicide a year ago before she was last admitted to detox, when she
thought about taking an overdose of the Cymbalta she had just started in combination with alcohol.
Jody has never attempted suicide and reports no history of self-harm behaviour. Her husband is
threatening to leave her and take the children.
SMART goal #1
_____________________________________________________________________________________________
_____________________________________________________________________________________________
SMART goal #2
_____________________________________________________________________________________________
_____________________________________________________________________________________________
SMART goal #3
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Integrated treatment planning
— 29 —
Enhancing concurrent capability: A toolkit
>| exercise |<
Reflecting on your current treatment planning process
Reflecting on your current treatment planning process, how do you treatment plan now?
List the steps you usually take after screening and assessment with the person below
(e.g., case conferences, written treatment plan).
1. ___________________________________________________________________________________
2. ___________________________________________________________________________________
3. ___________________________________________________________________________________
4. ___________________________________________________________________________________
Reflecting on the integrated treatment planning components (see below), how could you
modify your process to be more concurrent capable?
1. ___________________________________________________________________________________
2. ___________________________________________________________________________________
3. ___________________________________________________________________________________
4. ___________________________________________________________________________________
Components of integrated treatment planning:
3 Person-centred
3 Recovery focused
3 Trauma informed
3 Informed consent
3 Social determinants of health
3 Evidence informed
3 Motivation-based treatment
Challenges to integrated treatment planning
Spend a few moments, either alone or with a colleague, thinking about challenges you have
faced in your work related to integrated treatment planning.
For each challenge, identify strategies that might help reduce or eliminate it.
Challenge Strategy

Integrated treatment planning
— 30 —
Enhancing concurrent capability: A toolkit
Successful integrated treatment planning
Historically, persons with concurrent disorders were treated in parallel
treatment systems for substance use and mental health. Remnants
of these systems remain today and can sometimes pose barriers to
treatment if systems are not integrated or services do not interact.
Key messages
Ensuring the following can help make for successful integrated
treatment planning:
Clinicians and clinical services recognize the need for collaborative
treatment approaches and help coordinating this for the individual in a
seamless manner.
Trained professionals have a common understanding of concurrent
disorders and understand the role of other professionals in the field with
whom they might collaborate.
Working with the individual to set recovery-focused goals, even if they
are unwilling to address the concurrent disorder (they may be willing to
focus on one component to start).
Ensuring the individual is at the centre of the decision-making for
developing the plan.
Working with the individual to identify and develop a plan with SMART
goals.
The vulnerable population of individuals with concurrent disorders often
requires addressing socio-economic issues (e.g., poverty, homelessness,
unemployment) to ensure successful outcomes.
Including peer support workers and/or family members in treatment
planning.
Sustaining the individual’s participation in the ongoing treatment.
Continuity of treatment across various services.
Working with the individual to evaluate the treatment plan and change
intervention options or address other needs that might lead to poor
treatment adherence.

Integrated treatment planning
— 31 —
Enhancing concurrent capability: A toolkit
It’s not just the plan—it’s you!
A key component of creating an integrated treatment plan is realizing
that it is not just the plan itself. Rather, it is also the engagement
and collaboration amongst and between clinicians, clinical teams,
individuals and their families.
In an effort to create successful and seamless integrated treatment
planning, remember the following key components:
• Accessible consultation, education and teaching opportunities for
frontline staff to manage a wide variety of concurrent disorders.
• Improved collaboration and access between services to ensure
that the person is receiving the best care.
• Developing partnerships with other clinicians and clinical
programs, community organizations and other agencies or
programs that may enhance support and treatment (e.g., family
advocacy groups, police, shelters, food banks, social service,
criminal justice system).
• Supporting the person in navigating these systems and advising
them of available options. To do this, you yourself need to
establish relationships with other people, areas and services to
ensure you can provide the best options to the individual.
• Knowing when to keep and consult, and when to provide a warm
handoff to more appropriate services to ensure continuity of care.

Integrated treatment planning
— 32 —
Enhancing concurrent capability: A toolkit
>| exercise |<
Collaboration Opportunities
Take a few moments to identify programs, services, agencies or people that it would be
beneficial to collaborate with for integrated treatment planning.
First, list the networks, programs, services, agencies or people with which you already connect.
_____________________________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Now list the networks, programs, services, agencies or people with which you know exist but
with which you have not yet connected.
_____________________________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
How could you connect with these areas?
_____________________________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Commit to re-connecting with one or two community partnersselections you already have
an established relationship with, and reach out to one or two that you have yet to build a
relationship with, but that you feel would help you better accomplish integrated treatment
planning.

Integrated treatment planning
— 33 —
Enhancing concurrent capability: A toolkit
Conclusion
We hope you have found this chapter to be helpful. If you have any
questions, comments or stories to share, please contact
concurrent.disor[email protected].
Want more information on integrated treatment for concurrent disorders?
Check out the Substance Abuse and Mental Health Services Administration’s Integrated
Treatment for Co-Occurring Disorders, which has compiled a list of evidence-based
resources on topics such as the historical context of integrated treatment for concurrent
disorders, implementation and administrative issues, financing and cost-effectiveness,
engagement, system-level integration and evidence on specific treatment approaches,
and more:
http://store.samhsa.gov/product/Integrated-Treatment-for-Co-Occurring-Disorders-
Evidence-Based-Practices-EBP-KIT/SMA08-4367.

— 34 —
Integrated treatment planning | APPENDIX 1
Enhancing concurrent capability: A toolkit
APPENDIX 1
Examples of integrated treatment models
The Integrated Dual Disorder Treatment (IDDT) model
Integrated Dual Disorder Treatment (IDDT) evidence-informed
practice was developed by Robert E. (Bob) Drake MD, PhD; Kim T.
Mueser, PhD; and their colleagues, and is studied by researchers at the
Dartmouth Psychiatric Research Center of Dartmouth Medical School
in Lebanon, New Hampshire.
Mueser, Noordsy, Drake and Fox (2003) suggest that effective
treatment for concurrent disorders is based on shared decision-making
and consists of the following components:
• Integration of services – the same clinician or program provides
treatment for concurrent disorders to the individual (or seamlessly
coordinates all treatment for the individual)
• Comprehensiveness – acknowledges that reducing or eliminating
substance abuse is a major goal of integrated treatment, but that
achieving this usually involves more than changing behaviours
directly linked to the use, and may involve addressing social and
economic factors in the individual’s life i.e. employment, social
skills training.
• Assertiveness – clinicians must actively engage with the
individual in the process of treatment even if the individual is
unmotivated. This may requires assertive outreach i.e. meeting at
the individual’s home, developing trust
• Reduction of negative consequences – this refers to reducing
the negative consequences of substance abuse that may impair
insight into treatment or lack of motivation to seek treatment.
• Long-term perspective (time-unlimited) – recognizing that
adopting healthier lifestyles and changing habits that support
recovery can take months or even years.
• Motivation-based treatment – interventions should be adapted
to the individual’s motivation for change for most effective
treatment.

— 35 —
Integrated treatment planning | APPENDIX 1
Enhancing concurrent capability: A toolkit
• Multiple psychotherapeutic modalities – using an array of
different treatment approaches typically optimizes individual
outcomes.
The IDDT evidence-based practice involves cross-trained practitioners
providing integrated comprehensive services directed toward
individuals with concurrent disorders simultaneously in the same
venue, with the goal of recovery from both illnesses.
More information can be found in Mueser, K.T., Noordsy, D.L., Drake,
R.E., Fox, L. (2003). Integrated treatment for dual disorders a guide to
effective practice. New York, NY: The Guilford Press.
The Integrated Placement and Support model
Resources providing more detailed information on this model include
the following:
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4079136/
https://waamh.org.au/development-and-training/individual-placement--support-
ips.aspx

— 36 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 2
APPENDIX 2
Sample plan templates
SAMPLE: Treatment Plan Template
DATE PATIENT’S GOALS ACTION
To be taken and by whom
TARGET OUTCOMES TARGET
DATE
CLINICIAN
Name/Discipline
Goal:
Stage of change:
Goal:
Stage of change:
Goal:
Stage of change:
Patient signed
o Copy given to patient o Copy sent to community upon discharge
PATIENT PROGRESS
Achieved targets and successes Staff signature/Date
My name is: My support people are:
My hopes/goals are… My strengths are… My needs are…

— 37 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 2
SAMPLE: Recovery Plan Template
PROGRAM Date: 2013
PERSON: Client Team Members
Strength based discussion: Describe recent or relevant
periods of success:
Person’s goals for a happy Life
GOALS AND OBJECTIVES: WHAT DO WE DO?
(Stage matched
interventions)
RESPONSIBLE
PERSONS (Who
does what?)
Milestones of
progress and
opportunities for
rounds of applause
1. Issue:
Stage:
Goal
Objectives
2. Issue:
Stage:
Goal
Objectives
3. Issue:
Stage:
Goal
Objectives
4. Issue:
Stage:
Goal
Objectives
SIGNED BY: Client ( ) Family ( ) Program Manager ( ) Staff ( ) Staff ( ) MD ( ) Other ( )

— 38 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 3
APPENDIX 3
Cultural safety and cultural competency resources
AHS Aboriginal Sensitivity E Learning Course on AHS My Learning Link
Cultural Competency and Safety: A Guide for Health Care
Administrators, Providers and Educators
http://www.naho.ca/documents/naho/publications/culturalCompetency.pdf
Indigenous Cultural Competency Training Program
http://www.culturalcompetency.ca/training/indigenous
Colour Coded Health Care, The Impact of Race and Racism on
Canadians Health
http://www.wellesleyinstitute.com/wp-content/uploads/2012/02/Colour-
Coded-Health-Care-Sheryl-Nestel.pdf
Cross TL, Barzon BJ, Dennis KW, and Isaacs MR. (1989). Towards
a Culturally Competent System of Care: A Monograph on Effective
Services for Minority Children Who are Severely Emotionally
Disturbed. Washington, DC: CASSP Technical Assistance Center,
Georgetown University Child Development Center.

— 39 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 4
APPENDIX 4
Understanding stages of change and stages
of treatment
The following chart outlines both models along with clinical
intervention examples for each stage (Provincial Concurrent Capable
Learning Series (PCCLS), Alberta Health Services):

— 40 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 5
APPENDIX 5
HONOS – Addiction and Mental Health, AHS

— 41 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | APPENDIX 6
APPENDIX 6
Sample case conference presentation format
(Used with permission: K. Minkoff, personal communication,
November 27, 2015)

— 42 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | REFERENCES
References
AADAC. (2007). Concurrent disorders treatment approaches: literature review. AADAC.
Addiction and Mental Health Collaborative Project Steering Committee. (2014). Collaboration for addiction and
mental health care: Best advice. Ottawa, ON: Canadian Centre on Substance Abuse. Retrieved at http://www.
ccsa.ca/Resource%20Library/CCSA-Collaboration-Addiction-Mental-Health-Best-Advice-Report-2014-en.pdf
Addiction and Mental Health, ECC Components Sub-Group. (June 2011). Enhancing Concurrent Capability
Across Addiction and Mental Health Services - Foundational Concepts. Alberta Health Services.
Retrieved at https://my.albertahealthservices.ca/http://insite.albertahealthservices.ca/amh/tms-amh-ecc-
foundational-concepts.pdf
Addiction Messenger. (June 2006). Treatment Planning – Part 2 Making it a SMART Plan. Vol 9, Iss 5. Addiction
NorthwestFrontier/Vol.%209%20Issue%205.pdf
Addiction Messenger. (June 2006). Treatment Planning – Part 3 Putting it All Together. Vol 9, Iss 6. Addiction
NorthwestFrontier/Vol.%209%20Issue%206.pdf
Alberta Health Services. (2015). Patient First Strategy. http://www.albertahealthservices.ca/assets/info/pf/
American Society of Addiction Medicine (ASAM) (2015). http://www.asam.org/publications/the-asam-criteria/
about/
Biegel, D. E., Kola, L. A., Ronis, R. J., & Kruszynski, R. (2013). Evidence-based treatment for adults with co-
occurring mental and substance use disorders: Current practice and future directions. Community Mental
Health: Challenges for the 21st Century (2nd Ed.). New York, NY, US: Routledge/Taylor & Francis Group.
Brousselle, A., Lamothe, L., Sylvain, C., Foro, A., & Perreault, M. (2010). Integrating services for patients with
mental and substance use disorders: What matters?. Health Care Management Review, 35(3), 212–223.
Addiction and Mental Health Collaborative Project Steering Committee. (2014). Collaboration for addiction
and mental health care: Best advice [PDF File] Ottawa, ON: Canadian Centre on Substance Abuse. Retrieved
from http://www.ccsa.ca
Canadian Centre on Substance Abuse (CCSA). (2009). Concurrent disorders substance abuse in Canada.
Ottawa, ON. Canadian Centre on Substance Abuse. – Vaccarion, F.J. chapter 7 p58-63 A call to action http://
www.ccsa.ca/Resource%20Library/ccsa-011811-2010.pdf
Canadian Centre on Substance Abuse (CCSA). (Apr 2010). Substance abuse in Canada: concurrent disorders
- highlights. Ottawa, ON. Author. Retrieved from: http://www.ccsa.ca/Resource%20Library/CCSA-Systems-
Approach-System-Mapping-Tools-2014-en.pdf
Carlson, L., Rapp, C. A., & Eichler, M. S. (2012). The expert’s rate: supervisory behaviors that impact the
implementation of evidence-based practices. Community Mental Health Journal, 48(2), 179–186.
Centre for Addiction and Mental Health. Concurrent substance use and mental health disorders information
guide. Accessed March 29, 2015 from: http://www.camh.ca/en/hospital/health_information/a_z_mental_
health_and_addiction_information/concurrent_disorders/concurrent_substance_use_and_mental_health_
disorders_information_guide/Pages/how_cd_treated_infoguide.aspx
Centre for Addiction and Mental Health. A family guide to concurrent disorders. Accessed March 29, 2015
from: http://www.camh.ca/en/hospital/health_information/a_z_mental_health_and_addiction_information/
concurrent_disorders/a_family_guide_to_concurrent_disorders/treatment/Pages/treatment.aspx
Center for Substance Abuse Treatment. (2006). Screening, Assessment, and Treatment Planning for Persons
With Co-Occurring Disorders. COCE Overview Paper 2. DHHS Publication No. (SMA) 06-4164. Rockville,
MD: Substance Abuse and Mental Health Services Administration, and Center for Mental Health Services.
Retrieved from: http://store.samhsa.gov/shin/content//PHD1131/PHD1131.pdf
Centre for Addiction and Mental Health. (2005). Treating concurrent disorders a guide for counsellors.
Skinner, W.J.W. (Ed.). Canada.
Connecticut Department of Mental Health and Addiction Services. (February 2009). Competencies for
Providing Services to Individuals with Co-Occurring Mental Health and Substance Use Disorders.
Author. Retrieved from http://www.ct.gov/dmhas/lib/dmhas/cosig/CODcompetencies.pdf
Department of Mental Health and Addiction Services. Guide to Creating Your Program’s Implementation Plan
to Increase Co-Occurring Capability. Co-Occurring Disorders Initiative Integrated Treatment Tools. State of
Connecticut. Retrieved from: http://www.ct.gov/dmhas/lib/dmhas/cosig/implementationplanguide.pdf
Department of Mental Health and Addiction Services. (Feb 2009). Competencies for providing services to
individuals with co-occurring mental health and substance abuse disorders. Co-Occurring Disorders
Initiative Integrated Treatment Tools. State of Connecticut. Retrieved from: http://www.ct.gov/dmhas/lib/
dmhas/cosig/implementationplanguide.pdf
Drake, R. E., & Bond, G. R. (2010). Implementing integrated mental health and substance abuse services. Journal
of Dual Diagnosis, 6(3/4), 251–262.
Hamilton, I. (2010). Ensuring integrated treatment for people with mental health and substance use problems.
Nursing Times, 106(11), 12–5.
Health Canada. (2001). Best practices concurrent mental health and substance use disorders. Ottawa, ON.
— 43 —
Enhancing concurrent capability: A toolkit
Integrated treatment planning | REFERENCES
Healthy Public Policy, Health Promotion, Disease and Injury Prevention, Alberta Health Services (2011). Social
environments and health concept paper. Edmonton. http://www.albertahealthservices.ca/poph/hi-poph-
hpp-healthy-public-policy-concept-paper.pdf
Kodner, DL. (October 2012). Integrated health care: The what, why, how and how not. Paper presented at
the Health Council of Canada National Symposium on Integrated Health Care, Toronto. Retrieved from http://
healthcouncilcanada.ca/tree/symposium2012/P1_IntegratedHealthCare_Kodner_EN.pdf
Kola, L. A., & Kruszynski, R. (2010). Adapting the integrated dual-disorder treatment model for addiction
services. Alcoholism Treatment Quarterly. Kola, Lenore A.: Mandel School of Applied Social Sciences, Case
Western Reserve University, 10900 Euclid Avenue, Cleveland, OH, US, 44106, lenor[email protected]: Taylor &
Francis.
Mancini, M. A., & Miner, C. S. (2013). Learning and change in a community mental health setting. Journal of
Evidence-Based Social Work, 10(5), 494–504.
Meyer, PJ. (2003). ‘What would you do if you knew you couldn’t fail? Creating S.M.A.R.T. Goals.’ Attitude is
everything: if you want to succeed above and beyond. Meyer Resource Group, Incorporated, The. ISBN
978-0-89811-304-4.
Mental Health Commission of Canada. (2015). Recovery Guidelines Ottawa, ON: Author. ©2015 Mental Health
Commission of Canada http://www.mentalhealthcommission.ca/English/initiatives/RecoveryGuidelines
Miller, W.R., Forchehimes, A.A., Zweben, A. (2011) Treating addiction: a guide for professionals. The Guilford
Press. New York, NY. Chapter 18 pp281-300.
Mueser, K.T., Noordsy, D.L., Drake, R.E., Fox, L. (2003). Integrated treatment for dual disorders a guide to
effective practice. New York, NY: The Guilford Press.
NFATTC Addiction Messenger. (April/May 2006) Treatment Planning - Part 2 Make It a S.M.A.R.T. Plan.
Northwest Frontier Addiction Technology Transfer Center. Vol 9 Iss 5. Retrieved from http://www.
NFATTC Addiction Messenger. (June 2006) Treatment Planning - Part 3 Putting it all together. Northwest
Frontier Addiction Technology Transfer Center. Vol 9 Iss 6. Retrieved from http://www.attcnetwork.org/
Novotna, G. (2014). Competing institutional logics in the development and implementation of integrated
treatment for concurrent disorders in Ontario: A case study. Journal of Social Work. Novotna, Gabriela:
Faculty of Health Sciences, University of Lethbridge, 4401 University Drive, Lethbridge, AB, Canada, T1K 3M4,
gabriela.nov[email protected]: Sage Publications.
Novotna, G. (2013). Institutionalizing integrated treatment for concurrent disorders: creating new
organizational discourse. Health Care Management Review, 38(1), 51–60.
Rafferty, M. S., & Drake, R. E. (2013). Integrated treatment for people with co-occurring mental illness and
substance use disorders. (D. Barrowclough Drake, Drake, Drake, Drake, Fox, McHugo,
McHugo, O’Connor, Regier, Ridgely, Ed.) Best Practices in Community Mental Health: A Pocket Guide.
Chicago, IL, US: Lyceum Books.
Registered Nurses’ Association of Ontario. (2015). Engaging Clients Who Use Substances. Toronto, ON:
Substances_13_WEB.pdf
Roberts, B. (2012). Interprofessional relationships in dual diagnosis discourse in an Australian state: Are
we respecting each other yet? Mental Health and Substance Use. Roberts, Bridget: Department of Rural
and Indigenous Health, School of Rural Health, Faculty of Medicine, Nursing and Health Sciences, Monash
University, PO Box 973, Moe, VIC, Australia, 3825, [email protected]: Taylor & Francis.
Rush, B., Fogg, B., Nadeau, L., Furlong, A. (Dec 2008). On the integration of mental health and substance
abuse services and systems: summary report. Canadian Executive Council on Addictions. Retrieved from:
http://www.ceca-cect.ca/pdf/Summary-reportFINAL-Dec18-08.pdf
Substance Abuse and Mental Health Services Administration. (2009). Integrated Treatment for Co-Occurring
Disorders: Building Your Program. DHHS Pub. No. SMA-08-4366, Rockville, MD: Center for Mental Health
Services, Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human
Services. Retrieved from: https://store.samhsa.gov/shin/content/SMA08-4367/BuildingYourProgram-ITC.
pdf
Substance Abuse and Mental Health Services Administration. (2009). Integrated treatment for co-occurring
disorders: How to use the evidence-based practices KITs. DHHS Pub. No. SMA-08-4366, Rockville, MD:
Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, U.S.
Department of Health and Human Services.
Substance Abuse and Mental Health Services Administration. (2009). Integrated treatment for co-occurring
disorders: The Evidence. DHHS Pub. No. SMA-08-4366, Rockville, MD: Center for Mental Health Services,
Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.
