
Stanford School of Medicine
Master of Science in Physician Assistant Studies
MSPA Studies Program Handbook and Policy Manual
Academic Year 2023-2024
2
TABLE OF CONTENTS
1.0. INTRODUCTION ............................................................................................................... 4
2.0. GENERAL STANDARDS ..................................................................................................... 5
2.1. PHYSICIAN ASSISTANT PROGRAM COMPETENCIES ................................................................... 5
2.2. SPECIFICATION OF REQUIREMENTS FOR GRADUATION ............................................................. 7
2.3. SCHOOL OF MEDICINE TECHNICAL, NON-ACADEMIC STANDARDS ............................................. 8
2.4. SCHOOL OF MEDICINE PROFESSIONALISM PRINCIPLES FOR PA STUDENTS .............................. 11
2.5 TEACHER-LEARNER AGREEMENT ............................................................................................. 15
3.0. MSPA STUDIES PROGRAM REQUIREMENTS AND PROCEDURES ...................................... 17
3.1. ACADEMIC RECORDS AND PRIVACY OF STUDENT RECORD INFORMATION .............................. 17
3.2 REGISTRATION AND STUDY LISTS ............................................................................................ 21
3.3. DATA SECURITY AND PRIVACY (HIPAA) .................................................................................. 22
3.4. PA STUDENT PRACTICE ROLE.................................................................................................. 23
3.5. STUDENT RESOURCES: ACCOMMODATIONS AND SUPPORT .................................................... 25
3.6. ETHICAL CONDUCT OF BIOMEDICAL RESEARCH ...................................................................... 26
3.7. EVALUATION COMPLETION REQUIREMENTS .......................................................................... 27
3.8. INDUSTRY INTERACTIONS POLICY .......................................................................................... 29
3.9. LEAVES OF ABSENCE AND DISCONTINUATION AND REINSTATEMENT ...................................... 30
3.10. MALPRACTICE LIABILITY FOR MSPA PROGRAM STUDENTS .................................................... 34
3.11. MEDICAL HEALTH REQUIREMENTS AND IMMUNIZATIONS .................................................... 35
3.12. POLICIES AND RESOURCES FOR DEVICE ENCRYPTION, SECURITY AND USE ............................. 37
3.13. RESPECTFUL ENVIRONMENT AND MISTREATMENT POLICY ................................................... 40
3.14. SAFETY TRAINING ................................................................................................................ 45
3.15. STANFORD MEDICINE POLICY FOR THE REMOVAL AND TRANSPORT OF PHI .......................... 46
3.16. STANFORD SCHOOL OF MEDICINE EDUCATION RESEARCH POLICY ........................................ 50
3.17. STUDENT PARTICIPATION IN CLINICAL ACTIVITIES INVOLVING PERSONAL RISK ..................... 50
3.18. SURGICAL PROCEDURES FOR MSPA STUDENTS ..................................................................... 51
3.19. UNIVERSAL PRECAUTIONS AND NEEDLESTICK PROTOCOL ..................................................... 52
3.20. STANFORD HEALTH CARE/LUCILE PACKARD CHILDREN’S HOSPITAL STANFORD
COMPUTER ACCESS FOR PA STUDENTS (EPIC)......................................................................... 54
3.21. SCHOOL OF MEDICINE LEARNING SPACES ............................................................................. 56
3.22. ABSENCE POLICY AND EXPECTATIONS .................................................................................. 57
3.23. N95 RESPIRATOR MASK FIT REQUIREMENTS FOR PA STUDENTS ........................................... 59
3.24. SCHOOL OF MEDICINE DRESS CODE GUIDELINES FOR THE CLINICAL SETTING ........................ 61
3.24. SCHOOL OF MEDICINE CRIMINAL BACKGROUND CHECK POLICY ............................................ 62
3.25. MSPA PROGRAM POLICY ON VOLUNTEERING AND WORKING FOR THE PROGRAM ............... 62
4.0. CURRICULUM ................................................................................................................ 63
4.1 CURRICULUM OVERVIEW........................................................................................................ 63
4.2. ACADEMIC CALENDAR ........................................................................................................... 64
4.3. ACADEMIC REQUIREMENTS FOR GRADUATION ...................................................................... 68
4.4. LEADERSHIP TRACK AND THESIS PROJECT REQUIREMENT ....................................................... 69
4.5. REQUIRED PRE-CLERKSHIP COURSES ...................................................................................... 70
4.6. CALENDAR OF CLERKSHIP PERIODS ........................................................................................ 76
4.7. CLERKSHIP REQUIREMENTS ................................................................................................... 77
4.8. ELECTIVE CLERKSHIPS ............................................................................................................ 77
4.9. ABSENCES DURING CLERKSHIPS ............................................................................................. 78
3
4.10. CLINICAL PERFORMANCE EXAMS ......................................................................................... 79
5.0. ASSESSMENT OF STUDENT ACADEMIC PERFORMANCE .................................................. 80
5.1. HEALTH PROVIDER INVOLVEMENT IN STUDENT ASSESSMENT ................................................ 80
5.2. EVALUATION OF PERFORMANCE IN COURSES ........................................................................ 80
5.3. EXAM POLICY FOR REQUIRED PRE-CLERKSHIP COURSES ......................................................... 86
5.4. EVALUATION OF PERFORMANCE IN CLINICAL CLERKSHIPS ...................................................... 87
5.5. STANDARDIZED PATIENT TEACHING AND ASSESSMENT .......................................................... 88
6.0. STUDENT PROGRESS COMMITTEE (SPC) ......................................................................... 89
6.1. INTRODUCTION ..................................................................................................................... 89
6.2. STANDARDS FOR PERFORMANCE AND SATISFACTORY PROGRESS........................................... 94
6.3. PROMOTION ......................................................................................................................... 96
6.4. PROCEDURES FOR ADDRESSING PERFORMANCE, PROFESSIONAL AND TECHNICAL
STANDARDS CONCERNS ......................................................................................................... 97
6.5. APPENDIX: CHART OF STUDENT PROGRESS COMMITTEE
RESPONSES TO STUDENT ISSUES ..... 102
7.0. TUITION AND FINANCIAL AID ...................................................................................... 106
7.1. TUITION STRUCTURE AND BUDGET ...................................................................................... 106
7.2. ADDITIONAL FEES ................................................................................................................ 107
7.3. UNIVERSITY BILLING ............................................................................................................ 109
8.0. STANFORD UNIVERSITY POLICIES ................................................................................ 110
8.1. NONDISCRIMINATION POLICY ............................................................................................. 110
8.2. COMMUNITY STANDARDS .................................................................................................. 110
8.3. SEXUAL MISCONDUCT AND SEXUAL ASSAULT ...................................................................... 110
8.4. SEXUAL HARASSMENT AND CONSENSUAL SEXUAL OR ROMANTIC RELATIONSHIPS .............. 110
8.5. STUDENT ACADEMIC AND NON-ACADEMIC GRIEVANCE PROCEDURE ................................... 110
8.6. CHILDBIRTH ACCOMMODATION POLICY .............................................................................. 110
8.7. PREGNANCY, CHILDBIRTH, ADOPTION, AND LACTATION: POLICY ......................................... 110
8.8. STANFORD NAME AND TRADEMARKS ................................................................................. 110
8.9. COMPUTER AND NETWORK USAGE POLICY ......................................................................... 110
8.10. COPYRIGHT....................................................................................................................... 110
8.11. SMOKE-FREE ENVIRONMENT ............................................................................................ 110
8.12. CAMPUS SAFETY AND CRIMINAL STATISTICS ..................................................................... 110
8.13. TITLE IX OF THE EDUCATION AMENDMENTS OF 1972 ......................................................... 110
8.14. TITLE VI OF THE CIVIL RIGHTS ACT OF 1964 ........................................................................ 110
8.15. STUDENT ALCOHOL AND OTHER DRUGS POLICY ................................................................ 110
8.16. PROHIBITION OF THE POSSESSION OF DANGEROUS WEAPONS ON CAMPUS ...................... 110
8.17. GENERATIVE AI POLICY GUIDANCE .................................................................................... 110

4
1.0. INTRODUCTION
The following is the Master of Science in Physician Assistant Studies Program Handbook and
Policy Manual for 2023-2024 academic year. Students participating in the Stanford University
School of Medicine Master of Science in Physician Assistant (MSPA) Studies program are subject
to, and are responsible for being aware of, the policies and standards established by the MSPA
program, the School of Medicine, and by Stanford University; many of the Stanford University
policies are found in the Stanford Bulletin (https://bulletin.stanford.edu).
The MSPA program, Stanford University, and the School of Medicine reserve the right to make
changes in the applicable regulations, procedures, policies, requirements, and other
information contained in this handbook. Changes and revisions may occur throughout the
academic year.

5
2.0. GENERAL STANDARDS
2.1. PHYSICIAN ASSISTANT PROGRAM COMPETENCIES
The following are the Stanford School of Medicine, Master of Science in PA Studies program’s
competencies. These competencies were developed based on the framework of the program’s
mission and goals along with awareness of the Physician Assistant Education Association
(PAEA)’s Core Competencies for New PA Graduates and the Physician Assistant Competencies
which were written collaboratively by the American Academy of Physician Assistants (AAPA),
the Physician Assistant Education Association (PAEA), and The National Commission on
Certification of the Physician Assistant (NCCPA), and the Accreditation Review Commission on
Education of the Physician Assistant (ARC-PA.)
The Stanford School of Medicine Master of Science in PA Studies program uses achievement of
the following competencies as a guide for curriculum development and evaluation of the
success of the program and its graduates. Upon completion of the Stanford School of Medicine
Master of Science in PA Studies program, graduates are expected to achieve the following
competencies:
1. Medical Knowledge and Clinical Skills
a. Recognize the difference between normal and abnormal health states across all
organ systems.
b. Discern among acute, chronic, and emergent disease states.
c. Demonstrate knowledge of the anatomy, disease etiology, pathophysiology, clinical
manifestations, differential diagnoses, management, and appropriate interventions
for general medical and surgical conditions.
d. Demonstrate ability to obtain a medical history and perform a physical examination.
e. Demonstrate ability to conduct a virtual encounter.
f. Perform basic primary care diagnostic and therapeutic procedures.
g. Order appropriate diagnostic laboratory and radiographic tests and provide or obtain
accurate interpretations.
h. Develop differential diagnosis and treatment plans that include pharmacologic and
non-pharmacologic interventions.
i. Implement appropriate strategies for disease prevention and health care
maintenance.
j. Utilize evidence-based medicine to guide clinical decision-making.
k. Demonstrate ability to provide appropriate patient education.
2. Interpersonal and Communication Skills
a. Recognize the cultural norms, needs, influences, and socioeconomic, environmental,
and other population-level determinants affecting the health of the individual and
community being served.

6
b. Provide medical care that is respectful, ethical, considerate, empathetic, and
equitable.
c. Demonstrate the ability to provide effective verbal and nonverbal communication
with patients.
d. Review medical records, complete written documentation, and communicate
diagnostic findings and management strategies in a timely manner.
3. Health Care Finance
a. Demonstrate understanding of the basics of coding and billing.
b. Understand different types of health systems and insurance types.
c. Recognize the financial implications of clinical decision making and treatment plans.
4. Professionalism and Leadership
a. Demonstrate understanding of professional responsibilities around licensure,
credentialing, reimbursement, advocacy, and laws, policies, and regulations
regarding medical practice.
b. Demonstrate understanding of emotional intelligence and communication skills that
establish a personal leadership style.
c. Demonstrate understanding of the ability to shift leadership style to meet specific
professional challenges.
d. Demonstrate strong reading, writing and analytic skills.
e. Demonstrate professionalism, integrity, honesty, and respect for patient privacy and
confidentiality.
f. Understand the risk factors for burnout and the importance of one’s own health and
well-being.
7
2.2. SPECIFICATION OF REQUIREMENTS FOR GRADUATION
Graduation
The requirements for the MS degree in PA Studies are established by the Stanford University
Committee on Graduate Studies and allow no exceptions. Those requirements are as follows:
1. Satisfaction of Academic Requirements: To graduate, students must satisfy all academic
requirements.
2. Satisfaction of Professionalism Requirements: To graduate, students must meet the
standards of professionalism set forth in the School of Medicine Professionalism
Principles for PA Students in the MSPA Studies Program Handbook and Policy Manual,
Section 2.4.).
3. Satisfaction of Technical Standards: To graduate, students must meet the requirements
set forth in the School of Medicine Technical, Non-Academic Standards (MSPA Studies
Program Handbook and Policy Manual, Section 2.3.).
4. Satisfaction of Application to Graduate Submission: To graduate, students must register
for 9 quarters at full MSPA Studies program tuition. Candidates must be registered for
the quarter during which the degree is conferred. Students must apply for conferral of a
degree by filling out an “Application to Graduate” form on Axess. Students may
graduate in any quarter by completing their degree requirements and filing the
“Application to Graduate” form by the deadline date for that quarter.
5. Medical Health Requirements and Immunizations: MSPA students must be in
compliance with Stanford School of Medicine medical health requirements at all times.
Entering PA students must complete certain health-related forms, immunizations, and
tests before beginning studies at Stanford and, for some of these, annually thereafter.
6. Data Security and Privacy (HIPAA) Training: MSPA students must be in compliance with
Stanford’s HIPAA training and information security requirements (MSPA Studies
Program Handbook and Policy Manual, Section 3.3.).
7. Safety Training: MSPA students must be in compliance with Bloodborne Pathogens,
Hospital-Acquired Infections, and Safety and Emergency Preparedness training
requirements as well as N95 Respirator training and fitting requirements (MSPA Studies
Program Handbook and Policy Manual, Section 3.14).
8. Ethical Conduct of Biomedical Research: MSPA students must be in compliance with the
CITI training requirement (MSPA Studies Program Handbook and Policy Manual, Section
3.6.)

8
Note on licensure: Meeting the graduation requirements for the MSPA Studies degree at the
Stanford School of Medicine does not guarantee eligibility for state licensure. Some states have
specialized curricular requirements for licensure, and students are advised to check with the
Medical or PA Board in states of possible practice.
2.3. SCHOOL OF MEDICINE TECHNICAL, NON-ACADEMIC STANDARDS
Observation
Candidates must be able to observe demonstrations and participate in experiments of
science, including but not limited to such things as dissection of cadavers; examination of
specimens in anatomy, pathology, and neuroanatomy laboratories; and microscopic study
of microorganisms and tissues in normal and pathologic states. Candidates must be able to
accurately observe patients and assess findings. They must be able to obtain a medical
history and perform a complete physical examination in order to integrate findings based
on these observations and to develop an appropriate diagnostic and treatment plan.
Communication
Candidates must be able to communicate effectively and efficiently with patients, their
families, and members of the health care team. They must be able to obtain a medical
history in a timely fashion, interpret non-verbal aspects of communication, and establish
therapeutic relationships with patients. Candidates must be able to record information
accurately and clearly, and communicate effectively in English with other health care
professionals in a variety of patient settings.
Motor Function
Candidates must possess the capacity to perform physical examinations and diagnostic
maneuvers. They must be able to respond to emergency situations in a timely manner and
provide general and emergency care. They must adhere to universal precaution measures
and meet safety standards applicable to inpatient and outpatient settings and other clinical
activities.
Intellectual-Conceptual, Integrative, and Quantitative Abilities
Candidates must have sufficient cognitive (mental) abilities and effective learning
techniques to assimilate the detailed and complex information presented in the
curriculum. They must be able to learn through a variety of modalities, including, but not
limited to, classroom instruction; small group, team and collaborative activities; individual
study; preparation and presentation of reports; and use of computer technology.
Candidates must be able to memorize, measure, calculate, reason, analyze, synthesize, and
transmit information across modalities. They must recognize and draw conclusions about
three-dimensional spatial relationships and logical sequential relationships among events.
They must be able to formulate and test hypotheses that enable effective and timely
9
problem solving in the diagnosis and treatment of patients in a variety of clinical
modalities.
Behavioral and Social Attributes
Candidates must demonstrate the maturity and emotional stability required for full use of
their intellectual abilities. They must accept responsibility for learning, exercising good
judgment, and promptly completing all responsibilities attendant to the diagnosis and care
of patients. They must understand the legal and ethical aspects of the practice of medicine
and function within both the law and ethical standards of the medical profession.
Candidates must be able to work effectively, respectfully and professionally as part of the
healthcare team, and to interact with patients, their families, and health care personnel in
a courteous, professional, and respectful manner. They must be able to tolerate physically
taxing workloads and long work hours, to function effectively under stress, and to display
flexibility and adaptability to changing environments. They must be capable of regular,
reliable and punctual attendance at classes and in regard to their clinical responsibilities.
Candidates must be able to contribute to collaborative, constructive learning
environments; accept constructive feedback from others; and take personal responsibility
for making appropriate positive changes. It is expected that minimum accommodation will
be requested with regards to this set of standards.
Ethical and Legal Standards
Candidates must meet the legal standards to be licensed to practice as a PA in the State of
California. As such, candidates for admission must acknowledge and provide written
explanation of any felony offense or disciplinary action taken against them prior to
matriculation in the School of Medicine. In addition, should the student be convicted of
any felony offense while in PA school, they agree to immediately notify the Associate Dean
for PA Education as to the nature of the conviction. Failure to disclose prior or new
offenses can lead to disciplinary action by the School of Medicine that may include
dismissal.
Equal Access to the School of Medicine’s Educational Program
The Stanford School of Medicine intends for its students and graduates to become competent
and compassionate clinicians who are capable of meeting all requirements for PA licensure.
The School of Medicine has an institutional commitment to provide equal educational
opportunities for qualified students with disabilities who apply for admission to the MSPA
Studies program or who are enrolled as PA students. The School of Medicine is a leader in
student diversity and individual rights, with a strong commitment to full compliance with state
and federal laws and regulations (including the Rehabilitation Act of 1973, the Americans with
Disabilities Act of 1990 [as amended], and California law [Civil Code 51 and 54]). A “qualified
person with a disability” is an individual with a disability who meets the academic and technical
standards requisite to admission or participation in the School of Medicine’s educational
programs, with or without accommodations. As previously noted, admitted candidates with
10
disabilities are reviewed individually, on a case-by-case basis, with a complete and careful
consideration of all the skills, attitudes and attributes of each candidate to determine whether
there are any reasonable accommodations or available options that would permit the
candidate to satisfy the standards. An accommodation is not reasonable if it poses a direct
threat to the health or safety of self and/or others; if making it requires a substantial
modification in an essential element of the curriculum; if it lowers academic standards; or if it
poses an undue administrative or financial burden. Except in rare circumstances, the use by the
candidate of a third party (e.g. an intermediary) to perform any of the functions described in
the Technical Standards set forth above would constitute an unacceptable substantial
modification.
Process
As stated above, admission and promotion at the School of Medicine is conditional on the
candidate’s having the willingness and ability to satisfy the technical standards, with or without
reasonable accommodation.
Admitted candidates who have a disability and need accommodations should initiate
discussions with the PA program’s Student Life Officer as the offer of admission is received and
accepted. The Student Life Officer is the liaison with the University’s Office of Accessible
Education (OAE). It is the responsibility of a candidate with a disability to provide sufficiently
current information documenting the general nature and extent of their disability, and the
functional limitations proposed to be accommodated. Evaluating and facilitating
accommodation requests is a collaborative effort between the candidate, the School of
Medicine, and the OAE. The School of Medicine reserves the right to request new or additional
information.
Should a candidate have or develop a condition that would place patients, the candidate or
others at risk or that may affect their need for accommodation, an evaluation with the School
of Medicine and the OAE may be necessary. As in initial assessments, a complete and careful
reconsideration of all the skills, attitudes and attributes of each candidate will be performed.
This includes an assessment of their willingness, desire and ability to complete the MSPA
Studies program curriculum and fulfill all requirements for PA licensure, and will be informed by
the knowledge that students with varied types of disabilities have the ability to become
successful medical professionals.

11
2.4. SCHOOL OF MEDICINE PROFESSIONALISM PRINCIPLES FOR PA STUDENTS
The following professionalism principles must be met in order for a student to qualify for
conferral of the MS in PA Studies degree from the Stanford School of Medicine.
Professionalism comprises those attributes and behaviors that serve to maintain patient
interests above clinician self-interest. Professionalism extends beyond interactions with
patients and their families, however. Professionalism also involves relationships and
interactions between all those involved in medical education and the delivery of patient care
including PAs, physicians, nurses, other allied health professionals, students, and
administrators. It has implications for research activities and interactions with for-profit
companies, governmental agencies, and other outside entities. Professionalism should pervade
all of our activities in medicine and should include:
1. A commitment to the highest standards of excellence in the practice of medicine and in
the generation and dissemination of knowledge.
2. A commitment to sustain the interests and welfare of patients.
3. A commitment to be responsive to the health needs of society.
The elements of professionalism include altruism, accountability, responsibility, excellence,
duty, honesty, integrity, and respect for others. Physicians, physician assistants, students, and
all staff participating in medical education and patient care at the Stanford School of Medicine
are expected to aspire to these ideals, further defined as:
Altruism
Altruism is the unselfish regard for and devotion to the welfare of others and is a key element
of professionalism. Self-interest or the interests of other parties should not interfere with the
care of one’s patients and their families.
Accountability and Responsibility
Accountability and responsibility are required at many levels – individual patients, society and
the profession. First, there must be accountability to one’s patients and to their families. There
must also be accountability to society for addressing the health needs of the public and to
ensure that the public’s needs are addressed. One must also be accountable to the profession
to ensure that the ethical precepts of practice are upheld. Inherent in responsibility is reliability
in completing assigned duties or fulfilling commitments. There must also be a willingness to
accept responsibility for errors.
Objectives and Expectations
1. Adheres to Stanford School of Medicine and Stanford Hospital policies.
2. Arrives on time and prepared for educational and patient expectations.
3. Fulfills obligations and commitments in a timely fashion.
4. Respectfully and tactfully questions policies, procedures and practices perceived as
unfair.

12
5. Takes responsibility for shortcomings and areas for improvement.
6. Recognizes errors and impairments in peers and reports these to appropriate entities.
7. Maintains personal control amidst adverse or trying circumstances.
8. Takes initiative, perseveres, and is able to prioritize and to manage time.
9. Takes on appropriate share of teamwork.
10. Reports accurately and fully on patient care activities.
11. Always ensures transfer of responsibility for patient care.
12. Informs supervisor/team when mistakes occur or when faced with a conflict of interest.
Excellence
Excellence entails a conscientious effort to exceed ordinary expectations and to make a
commitment to lifelong learning. Commitment to excellence is an acknowledged goal for all
physicians, physician assistants and students of medicine. A key to excellence is the pursuit of
and commitment to providing the highest quality of health care through lifelong learning,
education, and reflection. One must seek to learn from errors and aspire to excellence through
self-evaluation and acceptance of the critiques of others.
Objectives and Expectations
1. Demonstrates ability to practice awareness and self-reflection for lifelong personal and
professional development.
2. Balances availability to others with care for oneself.
3. Recognizes the impact of personal biases on professional conduct.
4. Actively solicits and incorporates feedback in a timely fashion.
5. Demonstrates caring, compassion and commitment to the physical and emotional
wellness of self.
6. Addresses own gaps in knowledge and/or skills.
7. Pursues and commits to providing the highest quality of health care through lifelong
learning, education and reflection.
Duty
Duty is the free acceptance of a commitment to service. This commitment entails being
available and responsive when “on call,” accepting inconvenience to meet the needs of one’s
patients, enduring unavoidable risks to oneself when a patient’s welfare is at stake, advocating
the best possible care regardless of ability to pay, seeking active roles in professional
organizations, and volunteering one’s skills and expertise for the welfare of the community.
Objectives and Expectations
1. Demonstrates caring, compassion and commitment to the physical and emotional
wellness of others.
2. Constructively approaches conflict resolution.
3. Provides constructive feedback to improve instruction.
4. Actively participates in peer and faculty oral feedback sessions and written assessments.
5. Shares responsibility for group learning, feedback, and discussions.
6. Recognizes difficulties in peers and assists them in obtaining help or remediation.

13
7. Intervenes on behalf of colleagues when others behave unprofessionally; addresses
unprofessional behavior.
8. Advocates on behalf of patients.
9. Collaborates with communities to address the social determinants of health.
10. Advocates for traditionally underserved populations.
11. Identifies barriers to care and advocates to reduce those barriers.
Honesty and Integrity
Honesty and integrity are the consistent regard for the highest standards of behavior and the
refusal to violate one’s personal and professional codes. Honesty and integrity imply being fair,
being truthful, keeping one’s word, meeting commitments, and being forthright in interactions
with patients, peers, and in all professional work, whether through documentation, personal
communication, presentations, research, or other aspects of interaction. They require
awareness of situations that may result in conflict of interest or that result in personal gain at
the expense of the best interest of the patient.
Objectives and Expectations
1. Forthright in interactions with patients, peers and in all professional work.
2. Summarizes material in one’s own voice.
3. Reports accurate data.
4. Admits errors and omissions.
5. Identifies situations where confidentiality is expected and important.
6. Demonstrates ability to negotiate informed consent.
7. Identifies components of patient competence as it relates to informed consent.
8. Understands the role of proxies when patients are unable to provide consent.
9. Demonstrates awareness of situations that may result in conflict of interest or that
result in personal gain at the expense of the best interest of the patient or others.
Respect for Others
Respect for others is the essence of humanism, and humanism is central to professionalism.
This respect extends to all spheres of contact, including but not limited to patients, families and
professional colleagues, including physicians, nurses, residents, fellows, and School of Medicine
students. One must treat all persons with respect and regard for their individual worth and
dignity. One must listen attentively and respond humanely to the concerns of patients and
family members. Appropriate empathy for and relief of pain, discomfort, and anxiety should be
part of the daily practice of medicine. One must be fair and nondiscriminatory and be aware of
emotional, personal, family, and cultural influences on patient well-being and patients’ rights
and choices of medical care. It is also a professional obligation to respect appropriate patient
confidentiality.

14
Objectives and Expectations
General Professionalism
1. Demonstrates respect for patients and colleagues.
2. Demonstrates empathy and compassion for others.
3. Is fair and nondiscriminatory.
4. Exhibits sensitivity to cultural differences among patients and colleagues.
5. Is actively inclusive of others to achieve common educational and patient goals.
6. Maintains appropriate boundaries in work relationships.
7. Uses humor appropriately.
8. Ensures that their appearance is appropriate.
Teamwork
9. Takes initiative and works collaboratively on a team.
10. Clarifies expectations and clinical responsibilities, including the student’s role on the
team.
11. Communicates with their team regarding conflicting responsibilities.
12. Recognizes that relationships between clinicians and other healthcare workers are
sometimes characterized by unequal levels of authority, yet does not abuse their
authority.
Patient Care
13. Demonstrates caring and rapport with patients.
14. Demonstrates sensitivity to and actively addresses patients' needs.
15. Exhibits sensitivity to cultural differences among patients.
16. Listens attentively and responds humanely to the concerns of patients and family
members.
17. Includes patients and families in decision making.
18. Respects patients’ dignity.
19. Maintains appropriate boundaries in dealing with patients and their families.
20. Demonstrates appropriate empathy for and relief of pain, discomfort, and anxiety.
21. Extends themselves to meet patient and family needs.
22. Takes time and effort to explain information to patients.
23. Shows sensitivity when discussing clinical information with patients.
24. Maintains decorum even when patients or others behave inappropriately.
25. Maintains composure and seeks consultation as necessary when working with
challenging patients.
15
2.5 TEACHER-LEARNER AGREEMENT
Stanford School of Medicine holds in high regard professional behaviors and attitudes,
including altruism, integrity, respect for others and a commitment to excellence. Effective
learning is best fostered in an environment of mutual respect between teachers and learners.
In the context of medical education, the term “teacher” is used broadly to include peers,
resident physicians, full-time and volunteer faculty members, clinical preceptors, nurses, and
ancillary support staff, as well as others from whom students learn.
Guiding Principles:
Duty: Medical educators have a duty to convey the knowledge and skills required for
delivering the profession‘s standard of care and also to instill the values and attitudes
required for preserving the medical profession’s social contract with its patients.
Integrity: Learning environments that are conducive to conveying professional values must be
based on integrity. Students learn professionalism by observing and emulating role models
who epitomize authentic professional values and attitudes.
Respect: Respect for every individual is fundamental to the ethic of medicine. Mutual respect
is essential for nurturing that ethic. Teachers have a special obligation to ensure that students
are always treated respectfully.
Responsibilities of Teachers and Learners:
Teachers should:
• Treat students fairly and respectfully
• Maintain high professional standards in all interactions
• Be prepared and on time
• Provide relevant and timely information
• Provide explicit learning and behavioral expectations early in a course or clerkship
• Provide timely, focused, accurate, and constructive feedback on a regular basis and
thoughtful and timely evaluations at the end of a course or clerkship
• Display honesty, integrity and compassion
• Practice insightful (Socratic) questioning, which stimulates learning and self-discovery,
and avoid overly aggressive questioning which may be perceived as hurtful,
humiliating, degrading or punitive
• Solicit feedback from students regarding their perception of their educational
experiences
• Encourage students who experience mistreatment or who witness unprofessional
behavior to report the facts immediately
16
Students should:
• Be courteous of teachers and fellow students
• Be prepared and on time
• Be active, enthusiastic, curious learners
• Demonstrate professional behavior in all settings
• Recognize that not all learning stems from formal and structured activities
• Recognize their responsibility to establish learning objectives and to participate as an
active learner
• Demonstrate a commitment to lifelong learning, a practice that is essential to the
profession of medicine
• Recognize personal limitations and seek help as needed
• Display honesty, integrity and compassion
• Recognize the privileges and responsibilities coming from the opportunity to work with
patients in clinical settings
• Recognize the duty to place patient welfare above their own
• Recognize and respect patients’ rights to privacy
• Solicit feedback on their performance
Relationships Between Teachers and Students
Students and teachers should recognize the special nature of the teacher-learner
relationship, which is in part defined by professional role modeling, mentorship, and
supervision.
Because of the special nature of this relationship, students and teachers should strive to
develop their relationship into one characterized by mutual trust, acceptance and
confidence. They should both recognize the potential for conflict of interest and respect
appropriate boundaries.

17
3.0. MSPA STUDIES PROGRAM REQUIREMENTS AND PROCEDURES
3.1. ACADEMIC RECORDS AND PRIVACY OF STUDENT RECORD INFORMATION
Transcripts
The notations used for PA program courses on official University transcripts are pass (+),
incomplete (I), continuing (N), exempt (EX) and grade not reported (GNR). Students may order
transcripts through Axess. Non-program courses will follow grading guidelines applicable to
those courses.
Education Records
The University Registrar’s Office establishes a file for each student. The file contains
confidential information, which is available to the following parties with legitimate educational
interests without prior permission from the student:
1. Dean of the School of Medicine, Senior Associate Dean for Medical Education, and/or
Associate Dean for PA Education;
2. The Office of PA Education and committees within;
3. Executive Committee of the Faculty Senate, when asked by the Dean of the School of
Medicine to review a case;
4. A duly appointed grievance or grievance appeal officer, or a duly appointed ad hoc
committee on the Suitability for the Practice of Medicine;
5. Other University officials on a need-to-know basis; and
6. Others as permitted or required by law or by University policy.
Notification of Rights Under FERPA
The following is from the the Stanford Student Services website
(https://studentservices.stanford.edu/my-information/student-records-ferpa/notification-
rights-under-ferpa).
The Family Educational Rights and Privacy Act of 1974 (FERPA) affords students certain rights
with respect to their education records. They are:
The right to inspect and review the student's education records within 45 days of the date
the University receives a request for access.
• Current and former students who wish to make a FERPA-related request to view records
should submit to the Student Services Center via e-mail at [email protected]
a request that identifies the record(s) the student wishes to inspect.
• Students are advised to provide complete information in order to assist the University in
following up on the request. Federal law requires that the University provide access to
requested extant records within 45 days. A Registrar's Office official will make
arrangements for access and notify the student of the time and place where the records
may be inspected. If the records requested are not under the control of the Registrar's
18
Office, the Registrar's Office will make arrangements for the relevant office to provide
the records within the time frame established under the law.
The right to request the amendment of the student's education records that the student
believes are inaccurate, misleading, or otherwise in violation of the student's privacy rights
under FERPA.
• A student may ask the University to amend the record that he or she believes is
inaccurate or misleading. The student should write the University official responsible for
the record (with a copy to the University Registrar), clearly identify the part of the
records he or she wants changed, and specify why it should be changed.
• If the University decides not to amend the record as requested by the student, the
University will notify the student of the decision and advise the student of his or her
right to a hearing regarding the request for amendment.
• Additional information regarding the hearing procedures is provided to the student
when notified of the right to a hearing.
The right to consent to disclosures of personally identifiable information contained in the
student's education records, except to the extent that FERPA authorizes disclosure without
consent.
• FERPA contains various exceptions to the general rule that the University should not
disclose education records without seeking the prior written consent of the student. The
following circumstances are representative of those in which education records (and
information drawn from education records) may be disclosed without the student's
prior written consent:
a) Upon request, the University may release Directory Information (see the
"Directory Information" below).
b) School officials who have a legitimate educational interest in a student's
education record may be permitted to review it. A school official is: a person
employed by the University in an administrative, supervisory, academic or
research, or support staff position (including law enforcement unit personnel
and health staff); a person or company with whom the University has contracted
(such as an attorney, auditor, or collection agent); a person serving on the Board
of Trustees; or a student or volunteer serving on an official committee (or
representing a recognized student group), such as a disciplinary or grievance
committee, or assisting another school official in performing his or her tasks. A
school official has a legitimate educational interest if the official needs to review
an education record in order to fulfill his or her responsibility to Stanford or to
the student.
19
c) The University discloses education records without consent to officials of
another school, in which a student seeks or intends to enroll, upon request of
officials at that other school.
d) The University may choose to disclose education records (and information drawn
from education records) to either supporting parent(s) or guardian(s) where the
student is claimed as a dependent under the Internal Revenue Code.
e) The University may inform persons including either parent(s) or guardian(s)
when disclosure of the information is necessary to protect the health or safety of
the student or other persons.
f) For students under the age of 21, the University may notify either parent(s) or
guardian(s) of a violation of any law or policy relating to the use of alcohol or
controlled substances.
g) The University must provide records in response to lawfully issued subpoenas, or
as otherwise compelled by legal process.
The right to file a complaint with the U.S. Department of Education concerning alleged
failures by the University to comply with the requirements of FERPA.
The name and address of the office that administers FERPA is: Family Policy Compliance Office,
U.S. Department of Education, 400 Maryland Avenue, SW, Washington, DC 20202-4605.
Directory Information
The University regards the following items of information as "directory information," that is,
information that the University may make available to any person upon specific request (and
without student consent):
• Name*
• Date of birth
• Place of birth
• Directory addresses and telephone numbers
• E-mail addresses
• SUNet ID (as opposed to Stanford Student ID Number) *
• Mailing addresses
• Campus office address (for graduate students)
• Secondary or permanent mailing addresses
• Residence assignment and room or apartment number
• Specific quarters or semesters of registration at Stanford
• Stanford degree(s) awarded and date(s)
• Major(s), minor(s), and field(s)
• University degree honors

20
• Student theses and dissertations*
• Participation in officially recognized sports or activities*
• Weight and height of members of athletic teams*
• Institution attended immediately prior to Stanford
• ID card photographs
For more information, see Stanford's FERPA website at
https://studentservices.stanford.edu/my-information/student-records-ferpa/notification-rights-
under-ferpa
Students may prohibit the release of many of the items listed above (except those with an “*”)
by designating which items should not be released using the Privacy function of Axess. Students
may prohibit the release all directory information listed above after an appointment with the
Office of the University Registrar to discuss the ramifications of this action. Student theses and
dissertations can be restricted through the publishing options and embargo settings students
select during submission.
Students, faculty, and others with questions regarding student records should contact the
Office of the University Registrar.
Consent to Use of Photographic Images
Registration as a student and attendance at or participation in classes and other campus and
University activities constitutes an agreement by the student to the University's use and
distribution (both now and in the future) of the student's image or voice in photographs, video
or audio capture, or electronic reproductions of such classes and other campus and University
activities.
If any student in a class where such photographing or recording is to take place does not wish
to have their image or voice so used, the student should raise the matter in advance with the
instructor.
21
3.2 REGISTRATION AND STUDY LISTS
The Preliminary Study List Deadline is the first day of classes of each quarter during the
academic year. As early as possible when enrollment opens, but no later than the preliminary
study list deadline, students must submit to the Office of the University Registrar via Axess a
study list to enroll officially in classes for the quarter. Students are expected to be enrolled “at
status” by the Preliminary Study List Deadline, meaning that students must be enrolled in
sufficient units to meet requirements for their status. Students will be charged a $200 late fee
for submitting their study lists after the quarterly deadline.
Study List Changes
Students may add courses or units to their study lists through the end of the third week of
classes, also known as the Final Study List Deadline. Individual faculty may choose to close their
classes to new enrollments at an earlier date.
Courses or units may be added only if the revised program remains within the normal load
limits. Courses or units may be dropped by students through the end of the third week of
classes, without any record of the course remaining on the student’s transcript.
After the Final Study List Deadline, appropriate course instructor approval must be obtained to
change course enrollment. Study List changes approved after the deadline must be submitted
to the School of Medicine Registrar’s Office.
If the instructor allows a student to take an ‘I’ (incomplete) in the course, the student must
make the appropriate arrangements for that with the instructor by the last day of classes.

22
3.3. DATA SECURITY AND PRIVACY (HIPAA)
In compliance with the Privacy Rule of the Health Insurance Portability and Accountability Act
(HIPAA) of 1996, the Stanford School of Medicine requires all new students to complete Patient
Privacy Regulation HIPAA Training before starting classes and ANNUALLY thereafter. Stanford’s
HIPAA Training is a web-based module that takes approximately 120 minutes to complete. The
Office of PA Education sends e-mail instructions to all PA students annually.
Pre-clerkship students will not receive credit for the Practice of Medicine course until they have
completed this training (both years). Clerkship students will be unable to enter their clerkships
until they have completed this training.
The training module is self-paced and is accessible through the Stanford Training and
Registration System (STARS). Log into Axess and click on the STARS tab. In the Search Catalog
box, enter the course title “HIPAA/Protecting Patient Privacy” or the course code PRIV-0010.
Students must adhere to Stanford University’s HIPAA Privacy Policies outlined at
https://uit.stanford.edu/security/hipaa.
The Data Security Program at the School of Medicine oversees compliance with Stanford policy
and federal law. To find out more about the Data Security Program, and for information on
computer encryption: https://med.stanford.edu/datasecurity/.
See sections 3.12 and 3.14 for additional information on data security and encryption.
23
3.4. PA STUDENT PRACTICE ROLE
The PA Board of California (Laws and Regulations Relating to the Practice of Physician
Assistants, Section 1399.536, Requirements for Preceptors) states that clerkships
(“preceptorships”) are supervised by a licensed physician preceptor. Other licensed health care
providers approved by a program may serve as preceptors to supplement physician-supervised
clinical practice experiences. Each preceptor participating in the preceptorship of an approved
program shall:
(1) Be a licensed health care provider who is engaged in the practice of the profession
for which he or she is validly licensed and whose practice is sufficient to adequately
expose preceptees to a full range of experience. The practice need not be restricted to
an office setting but may take place in licensed facilities, such as hospitals, clinics, etc.
(2) Not have had his or her professional license terminated, suspended, or otherwise
restricted as a result of a final disciplinary action (excluding judicial review of that
action) by any state healing arts licensing board or any agency of the federal
government, including the military, within 5 years immediately preceding his or her
participation in a preceptorship.
(3) By reason of his or her professional education, specialty and nature of practice be
sufficiently qualified to teach and supervise preceptees within the scope of his or her
license.
(4) Teach and supervise the preceptee in accordance with the provisions and limitations
of Sections 1399.540 and 1399.541.
(5) Obtain the necessary patient consent as required in Section 1399.538.
(a) It shall be the responsibility of the approved program to ensure that
preceptors comply with the foregoing requirements.
(b) For the purposes of this section, "licensed health care provider" includes, but
is not limited to, a physician, a surgeon, a physician assistant, a registered nurse
certified in advanced practice, a certified nurse midwife, a licensed clinical social
worker, a marriage and family therapist, a licensed educational psychologist, and
a licensed psychologist.
During clerkships, PA students may write orders for medications, treatments, etc., provided
that all of the following are met:
• Any medically related activity performed by students be under the direction of a
licensed health care provider who has met criteria as a preceptor as defined above.
• The students are assigned to or are consultants to the service on which the order
pertains; and
• A licensed health care provider countersigns all orders before the orders are executed.
24
The PA Board of California (Laws and Regulations Relating to the Practice of Physician
Assistants, Section 3510) also requires that a trainee enrolled in an approved program for
physician assistants shall at all times wear an identification badge on an outer garment and in
plain view, which states the student's name and the title:
Physician Assistant Student or Physician Assistant Trainee
Upon matriculating to the MSPA program, each student is provided an orange-colored badge
hanger that reads “Physician Assistant Student.” This must always be worn with the Stanford
Medicine identification/name badge along with a white coat and/or scrubs when appropriate,
when students are in a clinical setting.
When signing notes, PA students will identify their signatures with PA-S (PA Student), just as
licensed PAs identify their signatures with PA-C.
PA students are not to be involved in any portion of the medical care of other PA students.

25
3.5. STUDENT RESOURCES: ACCOMMODATIONS AND SUPPORT
Office of Accessible Education
Students with disabilities (including, but not limited to, temporary and permanent physical,
psychological, or learning disabilities) who may need academic accommodations (including
services and auxiliary aids), should register with the Office of Accessible Education
(https://oae.stanford.edu) for assessment and approval of such accommodations. Students
with documented disabilities are responsible for sharing their OAE accommodation letters with
faculty for each course, for each term in which accommodations are desired. OAE
accommodation letters are valid for one academic year; students who wish to continue
receiving accommodations should arrange for reevaluation with OAE at the beginning of each
new academic year.
Students should request accommodations well in advance of when needed. Prior to registration
with the Office of Accessible Education, students should not request accommodations directly
from faculty members. Accommodations cannot be provided retroactively.
Schwab Learning Center (SLC@CHC)
Students may contact the Schwab Learning Center (SLC) for short-term clinical therapy,
screenings for learning differences, and diagnostic evaluations for ADHD and learning
disabilities, such as dyslexia. Schwab will be available beginning in September 2021.
The SLC will still be staffed with learning specialists with backgrounds in higher education to
provide 1-1 work (unlimited hours per quarter) to help students with dyslexia, ADHD and other
suspected learning differences. This will include technology recommendations, strategies to
support learning differences in college and the workplace, and promoting understanding and
self-awareness of how students learn. SLC services are free to Stanford graduate students.
Students do not need to have a diagnosed learning difference to be eligible for SLC services;
eligibility is determined based on a number of criteria.
To get started, students should reach out to:
• Nancy Lambert for general questions: nlambert@chconline.org
• Rosinel Ermio, Learning Specialist, for questions about working with a learning specialist:
rermio@chconline.org
• Nicole Ofiesh for assessment and screening questions: nofiesh@chconline.org
Mental Health Resources: CAPS @Vaden + SoM Mental Health Team (MHT)
Mental health support is offered through Counseling & Psychological Services (CAPS) at Vaden
Health Services, as well as the School of Medicine Mental Health Team (MHT).
CAPS offers urgent and non-urgent care, 24/7. Services include crisis support, initial and follow-
up consultations, medication consultation, medication management, care management
consultation and help with treatment planning, referral assistance, workshops and outreach

26
events, and a video library. Also available are coaching support services and a Virtual Well-
Being page. The Confidential Support Team (CST) provides telehealth and phone support to
students affected by sexual assault and relationship violence.
The School of Medicine Mental Health Team (MHT) is a unit totally dedicated to Stanford
Medicine students. MHT providers are uniquely familiar with the MSPA and MD programs and
concerns common to SoM students. The MHT offers appointments during business hours, and
also has some evening-hour appointment availability for clinical MD and MSPA students. As of
autumn 2021, MHT will offer one evening slot on Tuesdays and three evening slots on
Thursdays. To make an appointment with an MHT clinician, please call the CAPS Front Desk at
(650) 723-3785, Monday through Friday, 9 a.m. – 5 p.m.
MSPA Resources
Alumni tutors for MSPA curriculum are available for students who desire additional support for
their courses. Students interested in tutoring should contact the Director of Pre-Clerkship
Education or the Directors of Clerkship Education, depending on their program phase.
The Learning Strategies Specialist is dedicated to MSPA students and will help students who
wish to improve study skills, time management, organization, and/or test-taking skills. Students
may work with the Learning Strategies Specialist to create a study plan for an exam, discuss
their learning style and test-taking strategies, or figure out how to prioritize tasks to reduce
stress. Students interested in connecting with the Learning Strategies Specialist should contact
their Faculty Advisor.
3.6. ETHICAL CONDUCT OF BIOMEDICAL RESEARCH
As part of student training in the ethical conduct of biomedical research, all MSPA Studies
Program students are required to complete the CITI Group 9 (Medical Students) module.
The deadline for completion of this requirement for incoming first-year students is December 1,
2023.
To complete this training, students must access the CITI program website
(https://www.citiprogram.org/members/index.cfm?pageID=50) once logged in to the Stanford
intranet. The Group 9 modules should already be loaded and ready.
27
3.7. EVALUATION COMPLETION REQUIREMENTS
Receiving substantive, representative feedback from students about our required MSPA Studies
program curriculum and instructors is crucial in helping the School of Medicine to understand
program strengths and weaknesses and identify opportunities to improve the educational
experience for future generations of students. In addition, learning to give and receive feedback
is an integral part of developing professional skills students will need as future clinicians.
Professionalism Requirements for Completing Evaluations
1. Students are expected to complete all evaluations assigned to them.
2. All evaluations must be completed within the assignment timeframe (due dates will be
included in the initial evaluation notice).
3. Required evaluations include:
• Entry survey as required for grant funding.
• Evaluations of all required pre-clerkship courses.
• Individual evaluations of pre-clerkship faculty lectures.
• Preceptor evaluations for the Practice of Medicine course (POM).
• Small group evaluations for POM (peer and small group leader).
• Evaluations of all required clerkships and clerkship instructors (complete all assigned
evaluations).
• Student scholarship evaluations.
• Graduation Questionnaire.
• Annual Student and Alumni Survey
4. For the pre-clerkship curriculum, completion rates on evaluations will be reviewed at
the midpoint of each quarter as part of the mid-quarter check-in process, and again
after each quarter has finished and the evaluation due dates have passed. If a student
has not completed at least 75% of the evaluations assigned during the quarter, their
advisor will be alerted. The student will receive feedback about professionalism
expectations from their faculty advisor.
5. Evaluation completion rates will continue to be checked each quarter. If a student
completes less than 75% of the evaluations assigned during a subsequent quarter, their
advisor will be alerted that there has been a second lapse in professionalism with regard
to evaluations. The student will receive additional feedback regarding professionalism
expectations and a warning that any further lapse may result in a referral to the Student
Progress Committee.
6. If a student completes less than 75% of evaluations in another quarter (third violation),
the student may be referred to Student Progress Committee for a professionalism
concern.
7. Failure to complete other required evaluations (clerkship, student scholarship work,
etc.) may also lead to the student’s advisor being notified. Repeated failure to complete
these assigned evaluations may also result in a referral to Student Progress Committee.

28
Use of Professional Language in Evaluations
1. Comments provided in evaluations should be constructive, respectful and framed using
language that the evaluator would want to hear used if they were being evaluated.
2. Written comments provided in student evaluations are anonymous (i.e., faculty cannot
access information about the identity of an individual student who provides comments
in an evaluation form). However, if a student submits a written comment in an
evaluation form that violates either a) the Stanford Affirmation
(http://med.stanford.edu/pa/handbook-policies.html) or b) the Stanford School of
Medicine Technical, Non-Academic Standards (see Section 2.3), or c) if there are
concerns about student safety or wellbeing, that evaluation form may be subject to
review.
3. Any instructor, staff, or student may request that a comment be reviewed to determine
whether it violates the Stanford Affirmation or the Stanford School of Medicine
Technical, Non-Academic Standards, or if there are concerns about student safety or
wellbeing.
4. Comments in question will be brought before the Student Progress Committee for
review.
5. If the SPC review determines that the comment violates the Stanford Affirmation or the
Stanford School of Medicine Technical, Non-Academic Standards, or if there are
concerns about student safety or wellbeing, SPC will recommend escalation to the
Associate Dean for PA Education, who will review the recommendation and may contact
the vendor where the evaluation data is housed to request the identity of the student
who submitted the evaluation at issue.
6. The student who wrote the comment that is determined to have violated the Stanford
Affirmation and/or the Stanford School of Medicine Technical, Non-Academic Standards
will be notified of the situation by their Faculty Advisor or, in the case of a conflict of
interest, an SPC-assigned designee. The student may be asked to revise the evaluation
and/or submit an apology to the faculty member and/or the course or curriculum leader
the comment targeted.
7. In the case of a violation of the Stanford Affirmation or the School of Medicine
Technical, Non-Academic Standards, the student’s advisor will be notified of the
violation. The student will receive feedback about professionalism expectations and a
warning that a second lapse will lead to a referral to the Student Progress Committee.
8. If the student submits a second evaluation containing a comment that is determined to
have violated the Stanford Affirmation or the Stanford School of Medicine Technical,
Non-Academic Standards, the student will be referred to the Student Progress
Committee for a professionalism concern.

29
3.8. INDUSTRY INTERACTIONS POLICY
MSPA students, as members of the Stanford Medicine community, are expected to adhere to
the Stanford Medicine Industry Interactions Policy (SMIIP).
Purpose of Policy
The purpose of this policy is to establish guidelines for interactions with Industry
representatives throughout Stanford Medicine, which is composed of the Stanford School of
Medicine, Stanford Health Care and the Lucile Packard Children’s Hospital Stanford.
Interactions with Industry occur in a variety of contexts, including marketing of new
pharmaceutical products, medical devices, and hospital and research equipment and supplies
on-site, on-site training of newly purchased devices, the development of new devices,
educational support of medical students and trainees, and continuing medical education.
Faculty and trainees also participate in interactions with Industry off campus and in scholarly
publications in a variety of circumstances including consulting activities of various sorts. Many
aspects of these interactions are very positive and important for promoting the educational,
clinical and research missions of Stanford Medicine and for translating knowledge and expertise
from the faculty to society. However, these interactions must be ethical and cannot create
conflicts of interest (COI) that could endanger patient safety, data integrity, the integrity of our
education and training programs, or the reputation of either the faculty member or the
institution. Individuals must consciously and actively divorce clinical care decisions from any
perceived or actual benefits expected from any company. It is unacceptable for patient care
decisions to be influenced by the possibility of personal financial gain. See policy for Conflicts of
Interest in Clinical Care.
Statement of Policy
It is the policy of the Stanford School of Medicine, Stanford Health Care and the Lucile Packard
Children’s Hospital Stanford that interactions with Industry should be conducted so as to avoid
or minimize conflicts of interest. When conflicts of interest do arise, they must be addressed
appropriately, as described herein.
The full policy is available online at http://med.stanford.edu/smiip/home.html.

30
3.9. LEAVES OF ABSENCE AND DISCONTINUATION AND REINSTATEMENT
MSPA students can request a leave of absence or withdrawal from the program for medical or
personal reasons. Students must make this request in writing to the Program Director and
follow all University procedures as noted below. If a student withdraws from the program, a
student must reapply to the program for consideration of future matriculation.
Given the advancing curriculum of the MSPA program, a leave of absence from the program will
likely result in the need for the student to decelerate. The student might need to audit the
courses they have successfully completed and begin their coursework where they left off the
prior year. The modification of the curriculum due to a deceleration or leave of absence is at
the discretion of the Program Director and is not automatically granted.
University Policies
Leave of Absence
A leave of absence is required by graduate students who wish to withdraw from the University
for the current quarter, or who do not wish to attend a future quarter (excluding Summer
Quarter).
The following is quoted from the Stanford University Registrar’s Office website (8/15/2022,
https://studentservices.stanford.edu/more-resources/student-policies/leaves-
reinstatements/graduate-degrees-leaves-reinstatements):
“Leaves of absence are granted for a maximum of one calendar year, or four quarters. Leaves
requested for a longer period are approved only in exceptional circumstances (for example,
mandatory military service). An extension of leave, for a maximum of one year or four quarters,
is approved only in unusual circumstances. Extension requests must be made before the
expiration of the original leave of absence. Leaves of absence for graduate students may not
exceed a cumulative total of two years (eight quarters including summer quarters).”
Students should review all possible ramifications of taking a leave of absence. Students are
encouraged to check with all other appropriate University offices (e.g., Housing Assignments,
Financial Aid, Student Financial Services, Bechtel International Center, Vaden Health Center) to
determine how taking a leave of absence impacts their status with these offices. Students on
leave of absence are not registered and therefore do not have the rights and privileges of
registered students. They cannot fulfill any of-ficial department or University requirements
during the leave period.
Graduate students are subject to special registration requirements; see the “Leave of Absence”
section of the Stanford Bulletin. (https://studentservices.stanford.edu/my-academics/time-
away-stanford-leave-withdraw-return/leaves-absence)

31
Leave of Absence Procedures for Graduate Students
1. Review the Leave of Absence Form via Axess (directions at
https://studentservices.stanford.edu/my-academics/time-away-stanford-leave-withdraw-
return/leaves-absence - submit)
2. Discuss plans with MSPA Faculty Advisor and all pertinent MSPA team members.
3. Submit the completed Leave of Absence form. It will be routed for MSPA approvals, and
also for approval from the Bechtel International Center if applicable.
Leave of Absence Policies
Graduate students may not take a leave of absence during their first quarter of enrollment.
Deadlines
Before a given quarter:
The deadline to submit a Leave of Absence for a full refund is the Preliminary Study List
deadline. To ensure a full refund, submit a fully completed and properly endorsed Leave of
Absence form by the Preliminary Study List deadline.
During a given quarter:
The deadline to submit a Leave of Absence form for a partial refund is the Term Withdrawal
deadline. Graduate students must submit a Leave of Absence form to the Student Services
Center. All courses for that term are dropped if the last day of attendance is prior to the Final
Study List deadline. Axess does not allow students to drop all courses themselves. Submitting a
Leave of Absence form after the Final Study List deadline results in ‘W’ notations on the
transcript for all registered courses.
After the term withdrawal refund deadline (60% of the quarter), a Leave of Absence is granted
only for approved health or emergency reasons with supporting documentation.
Refund Policy
Policies and procedures for refunds for tuition can be found on the Stanford Bulletin
(https://studentservices.stanford.edu/my-academics/time-away-stanford-leave-withdraw-
return/leaves-absence - deadlines-refund)
Tuition
Leaves of Absence Before the First Day of Classes:
Students who take a leave from the University voluntarily on or before the first day of classes
will receive a full tuition refund. Such students are not included in University records as
registered for the term.

32
Leaves of Absence After the First Day of Classes:
An active student in good standing who voluntarily takes a leave from the University after the
first day of instruction, but before the term withdrawal deadline, receives a pro rata refund.
There is no refund after the Term Withdrawal deadline. Courses in which the student was
enrolled after the Final Study List deadline appear on the student’s record and show the grade
of ‘W’ (withdrew).
Extending a Leave or Returning from a Leave at a Different Time
A Leave of Absence form must be completed (with the extension portion of the form filled out)
by a student who wishes to extend an initial leave of absence.
For graduate students, an Application for Reinstatement in Graduate Study (accessible in the
eForms section in Axess) must be submitted by a student who did not submit a Leave of
Absence form and was discontinued for no enrollment. Both an application fee and
reinstatement fee apply.
Student Status While on Leave
Academic Status
Students on an approved Leave of Absence retain their admitted student status; however, they
are not registered and therefore do not have the rights and privileges of registered students.
Students on leave may complete coursework for which an ‘Incomplete’ grade was reported in a
prior term and are expected to comply with the one-year maximum time limit for resolving
incompletes.
Graduate Students
Degree programs and candidacy must be valid in the term of reenrollment. Leaves do not delay
candidacy or master’s program expiration dates. Failure to return as scheduled or to secure an
extension of a prior leave will result in cancelation of registration privileges and a substantial
reinstatement fee. Official department or University requirements (e.g., qualification
examinations) cannot be fulfilled during the leave period.
International Students
Nonimmigrant students and their dependents must maintain an appropriate visa status at all
times. An absence from the U.S. of five or more months will result in termination of F-1 or J-1
status. If a student remains outside the U.S. for five or more months, a new I-20 or DS-2019 is
necessary for re-entry. For further information, contact Bechtel International Center.
Financial Aid
Students should notify the Financial Aid Office of their intent to leave the University if they are
receiving any type of aid, particularly to protect eligibility for certain programs and funds such
as Cal Grants while on leave. A portion of any refund is returned to the sources of aid. Students
should clear all outstanding bills with the Student Services Center before returning to campus.
Graduate students may apply for loans four weeks before the first day of classes in the quarter

33
in which they plan to return. See the Financial Aid (https://financialaid.stanford.edu) website
for detailed application requirements.
Loans
Students must notify all lenders of their intent to leave the University and request exit
information before leaving campus (Stafford and private loans through the Financial Aid Office;
Perkins and Institutional loans through Student Financial Services). Students are cautioned to
consider carefully the effect of leaves on their loan status; lenders may count the leave period
as part of the total grace period. Stanford will provide enrollment status to the National
Student Loan Clearinghouse. Students who receive loan disbursements directly may be
required to repay portions of their loans.
University Housing
University housing is generally not available to students on leave. Students with questions
about room-and-board refunds should contact the Stanford Housing Assignment Services or the
central office of the University Dining Services (for board refunds). Students with medical
disabilities that require University medical services and students approved for the Childbirth
Accommodation may petition to remain in campus housing for one term while on leave.
Approval requires good academic standing, department recommendation, and no outstanding
financial obligations to the University. Address questions to the appropriate unit at
https://rde.stanford.edu/studenthousing.
Health Insurance
Contact Vaden Health Center at (650) 723-2135 or visit the Vaden website
(https://vaden.stanford.edu/insurance-referral-office) for information regarding Cardinal Care
coverage and/or Dependent Plan Insurance during a student leave of absence. If you have a
question or problem, you can submit a Help Ticket (https://stanford.service-
now.com/student_services).
Library
Contact the Privileges Division at Green Library to determine whether you may retain access
and/or borrowing privileges while you are on leave.
Our Lane Medical Library (https://lane.stanford.edu) continues to be available to you while you
are on leave, as your SUNetID will continue to allow you access.
34
3.10. MALPRACTICE LIABILITY FOR MSPA PROGRAM STUDENTS
Stanford assumes the financial responsibility for medical malpractice liability incurred by
registered MSPA students when they are participating in any clinical activities as part of their
formal educational program at the Stanford University Medical Center, or at other Stanford-
approved medical facilities. However, it is very important that Stanford MSPA students be
certain they are protected when participating in clinical work in special situations. Therefore,
students should consult the Clerkship leadership team if they will be:
1. Undertaking a clinical clerkship at another hospital or PA school in the United States
while not paying tuition and not registered as a PA student at Stanford.
2. Undertaking a clinical experience in a foreign country while not paying tuition and not
registered at Stanford.
3. Participating in any volunteer clinical work away from Stanford.
4. Working in a private physician’s office.
5. Participating in any clinical activities not at Stanford that are not covered in (1) through
(4) above.
Stanford reserves the right, without prior notice, to modify its practices with regard to financial
responsibility for medical malpractice liability.

35
3.11. MEDICAL HEALTH REQUIREMENTS AND IMMUNIZATIONS
Medical Requirements
All matriculated Stanford students must complete the Entrance Medical Requirements
(https://vaden.stanford.edu/about/entrance-health-requirements) at their own expense. These
requirements are based on the Centers for Disease Control and Prevention recommendations
for health professionals and monitored by Vaden Student Health Center
(https://vaden.stanford.edu).
Vaccines
Measles, Mumps, Rubella (MMR)
• 2 doses of live vaccines MMR/MMRV or
• Laboratory evidence of immunity
Varicella
• 2 doses of Varicella vaccine or
• Laboratory evidence of immunity
1
Hepatitis B
• Three doses of Hepatitis B vaccine or
• Laboratory evidence of immunity from vaccination (Hepatitis Surface Antibody) or
• Laboratory evidence of natural immunity (have had past hepatitis B infection)1. This must
include results for Hepatitis Surface Antibody, Hepatitis B Core Antibody and Hepatitis B
Surface Antigen.
1
Equivocal antibody titers are not considered sufficient to protect from infection and a
complete vaccine series will be administered as recommended by the CDC-ACIP.
Tetanus, diphtheria, pertussis (Tdap)
• Tdap: Booster must be within past 10 years, regardless of last Td vaccine
Students are expected to comply with evolving University vaccination requirements.
Strongly Recommended Vaccines
• COVID-19 vaccine. Students should be advised that while the COVID-19 vaccine is strongly
recommended but not required by the University, it is required by most clerkship sites.
Recommended Vaccines
In addition to the required immunizations above, Stanford also recommends that students
consider the following immunizations if applicable:
• Hepatitis A vaccine.
• Human Papillomavirus vaccine.

36
• Meningococcal vaccine.
• Pneumococcal vaccine (for those with a history of asthma or other lung diseases, an
immunocompromising condition, or cigarette smoking).
• A completed polio vaccine series.
Required Testing
• Tuberculosis (TB): Quantiferon (required prior to matriculation and annually)
Annual Tests and Immunizations
After matriculation, the following tests/immunizations are required of each MSPA student
ANNUALLY:
• Tuberculosis (TB): Quantiferon.
• Influenza: All MSPA Studies program students must be immunized against influenza.
Immunizations and tests can be performed at the following location:
Vaden Student Health Center (https://vaden.stanford.edu)
866 Campus Drive
Stanford, CA 94305-8580
(650) 498-2336
Additional tests or immunizations required by specific clerkships will have documentation on
file with the clerkship team of these requirements.
Annual immunizations required by the School of Medicine and its clerkships are performed at
the School of Medicine’s expense.
If a student is not in compliance with required immunizations and annual testing, an enrollment
hold will be placed on the student’s account preventing enrollment. The hold will be released
once the student is in compliance with the required immunizations and annual testing.
Clerkship students who are out of compliance may have their rotations paused until they
become compliant. Student compliance with required screenings, testing and immunizations
are considered a component of professionalism. If a student fails to meet required deadlines,
their Faculty Advisor will be notified. The student will receive feedback regarding
professionalism expectations and a warning that any further lapse may result in a referral to the
Student Progress Committee.

37
3.12. POLICIES AND RESOURCES FOR DEVICE ENCRYPTION, SECURITY AND USE
As all MSPA students will at some point in their training access Protected Health Information
(PHI), they should always attest Yes to “may access or receive High Risk data,” and all devices
used for Stanford work (even just email) must be appropriately encrypted and fully compliant
with School of Medicine data security standards. This applies to all Stanford Medicine students
at all times, whether or not they are currently accessing or storing PHI, even if stepping out of
the curriculum to obtain another degree.
Attestation and data security compliance by stated deadlines are a professional expectation. If
attestation and encryption is not completed following a notification reminder, the student will
be referred to the Student Progress Committee.
Personal Responsibility
Legally, students are personally and fiscally responsible for any information disclosure from
their computer or mobile devices, whether accidental or not. TDS Information Security Services
is here to help students protect themselves: encryption is a one-time, necessary step students
can take now to prevent problems in the future.
Data Classification: What Data Must Be Encrypted?
Stanford University has classified information assets into categories to determine which
security precautions must be taken to protect it against unauthorized access. Data may be
classified as High, Moderate or Low Risk. Common types of High-Risk data include:
Health Information, including Protected Health Information (PHI)
Health Insurance policy ID numbers
Social Security Numbers
Credit card numbers
Financial account numbers
Export controlled information under U.S. laws
Driver's license numbers
Passport and visa numbers
Donor contact information and non-public gift information
The School of Medicine Data Security Policy requires the encryption of all computers and
mobile devices used for Stanford work by an individual who might access Protected Health
Information (PHI) or other High Risk data. This applies to both Stanford-owned and personally-
owned equipment.
For more information, see the University risk classification standards and encryption
requirements.
Because personal computing devices are becoming more and more portable—laptops, smart
phones, USM thumb drives, etc.—securing the sensitive information stored on those devices is

38
more important than ever. Based on government regulations, individuals may be held
personally and fiscally liable in the event of information disclosure. Students are expected to
review and follow the policies outlined below:
• Mobile Device Management (https://uit.stanford.edu/service/mobiledevice/management)
If students have an iOS or Android device that is used for Stanford work, there's an easy
way to set up and maintain proper security practices on the device with Stanford’s Mobile
Device Management (MDM) apps. The applications are free to install, and automatically
configure your device to be optimized for the Stanford environment—from email settings
to security settings. Visit the link provided above for more information about MDM at
Stanford.
• Stanford School of Medicine Course Content Access and Appropriate Use Policy
(http://med.stanford.edu/edtech/services/ClassroomTechnologies/course-content-
access.html)
Students may only use Stanford School of Medicine course materials as intended for
curriculum and course-related purposes. These materials are copyrighted by the University
or others. Access to this content is for personal academic study and review purposes only.
Unless otherwise stated in writing, students may not share, distribute, modify, transmit,
reuse, sell, or disseminate any of this content.
• High Risk Data and HIPAA Compliance (https://uit.stanford.edu/guide/riskclassifications)
Students must ensure all devices used for Stanford work fully comply with Stanford’s data
security requirements and HIPAA guidelines. As medical students are expected to interact
with High Risk data (such as PHI), all devices must be verifiably encrypted. The University’s
BigFix application is used to report the encryption status of laptops and desktops regularly.
MDM (AirWatch) is used to report the encryption status of mobile devices. Additional
requirements include ensuring a password is set and that all backups are encrypted.
• Stanford University Computer and Network Usage Policy
https://bulletin.stanford.edu/pages/BFR6SWHFxkWJ2Z0BKGxq
Students must respect copyrights and licenses, respect the integrity of computer-based
information resources and refrain from seeking to gain unauthorized access, and respect
the rights of other information resource users.
• Stanford Medicine Bring Your Own Device (BYOD) Policy
(http://med.stanford.edu/edtech/services/ClassroomTechnologies/byod.html)
Stanford Medicine is a “Bring Your Own Device (BYOD)” campus. What does this mean?
• In pre-clerkship courses, students will use their own device for online quizzes and
exams, and potentially other classroom activities. Students will be asked to install
secure browsers on their devices at the beginning of the year for examinations.
• In clerkship courses, students will use their own devices for exams. Instructions will be
provided to install the required secure browser prior to the exam.

39
The School of Medicine EdTech and AV Tech teams provide support for required courses
and clerkships during examinations to ensure a smooth experience. Please visit BYOD at
Stanford Medicine for the latest details on system recommendations. If you have any
questions, please contact EdTech at [email protected].
• Loaned iPads
Policies and guidelines around appropriate use of iPads may vary among clerkships and
hospital sites. Therefore, students must review and follow the policies and guidelines set
by the clerkship leadership team and by each hospital site. The privilege of using an iPad
may be rescinded at any time. Students who do not follow policies and guidelines for
appropriate iPad use may be asked to return the device prior to completing the clerkship
rotation.
See sections 3.3 Data Security and Privacy (HIPAA) Training and 3.15 Stanford Medicine Policy
for the Removal and Transport of PHI for additional information.
40
3.13. RESPECTFUL ENVIRONMENT AND MISTREATMENT POLICY
I. Standards
A. Stanford School of Medicine is committed to providing a work and educational
environment that is conducive to teaching and learning, research, the practice of
medicine and patient care. This includes a shared commitment among all members of
the School of Medicine community to respect each person’s worth and dignity, and to
contribute to a positive learning environment where medical students are enabled and
encouraged to excel. Given their roles in the educational process and their inherently
unequal positions vis a vis students, all instructional personnel (including faculty,
residents, and other members of the healthcare team) are to treat students with
courtesy, civility and respect and with an awareness of the potential impact of their
behavior on such students’ professional futures.
B. Conduct inconsistent with this policy can occur in a variety of forms and may seriously
impair learning. In particular, instructional personnel are expected to create an
environment in which feedback regarding their performance can be given openly by
students without concern for reprisal, and which is free of exploitation, harassment,
impermissible discriminatory treatment, humiliation, or other mistreatment or abuse of
medical students. Examples of conduct inconsistent with these standards might include:
• Sexual harassment
• Physical or verbal abuse
• Assigning duties as punishment rather than education
• Requiring a student to perform personal services (such as shopping or babysitting)
• Unwarranted exclusion from reasonable learning or professional opportunities
• Evaluation or grading on inappropriate criteria (or threatening to do so)
• Harassment or discrimination on the basis of sex, race, age, color, disability, religion,
sexual orientation, gender identity, national or ethnic origin, or any other
characteristic protected by applicable law
C. Note: The expectations stated in this policy primarily relate to the standards of
conduct for instructional personnel. For their part, MD and MSPA students are expected
to adhere to similar standards of respectful and professional behavior, including (but not
limited to) the standards of conduct for students set forth in the MD Program Handbook
and Policy Manual and website.
II. Guidelines for Application
A. These standards of conduct are applicable to all School of Medicine instructional
personnel (including faculty, residents, teaching assistants and other members of the
healthcare team) in their interactions with Stanford medical students—whether on or off
campus and whether in formal educational (such as clinical or classroom) or in social
settings.

41
B. In general, a determination of whether specific conduct is inconsistent with this policy
will depend on a case-by-case analysis of the particular facts and circumstances, and the
use of a “reasonable medical student” standard.
C. Students subjected to abuse, discrimination, mistreatment or harassment have a right
to seek timely and effective remediation with the full support of the School of Medicine
and Stanford University. In addition, retaliation and/or reprisals against an individual
who in good faith reports or provides information in an investigation about conduct that
may violate this policy is prohibited.
D. Conduct inconsistent with this policy may consist in repeated actions or may even
arise from a single incident if sufficiently egregious.
E. In the review of conduct under this policy, other Stanford University and School of
Medicine policies and procedures (such as Stanford’s Prohibited Sexual Conduct Policy)
may become relevant.
III. The Respectful Environment and Mistreatment Committee
The Respectful Environment and Mistreatment Committee is a standing committee to carry out
the purposes and procedures set forth in this policy.
A. The committee meets monthly, and on an ad hoc basis if it is deemed necessary by
the Chair.
B. The committee is chaired by the Associate Dean for Medical Student Life Advising, who
is hereafter referred to as the Chair.
C. The composition of the committee includes the following as members:
• The Chair
• One or more students (clinical and preclinical) from both the MD and MSPA program
• A student selected by SUMMA (Stanford University Minority Medical Alliance)
• A student selected by SNMA (Student National Medical Association)
• An Academic Advising Dean
• The Director of Graduate Medical Education (or designee)
• The Assistant Dean for Clerkship Education
• The Assistant Dean for Preclerkship Education
• The Director of Educators for CARE
• A Residency Training Program Director
• A faculty or staff member with specific knowledge and sensitivity to racial issues and
instances of bias
• A faculty or staff member with specific knowledge and sensitivity to LGBTQ+ issues
and instances of bias

42
• A faculty or staff member with specific knowledge and sensitivity to ability issues
and instances of bias
• A Resident
• The Chair of the Physician Wellbeing Committee
• A faculty member from the MSPA program
D. The REMC will keep such confidential records of its proceedings as are appropriate to
support its purposes of education and concern resolution.
IV. Procedures
The following procedures for handling incidents of potential violations of the Standards of
Conduct for the Teacher-Learner Relationship place a strong emphasis on resolving complaints
informally. The procedures include advising and mediation. It is important to note that the
procedures do not preempt other formal or informal channels available within the
University. It is recommended that students should -- as a first step-- contact the Chair of the
Respectful Environment and Mistreatment Committee to review the various options that are
available (on a confidential basis as that status is granted to the Associate Dean for Medical
Student Life Advising). The Chair is empowered to explore with the student a plan of action
that may include some or all of the steps described below. Alternatively, there are three
anonymous avenues to report a concern: 1) MedHub; 2) SAFE report, and 3) on an end of
Course or end of Clerkship evaluation.
A. Informal: Concern about potential violations may be handled by communication with
various individuals, including but not limited to the following:
1. Direct discussions (by the student or others) with the alleged offender.
2. Conversation (by the student or others) with individuals such as the chief resident,
attending physician, clerkship director, and/or Educator-4- Care (E4C) faculty.
3. The Chair may present the concern to all or a portion of the committee, and to such
third parties that the Chair deems appropriate for seeking an informal resolution.
4. The Chair may enlist one of the trained Mistreatment Coaches to educate the
person who is the source of the concern.
5. The Chair also may in his/her discretion refer the matter to an alternate available
University process or office, such as an existing grievance process or the Sexual
Harassment Policy Office or the Director of the Diversity and Access Office.
6. Direct conversation by the student with confidential resources including but not
limited to the Ombuds, Counseling and Psychological Services, and the Deans of
Religious Life.
Informal solutions to address the problem may be recommended and/or pursued such
as (but not limited to) systems changes or educational interventions. The Chair will be
available throughout the process to discuss with the student the status of the matter,
including any potential resolution.
43
B. Formal: If no resolution is reached and the student wishes to proceed with a more
formal grievance or complaint process, the Chair may refer the student to other existing
processes or may (in an appropriate case) accept from the student a written grievance or
complaint to use the procedure described below.
1) The student should set forth in writing the substance of the grievance or complaint,
the grounds for it and the evidence on which it is based, and the efforts taken to
date to resolve the matter. It is at this stage that the matter becomes a formal
grievance or complaint.
2) The grievance or complaint document should be submitted to the Chair. A grievance
should be filed in a timely fashion, i.e., normally within thirty days of the end of the
academic quarter in which the action that is the subject of the grievance or
complaint occurred. A delay in filing may be grounds for rejection of that grievance
or complaint.
3) The Chair will review the grievance or complaint and (if it reflects an appropriate use
of the process) will then promptly (within 7 days) transmit the grievance or
complaint to the Senior Associate Dean for Medical Education (SADME) for handling.
4) The SADME shall promptly initiate a review, which should normally be completed
within sixty days. The SADME may attempt to resolve the matter informally and
may refer the matter (or any part of it) to a grievance officer or other designee, who
will evaluate and/or address the matter as the SADME directs. The SADME may
also, in appropriate cases, remand the matter to the appropriate administrator
(including to the administrative level at which the grievance or complaint arose) for
further consideration.
5) In undertaking this review, the SADME (or their designee) may request a response to
the issues raised in the grievance or complaint from any individuals believed to have
information the reviewer considers relevant, including faculty, staff and students.
6) The SADME (or their designee) shall issue their decision in writing and take steps to
initiate such corrective action as is called for (if any). Conduct meriting discipline
shall be brought to the attention of the appropriate disciplinary process.
7) Appeal
a) If the student is dissatisfied with the disposition by the SADME (or their designee),
they may appeal to the Dean of the School of Medicine. The appeal should be
filed in writing with the Dean within ten days of the issuance of the decision by
the SADME (or their designee); a delay in filing the appeal may be ground for
rejection of that appeal.
b) The Dean may attempt to resolve the matter informally and may refer the matter
(or any part of it) to a grievance appeal officer or other designee, who will review
the matter at the Dean’s direction. The Dean also may remand the matter to the
appropriate administrator (including to the administrative level at which the
grievance arose) for further consideration.
c) The Dean should normally complete his or her review of the appeal and issue his
or her decision in writing within forty-five days. That decision is final. It is not
subject to further review by any other University process.
44
V. General Provisions
A. Time Guidelines: The time frames set forth herein are guidelines. They may be
extended by the Chair, the SADME or the Dean, as applicable, in his or her discretion
for good cause (including for reasons relating to breaks in the academic calendar).
B. Advisers: A student initiating or participating in a grievance or complaint under this
procedure may be accompanied by an adviser in any discussion with the Chair, the
SADME, the Dean, or their designees (such as a grievance or grievance appeal officer);
such adviser must be a current Stanford faculty, staff member or student.
C. Ombuds: Students should be aware that the University Ombuds and the School of Medicine
Ombuds are available to discuss and advise on any matters of University concern and
frequently help to expedite resolution of such matters. Although it has no decision-
making authority, the Ombuds’ Office has wide powers of inquiry.
D. Sexual Harassment and Disability related issues: For further information and resources
concerning sexual harassment and sexual violence, students should refer to the web
page of the Sexual Harassment/Assault Response & Education-Title IX Office. For
further information and resources concerning disabilities and accessible education,
students should refer to the web page of the Office of Accessible Education and/or the
Diversity and Access Office.
E. No retaliation: Stanford University prohibits retaliation or reprisals against individuals
based on their pursuit in good faith of a grievance or complaint under this procedure,
or their participation in good faith in the grievance or complaint process.
F. Standards for Review: If the grievance or complaint involves a decision that is being
challenged, the review by the SADME, as well as the review by the Dean on appeal,
usually will be limited to the following considerations:
1. Were the proper facts and criteria brought to bear on the decision? Were improper or
extraneous facts or criteria brought to bear that substantially affected the decision to
the detriment of the grievant?
2. Were there any procedural irregularities that substantially affected the outcome of
the matter to the detriment of the grievant?
3. Given the proper facts, criteria, and procedures, was the decision one which a person
in the position of the decision maker might reasonably have made?
VI. Education
The Stanford School of Medicine will provide ongoing education to promote a positive learning
environment and discourage violations of the standards of conduct for the teacher-learner
relationship. Such education serves several purposes. First, it promotes an environment of

45
respect for each person’s worth and dignity. Second, it informs students that there are
procedures available for them to register concerns of educator conduct violations, which can be
investigated and addressed without fear of retaliation. Third, it informs instructional personnel
of the School of Medicine’s standards of conduct and procedures for responding to allegations
of violations of these standards. Educational sessions on this topic will be introduced during the
pre-clerkship curriculum and readdressed early in the clinical curriculum. Educational sessions
on this topic will also be presented to educational personnel including but not limited to at
forums such as resident orientation, department meetings, and staff meetings. The materials
and methods for providing this education will be the responsibility of the Respectful
Environment and Mistreatment Committee.
3.14. SAFETY TRAINING
Bloodborne Pathogens Training
The California OSHA (Occupational Safety and Health Administration) Bloodborne Pathogens
Standard requires that all individuals with occupational exposure to blood, blood products, or
other potentially infectious materials complete a Bloodborne Pathogens training course
ANNUALLY. This requirement applies to all MSPA students. Stanford University Bloodborne
Pathogens Training is a web-based training that takes approximately 30 minutes to
complete. The Office PA Education sends e-mail instructions to all MSPA students annually.
Pre-clerkship students will not receive credit for Practice of Medicine (POM) course until they
have completed this training (both years). Clinical students are not able to enter the Clerkship
until they have completed this training.
The training module is self-paced and is accessible through STARS. Log into Axess and click on
the STARS tab. In the Search Catalog box, enter the course title “Bloodborne Pathogens” or the
course code EHS-PROG-1600.
Safety and Emergency Preparedness Training
All MSPA students are required to complete the following three online courses:
• General Safety, Injury Prevention (IIPP) and Emergency Preparedness (EHS-4200)
• Biosafety (EHS-1500)
• Chemical Safety for Labs (EHS-1900) is required for all MSPA students in laboratories.
Compliance is monitored by the lab administrators
These courses are accessed through STARS in Axess.
46
3.15. STANFORD MEDICINE POLICY FOR THE REMOVAL AND TRANSPORT OF PHI
Purpose
The purpose of this policy is to set forth controls related to removal of Protected Health
Information (PHI) or Personal Information (PI) from the medical center and transport of medical
information within the medical center. This policy does not replace IT Security policies for
protection of electronic patient information including requirements related to emailing patient
information.
Policy Statement
Stanford Health Care (including all SHC-affiliated locations), Lucile Packard Children’s Hospital
(including all LPCH-affiliated locations), and the Stanford School of Medicine (collectively,
“Stanford Medicine”) are committed to complying with state and federal requirements related
to the privacy and security of patient information. Workforce Members at Stanford Medicine,
as well as those with whom Stanford Medicine conducts its business, have a legal and ethical
responsibility to maintain the confidentiality, privacy and security of all PHI/PI, to protect PHI/PI
at all times and to guard against the loss of, or unauthorized access to, use or disclosure of,
PHI/PI when removing it from the medical center up through its return, and when transporting
it within the medical center. Such removal and transport of PHI/PI shall not occur in a manner
inconsistent with this policy. Principles and procedures in this policy apply to PHI/PI in all
media, including paper and electronic format. Consistent with other policies, PHI/PI that is
removed from the premises should never be verbally discussed with any unauthorized person.
Definitions
Protected Health Information (“PHI”) is defined as information that (i) is created or received by
a health care provider, health plan, employer, or health care clearinghouse; (ii) relates to the
past, present, or future physical or mental health or condition of an individual; the provision of
health care to an individual; or the past, present or future payment for the provision of health
care to an individual; and (iii) that identifies the individual, or provides a reasonable basis to
identify the individual. PHI does not include employment records held by Stanford Medicine in
its capacity as an employer, or information that has been de-identified in accordance with the
HIPAA Privacy Standards.
Personal Information (“PI”) is a person’s first name and last name, or first initial and last name,
in combination with any one of the following data elements that relate to such person:
• Social Security Number (SSN);
• Driver’s license or state-issued identification card number; or
• Financial account number, credit or debit card number (e.g., health insurance policy
number).
Personal information shall not include information that is lawfully obtained from publicly
available information, or from federal, state or local government records lawfully made
available to the general public.
47
De-identification is defined as the process by which PHI is stripped of specific data elements, as
defined by HIPAA, in order to assure that personal identities cannot readily be identified from
data sets.
Workforce Members are defined as faculty, employees (including temporary employees),
researchers, volunteers, trainees, and other persons whose conduct, in the performance of
work, is under the direct control of Stanford Medicine, whether or not they are paid by
Stanford Medicine.
Supervisor: For the purposes of this policy, Supervisor is used in the context of approval for a
Workforce Member to remove PHI/PI from the medical center or transport PHI/PI within the
medical center. It is understood that from time to time the duties of senior operational
leadership (Directors and above) and faculty will require them to conduct Stanford Medicine
business for which this policy requires Supervisor approval. Such approval for senior
operational leadership and faculty is self-granted, provided that they have ensured that all
safeguards and other privacy and security controls are in place. For research activities,
Supervisor means the Principal Investigator or Protocol Director.
Medical Center is any location owned, leased or operated by Stanford Medicine, wherever
located.
Principles
1. PHI/PI shall be treated as confidential and shall be safeguarded according to Stanford
Medicine policies at all times.
2. Treatment, payment, healthcare operations, education, IRB-approved research and
other Stanford Medicine business involving the permissible use or disclosure of PHI/PI
should be conducted within the medical center whenever feasible. Removal of PHI/PI
from the medical center by Workforce Members shall occur solely for job-related
purposes and with the approval of the Workforce Member’s Supervisor. Removal of
PHI/PI from the medical center should not be approved for reasons related to the
convenience of the Workforce Member, but rather for instances where the work
requiring the PHI cannot practically be conducted on-site in a timely manner, and only
after due consideration of alternative ways to remotely perform the work, such as VPN
access to PHI/PI or secure scanning of PHI/PI for access from the remote site.
3. The Workforce Member taking the PHI/PI off-site and the approving Supervisor are
responsible for ensuring that only the minimum amount of PHI/PI necessary to perform
the off-site work is approved and removed from the medical center. De-identified
patient information or limited data sets shall be used whenever possible. The approving
Supervisor and the Workforce Member removing the PHI/PI, or the Workforce Member
transporting the information within the medical center, should be able to account for
every element of PHI/PI removed from or transported within the medical center,

48
whether electronic or paper, and should be able to reconstruct the exact PHI/PI that
was removed from or transported within the medical center.
4. Appropriate safeguards shall be diligently followed regarding secure transport of PHI/PI
off-site and within the medical center. PHI/PI must be in the immediate personal
possession of the workforce member at all times during transport, for example, from
the time the PHI/PI is taken from the medical center to the time of arrival at the off-site
location, or from location-to-location within the medical center.
5. Appropriate safeguards shall be diligently followed regarding securing PHI/PI at the off-
site location. PHI must be secured in a manner so that it cannot be accessed by
unauthorized individuals.
In the case of PHI that is lost, stolen, accessed, viewed or reviewed by unauthorized
individuals, or the confidentiality of which has been otherwise compromised, it is
essential that the Stanford University Privacy Office be notified immediately. There are a
number of federal and state privacy laws which may require Stanford to take very
specific actions within very defined timelines. The Privacy Office will work with you to
gather all of the relevant facts to ensure Stanford complies with all of our privacy
obligations. A loss or theft counts as a Privacy Incident; report it to the Stanford
University Privacy Office, by email at privacy@stanford.edu, or by phone: (650) 725-
1828. For more information about a lost or stolen device, see
https://med.stanford.edu/irt/security/help.html
Procedures
1. PHI should be saved or stored on secure medical center network servers whenever
feasible. Saving or storing PHI/PI on computer or laptop hard drives, personal laptops or
other personal devices, flash drives or USB drives, external drives, and other removable
media is prohibited unless the device is encrypted to Stanford Medicine standards,
password protected and meets other applicable Stanford Medicine security
requirements.
2. Before the decision is made by the Workforce Member and the Workforce Member’s
supervisor to remove electronic PHI from the premises, IT Security must be contacted to
determine whether a viable alternative is available to remotely access the PHI/PI
needed to perform the job-related work.
3. PHI/PI should not be printed at off-site locations, for example, home or public printers,
unless a Stanford Medicine business need exists to do so.
4. Safeguards must be in place to prevent unauthorized individuals, such as family
members, conference attendees or the general public, from viewing or accessing PHI/PI
at off-site locations.
49
5. PHI/PI must be safeguarded during transport and in the personal possession of the
Workforce Member at all times. PHI shall not be left unattended in publicly accessible
locations.
6. PHI/PI transported for purposes such as off-site storage, office relocation and new
location openings shall be safeguarded to prevent the loss of or unauthorized access to
PHI/PI. Only medical center approved off-site storage locations may be used for storing
records, documents and electronic media containing PHI/PI. Records and documents
containing PHI must be inventoried before off-site storage. See Appendix B for securing
documents and records containing PHI/PI for off-site storage or office/department
relocation
Compliance
1. All Workforce Members are responsible for ensuring that individuals comply with those
policy provisions that are applicable to their respective duties and responsibilities.
2. Workforce Member failure to protect the privacy, confidentiality, and security of patient
information is detrimental to the mission, goals, and operations of Stanford Medicine.
Serious consequences can result from failing to protect patient information, up to and
including termination.
3. Violations of this policy will be reported to the Privacy Office and any other department
as appropriate or in accordance with applicable Stanford Medicine policy. Violations will
be investigated to determine the nature, extent, and potential risk to Stanford
Medicine.

50
3.16. STANFORD SCHOOL OF MEDICINE EDUCATION RESEARCH POLICY
All research involving MSPA students requires approval by the student’s faculty advisor and
their Leadership Track lead. Research examining the MSPA Studies program or MSPA students
or alumni also requires the approval of the Associate Dean for PA Education.
The process and timing for submitting research ideas, objectives, and the Thesis project
proposal are provided in Q1. An overview of the IRB approval by the Stanford University
Research Compliance Office (https://researchcompliance.stanford.edu) is presented in Q2.
Important: In general, any data gathering and analysis with the intent to disseminate findings
to a broader scientific community would be considered research and should be reviewed and
approved by the IRB (via the Stanford University Research Compliance Office,
https://researchcompliance.stanford.edu). All other projects by MSPA students will require
submission of a “Determination of Human Subject Research Application Form” to determine
if formal IRB approval is indicated.
3.17. STUDENT PARTICIPATION IN CLINICAL ACTIVITIES INVOLVING PERSONAL RISK
The Stanford University School of Medicine has long had the policy that students learn to be
clinicians by participating in the care of patients under faculty supervision. Some of these
patients may have an infectious or other disease that provides some risk to caretakers,
including students. While every effort will be made to provide appropriate training and
safeguards for students so that these risks are minimized, they cannot be totally eliminated.
Students are required to participate in patient care as one of their fundamental responsibilities
during their medical education. Students are expected at all times to follow universal safety
precautions in order to safeguard their own health. Under certain rare and extenuating
circumstances where the risk to the student significantly outweighs either the educational
benefit to the student or the health-care benefit to the patient, a supervising clinician may
suggest that a student be exempted from, or a student may ask permission from the
supervising clinician to be excused from, participation in certain aspects of patient care.
The course and/or clerkship director are responsible for providing guidance and clarification of
this statement and resolving any disputes. In the event a dispute is unsatisfactorily resolved
from the standpoint of either the student or the supervising clinician, the matter may be
referred to the Director of Pre-Clerkship Education or Director of Clerkship Education for final
review as necessary.
51
3.18. SURGICAL PROCEDURES FOR MSPA STUDENTS
An MSPA student must meet all of the following conditions and criteria in order to scrub and/or
participate directly in a surgical procedure.
1. Each Stanford MSPA student must:
a. Complete the scrub training
i. Initial training: Full course with knowledge test and scrubbing/gowning
checklist.
1. Red sticker for pre-clerkship students. Initial training valid for one year
from training date.
2. Green sticker for clerkship students. Initial training valid for two years
from training date.
ii. Clerkship students:
1. Pre-clerkship trained (red sticker) students will be required to
complete an online course with medical knowledge test and
scrub/gowning verification to convert to clerkship (green) certification
iii. Students scrub training certification will require that this sticker be visible on
their name badge.
2. The lists of names and documentation to attest meeting requirements to scrub received
from each surgical division/department are kept with the Goodman Surgical Education
Center or the education/administration office.
3. Student may scrub and participate in surgical cases only if they have an OR-approved
sticker affixed on their name badge as a proof that the student underwent appropriate
training in aseptic techniques.
4. If a student’s name is not present on the list submitted by their respective surgical
division/department, they will be denied presence in the OR and be dismissed until
credentials are verified.

52
3.19. UNIVERSAL PRECAUTIONS AND NEEDLESTICK PROTOCOL
MSPA students are required to take the necessary precautions to avoid injury and exposure to
infectious and hazardous materials. In addition to the required training noted in section 3.14,
students must actively ensure that they take necessary precautions, including following
universal precautions, utilizing personal protective gear (gloves, gowns, surgical and N95 masks
etc.), and disposing of sharps and soiled materials appropriately. All MSPA students are
required to have healthcare coverage. The financial responsibility for treatment will be borne
by the student and their healthcare plan.
Needle Stick Policy and Procedures
If you are stuck by a needle or splashed with bloody fluid, follow the steps below
immediately.
1. If sharps injury: Wash skin with soap/water x 15 minutes. If eyes: flush with 500cc
lactated Ringers or normal saline; if mouth/ nose: flush with water x 15 minutes
2. Activate 1-STIX Pager for OHS BBP Advice RN (24/7/365)
• Page Operator (650) 723-6661: Ask for 1-STIX pager (17849)
3. Obtain Source Patient's Blood by cooperating with site hospital personnel:
• Name/MRN/Unit Location/ HIV, HBV, HCV status
Follow-up services may be advised by OHS BBP RN for testing at University Services at
484 Oak Rd (650) 735-5308 or in the basement of 300P.
QUICK & CONVENIENT - A trained professional will contact you and order medication from
pharmacy near you. Follow-up may be advised by the OHS BBP Advice RN at University services
at 484 Oak Rd (650-725-5308) or Stanford Employee Health in the basement of 300P.
CONFIDENTIAL - Does not become part of your health care record.
FREE - No charge for services obtained via hotline.
Keep a copy of the 1-STIX orange card with your Hospital ID Badge at all times. Hotline
problems? Email the wellness team at [email protected].
If you are at Pioneers, please contact the Pioneers Clinical Site Director via phone call, text, or
secure e-mail to help coordinate treatment at Occupational Health. If sending a text message,
confirm your name and share that you have a “Code Zebra” and request a call back. Please
bear in mind that text messages are not PHI-safe, hence the use of a code phrase is necessary.
If you are at a Central Valley site, please contact the Central Valley Clinical Site Director as
outlined above. If you are at TriValley, please also contact the TriValley Clinical Site Director.
If you are at any other site type, or are unable to connect with a site director, please contact
the clerkship leadership team as outlined above.

53
Follow up appointments may be needed but this will be recommended by the 1-STIX
professional staff person. This has been set up specifically for Stanford MD AND MSPA
students and employees so that it is QUICK, CONFIDENTIAL and with NO CHARGE. Records are
kept confidential in accordance with applicable laws so that it does not become a part of your
health care record. This is a protection for you.
If you have any problems with the hotline, please contact Dr. Rebecca Smith-Coggins
immediately. Dr. Smith-Coggins can be reached through the hospital page system at (650) 723-
6661, at pager 13481, or via email at [email protected].
If you choose to go to the Emergency Department, the hospital will charge you and it will go on
your health care record. Please call the Needlestick Hotline first.
Regardless of where the exposure occurred, you must notify the MSPA clerkship leadership
team via secure e-mail within 1 business day.
Universal Precautions
Universal Precautions apply to the handling of all blood, body fluids, and human tissue. Body
fluids, also known as other potentially infectious materials (OPIM), include: semen; vaginal
secretions; cerebrospinal, synovial, pleural, peritoneal, pericardial, and amniotic fluids; feces,
urine; sputum; nasal secretions; saliva; tears; vomitus; or any other body fluid or tissue that is
visibly contaminated with blood. Appropriate protection, including gloves, mask, and gown,
should be worn to protect oneself from exposure.

54
3.20. STANFORD HEALTH CARE/LUCILE PACKARD CHILDREN’S HOSPITAL STANFORD
COMPUTER ACCESS FOR PA STUDENTS (EPIC)
As a Stanford MSPA student registered in a clerkship for credit and/or doing an approved
research project, you will/may need access to the Epic systems (EMR, or Electronic Medical
Records) in order to access patient information at Stanford Health Care (SHC) and/or Stanford
Children’s Health (SCH or LPCH).
Obtaining Access to Epic
Am I Compliant?
1. You must be compliant with your Stanford University HIPAA/PHI training(s) in Axess
2. You must be compliant with the Data Security Policy
(https://med.stanford.edu/irt/security.html)
Hospital Computer Access
1. Contact the MSPA program if you need hospital computer access:
a. You need access because you will be working in clinics for your Practice of
Medicine course (POM).
b. You need access because you’re doing an approved research project and you
require access to Epic.
2. The MSPA program will submit your information to the Medical Staff Office (MSO) to
start the credentialing process.
3. Once the MSO notifies the MSPA program that your dictation number/MSO number has
been enabled, it will take approximately 24 hours for your credentials to become active.
a. For SHC Epic access: You will receive an email from HealthStream (module
accessible in Axess) with instructions to complete the Epic training courses “SHC
Epic New Hire Provider - Medical / PA Students” and “SHC Epic New Hire
Provider Inpatient - Medical / PA Students”. Please complete the training at your
earliest convenience.
i. The MSPA program will submit a request to the IT department (Access
Control and Epic Security) to assign you an SID and grant you SHC Epic
access. It may take up to 72 hours for your SID to be assigned and up to
an additional 72 hours for your Epic access to be granted.
ii. Once you receive your access confirmation email, call the Stanford Digital
Solutions Service Desk at (650) 723-3333 to receive a temporary
password. This password will only be valid for 24 hours; if it expires, you
will need to call again.
iii. You should log in for the first time from an SHC-networked computer at
one of the hospitals, Lane Library, or LKSC. Once you have successfully
logged in, you may submit a request for remote access if you need it.

55
iv. For SCH (LPCH) Epic Access: You may call the Stanford Children’s IR
Service Desk at (650) 498-7500 after your dictation number is assigned to
request your username and password. SCH Epic utilizes different login
credentials than SHC Epic. If you already have SHC Epic access, you can
call the SCH Service Desk and request your username and password at
any time. You should use the following specific language: “I am a Stanford
MSPA student who currently has Epic access and I need my username
and password.” They will ask for an identifier, such as your SID or social
security number.
If Your Account is Inactive
There are a few reasons that your Epic account may be inactive:
• You have not completed the HealthStream Epic training modules. Please contact
EpicEduc[email protected] for assistance.
• You completed the module within the past 48 hours. It will take up to 48 hours for your
access to be activated following completion of the training module. Contact the Service
Desk at (650) 723-3333 if you have an urgent need to access Epic.
• Your Epic credentials have expired. If you do not log in for 90 days, your Epic access will be
deactivated. Please contact the MSPA program to reactivate your access.
• Your SID may have expired. For security reasons, an SID is valid for one year, but it can be
renewed easily. Digital Solutions will send weekly email reminders beginning one month
before your SID is scheduled to expire. These emails contain a link to request access
extension. If you do not submit an extension request in time, your account will expire and
you will need to contact the MSPA program to be onboarded again.
Whom to Call?
Stanford Health Care Help Desk
Phone: (650) 723-3333 for access issues; 650-724-EPIC(3742) for functional issues
Email: [email protected]rg
Stanford Children’s Health Service Desk
Phone: (650) 498-7500
Epic Training
Email: Ep[email protected]

56
3.21. SCHOOL OF MEDICINE LEARNING SPACES
General Learning Spaces
All Learning Spaces (exceptions are the Goodman Immersive Learning Center [see below] and
the Berg Conference Center) may be booked by students for study, seminar discussions, etc.
These spaces include EdTech classrooms in: LKSC (floors 1-3), MSOB, Alway, CCSR and HRP.
Students are advised that after-hours activities that may require housekeeping will need to be
planned in advance. Rooms must be returned to their original condition. More information can
be found at https://med.stanford.edu/medscheduler/features.html.
Goodman Immersive Learning Center (ILC)
The Goodman Immersive Learning Center in LKSC may be scheduled only by course
coordinators and/or faculty for guided learning exercises and activities. The hours of operation
of the ILC are 8:00 am – 6:00 pm Monday – Friday. More information can be found at
https://med.stanford.edu/medscheduler/features.html.
Safety and Emergencies
In the case of an emergency (fire, security, medical, chemical spill, etc.) call X-C286.
If evacuation is necessary, please move to designated evacuation-meeting locations outside of
buildings and look for the Building Response Team in the bright vests.
Cell phone reception may be limited in basement facilities.
TA Training: All TAs must adhere to TA lab training and safety policies that are referenced in the
TA Handbook.

57
3.22. ABSENCE POLICY AND EXPECTATIONS
It is the student’s professional responsibility to review the absence policy and specific
attendance requirements for all courses, clerkships and curricular activities in which they are
involved. Students should avoid scheduling or participating in activities that directly conflict
with required sessions, courses or clerkships.
Required Courses
1. Students are expected to be present at ALL required-attendance sessions and final
exams. It is the student’s responsibility to be aware of the attendance expectations for
each course. Generally, attendance is required for MSPA students at all regularly
scheduled class sessions.
2. If a student anticipates missing a required-attendance session, they must communicate
and receive approval from the course director at a minimum of two weeks in advance.
In cases involving illness and unexpected emergencies, students should notify their
course director as soon as possible and submit an absence request form (see below)
thereafter.
a. All students are required to complete the Absence Request Form
(https://stanforduniversity.qualtrics.com/jfe/form/SV_bqDVfMBaZWWkhyl)
regardless of whether the absence has been approved. If the student and course
director are unable to agree on the appropriateness of an absence for a required
session, they are encouraged to schedule a meeting with the course director and
the student’s faculty advisor to discuss the absence further.
b. Approval of all absences is at the discretion of the course director.
c. If an absence is not approved, it is expected that the student will make the
necessary arrangements to change their schedule to be present.
3. Students are responsible for the content and work associated with all missed sessions.
Students are also expected to meet the participation requirement and contribute to
their group’s learning, even for sessions missed, and must work out an equitable
solution that balances the individual student’s needs with the needs of the group. Under
no circumstances will an absence relieve a student of meeting all of the academic
requirements of the course. If the absence request conflicts with a session or sessions
that cannot be otherwise made up or completed, the student is advised that the
absence may affect their performance evaluation in the course.
4. Students are expected to meet all deadlines and requirements for timely completion of
coursework.
5. The following are considered professionalism issues and a student’s Faculty Advisor will
be notified. The student will receive feedback regarding professionalism expectations

58
and a warning that any further lapse may result in a referral to the Student Progress
Committee.
i. Absence from a required session without obtaining advance approval from the
course director.
ii. Failure to communicate with the course director.
iii. Failure to complete the online Absence Request Form.
iv. Trend in number of absences across courses.
v. Tardiness for required sessions without obtaining advance approval from the
course director.
Please note that each student is responsible for requesting approval for their own
absence; no group approvals will be granted.
Required Clerkships
• Students are expected to attend 100% of all scheduled clerkship activities.
• Students who miss more than 10% of scheduled time—for any reason—will be required to
make up missed time.
• Students who miss more than 20% of the total duration of a clerkship—for any reason—
will be required to make up the missed time or reschedule the clerkship.
• Students must contact the clerkship team at mspa-c[email protected] to obtain
advance approval for any unavoidable absence from a clerkship. Unanticipated absences
for illness or emergency must be communicated to the Clerkship leadership team and to
preceptors/site staff as promptly as possible.
• If a student is absent without obtaining advance approval from the clerkship leadership
team, the absence will be recorded and reported to the Student Progress Committee.
• Approval of all absences is at the discretion of the clerkship leadership team.
• If an absence is not approved, it is expected that the student will make the necessary
arrangements to change their schedule to be present.
• Failure to communicate with the clerkship leadership team about unavoidable absences is
a potential reason for failing the clerkship.
• Students are expected to seek necessary health care to maintain their physical and mental
well-being. Examples of necessary health care include preventive health services, visits for
acute illness, ongoing care for chronic illnesses, physical therapy, and counseling and
psychological services. Consistent with their rights under University policies and the law,
students have a right to privacy when seeking care.
• For planned absences related to healthcare, students must contact the clerkship leadership
team, site director, and preceptor or patient care team in advance to coordinate time away
from the clerkship. Students need not disclose the specific type of healthcare that is being
sought. A student’s decision to seek healthcare during a clerkship should have no impact
on their performance evaluation.
• Students who experience mistreatment or who witness unprofessional behavior should
report the facts immediately to the clerkship leadership team.

59
3.23. N95 RESPIRATOR MASK FIT REQUIREMENTS FOR PA STUDENTS
All MSPA students participating in clinical activities are required to be fit for a N95 Respirator
on an annual basis. N95 filtering face-piece respirators are air-purifying respirators certified by
the National Institute of Occupational Safety and Health (NIOSH) that protect against airborne
contaminants (i.e., dusts, fumes, microbial agents such as tuberculosis bacteria & flu virus). Fit
testing is the process used to determine the appropriate N95 respirator mask (type and size) to
ensure consistent and proper mask use. As a medical student participating in clinical activities,
you may be required to wear a N95 respirator mask for tasks such as entering isolation rooms
and other activities involving close contact with potentially infected persons.
All students are responsible for maintaining compliance with the annual fit testing requirement
and must self-report the results of their fit test by completing the N95 Respirator Fit Testing
Self Attestation Form (SUNet ID required).
Stanford Occupational Health Services (OHS), located in Stanford Hospital, 300 Pasteur Palo
Alto, CA, Ground Floor, Room H0124, oversees the mask fit testing process. Per OHS policy and
Cal/OSHA guidelines, users must first be medically cleared to determine if they are physically fit
to wear a respirator.
In response to the COVID crisis, Stanford Hospital has approved the use of industrial grade N95s
in conjunction with an approved face shield. Medical students who are fit tested for an
industrial grade mask must adhere to this policy.
Students are responsible for maintaining compliance with the annual fit testing requirement.
To maintain compliance, students must:
• Print and complete both the N95 Respirator Medical Evaluation Questionnaire and the
OHS Annual Fit Testing Form.
• Bring both completed forms to Stanford Occupational Health Services (OHS) at Stanford
Hospital, 300 Pasteur, Palo Alto, CA, Ground Floor, Room H0124) during regular business
hours: (Monday: 7am-2pm; Tuesday: 7am-3:30pm; Wednesday: 7am-2pm; Thursday:
7am-3:30pm; Friday: 7am-1pm; closed on weekends and holidays). Fit testing
is provided as a courtesy to students on a first-come, first-served basis. Hospital
employees do take priority, therefore, you may be asked to return at a later date
depending on OHS' workload.
o Students must be clean shaven (no mustaches, beards, or stubble), since this will
interfere with the respirator seal. Students who are not clean shaven will not be fit
tested (see below for more information).
• At the end of the fit session, students should take a picture of the completed OHS
Annual Fit Testing Form before leaving. OHS will place a sticker on the student’s
Stanford Medicine ID badge indicating fit test date and mask type.
• Lastly, students must self-report the results of their fit test by completing the N95
Respirator Fit Testing Self Attestation Form.

60
During fit testing and when wearing a N95 respirator mask, students must be clean shaven (no
mustaches, beards, or stubble), since this will interfere with the respirator seal. Students who
are not clean shaven will not be fit tested. Students requesting an exemption to the clean-
shaven guidelines will need to sign the N95 Respirator Fit Facial Hair Notification and Waiver
and complete a separate HealthStream Training Module for a Controlled Air Purifying
Respirator (CAPR), which consists of a battery powered HEPA filter which blows purified air into
a loose-fitting hood worn over the head. CAPR users require annual training. CAPR hooded
supplied air-systems may not be readily available when N95 mask protection is required.
Compliance with the annual N95 fitting process is considered a component of professionalism.
In the event that a student is not compliant, a hold may be placed on their registration and
their Faculty Advisor will be notified. The student will receive feedback regarding
professionalism expectations and a warning that any further lapse may result in a referral to the
Student Progress Committee.
Clerkship students should be advised that different clinical sites may have their own policies
regarding fit testing, and students may need to complete additional fit testing prior to starting
rotations at these sites.

61
3.24. SCHOOL OF MEDICINE DRESS CODE GUIDELINES FOR THE CLINICAL SETTING
Any time students see patients, they should adhere to the dress code described below. Dress
code guidelines must be followed at all encounters with patients, standardized or real.
Students are expected to dress professionally and conservatively. Attire typically worn to class
or lecture will in many cases not be appropriate. Hospital scrubs are not considered
professional attire for ambulatory/outpatient clinical encounters.
• Always bring your white coat. Your coat must be clean, pressed and worn at all times.
• Wear your name tag in an easily viewable location (collar of coat, top, or dress).
• Do not wear cologne or perfumes.
• Tattoos should be covered.
• Jewelry should be minimal and understated.
• Clothing should not have rips, tears or frayed edges.
• Do not expose your midriff.
• Clothing should allow for an appropriate range of movement and should not be flashy or
draw attention.
• Button-down shirts (with or without ties), professional tops, or blouses should be worn.
and should avoid low-cut necklines.
• Tank tops, halter tops, racerback tops, sleeveless tops, t-shirts, and thin or “spaghetti-
style” straps on tops are not appropriate.
• Athletic clothing, including hooded sweatshirts, is not appropriate.
• Do not wear political campaign buttons or symbols representing a cause, excluding those
defined as “protected activity” by the National Labor Relations Board or a health initiative.
• Denim clothing, including pants, skirts, and jackets, is not appropriate.
• Pants, slacks, khakis, skirts, or dresses are appropriate. Legs should be covered to the knee.
• Do not wear jeans, capri pants, yoga pants, leggings, or shorts.
• Dress shoes, low heels, or flats should be worn. Open-toed shoes, sandals, flip- flops, or
porous shoes are not appropriate.
• Sneakers should not be worn in the ambulatory/outpatient setting.
• Long hair must be tied back or up.
• Nails must be natural and short. Long nails, acrylic/artificial nails, overlays, tips, nail wraps,
etc. are not appropriate.
62
3.24. SCHOOL OF MEDICINE CRIMINAL BACKGROUND CHECK POLICY
The School of Medicine requires Criminal Background Checks for all MSPA students.
The following outlines the rationale for performing Criminal Background Checks:
• To facilitate the placement of students into clinical training programs.
• To bolster the public's continuing trust in the medical profession.
• To enhance the safety and well-being of patients.
• To ascertain the ability of accepted applicants and enrolled PA students to eventually
become licensed as PAs.
• To minimize the potential liability of medical schools and their affiliated clinical facilities.
3.25. MSPA PROGRAM POLICY ON VOLUNTEERING AND WORKING FOR THE PROGRAM
The MSPA program discourages students from working during their PA education and reminds
students to prioritize their education when considering engaging in other activities. The MSPA
program cannot require students to work for the program.
Students with specific knowledge, experience, or skills may assist faculty in didactic and
workshop sessions to share their knowledge and skills. However, students are not permitted to
be the primary instructor or instructor of record for any component of the curriculum.
While on clerkship, students are not permitted to function in any medical/clinical role outside
of a PA student. As an example, a student is not allowed to function as a medical assistant or
scribe.

63
4.0. CURRICULUM
4.1 CURRICULUM OVERVIEW
Courses and Units
Total for Graduation: 182
Quarter 1:
Foundations of Clinical Medicine 4 units
Histology 1 unit
Embryology 1 unit
Clinical Anatomy I 11 units
Practice of Medicine I 8 units
PAs in Health Care I 1 unit
Quarter 2:
Clinical Therapeutics I 2 units
Practice of Medicine II 5 units
Principles of Clinical Medicine I 8 units
Foundations of Clinical Neurosciences 2 units
Quarter 3:
Clinical Therapeutics II 2 units
Practice of Medicine III 6 units
Principles of Clinical Medicine II 10 units
Quarter 4:
Clinical Therapeutics III 3 units
Practice of Medicine IV 8 units
Principles of Clinical Medicine III 12 units
PAs in Health Care II 2 units
Quarter 5:
Clinical Therapeutics IV 2 units
Practice of Medicine V 6 units
Principles of Clinical Medicine IV 10 units
PAs in Health Care III 2 units
Quarter 6:
Clerkships 18 units
PAs in Health Care IV 1 unit
Quarter 7:
Clerkships 18 units
PAs in Health Care IV 1 unit
Quarter 8:
Clerkships 18 units
PAs in Health Care IV 1 unit
Quarter 9:
Clerkships 18 units
PAs in Health Care IV 1 units

64
4.2. ACADEMIC CALENDAR
The School of Medicine's Academic Calendar combines dates relevant to all our matriculating
programs: MD, MSPA, MS, and PhD. As an MSPA student, it is your responsibility to review the
academic calendar and to be present and available for required MSPA program activities.
Please visit the School of Medicine's Academic Calendar for the up-to-date changes and note
key administrative dates on your calendar.
The following is a sample schedule of the pre-clerkship phase of the program. It should be
noted that this is a sample, and the actual schedule may vary; please refer to course syllabi and
Canvas for the most accurate schedule information.
During the clerkship phase, student schedules will vary according to rotation. Students should
generally plan to have a full schedule during weeks 1-3 of the rotation and be in clinic Monday –
Wednesday of week 4, with a callback to campus at the end of the week. The End of Rotation
exam will be administered on Thursday morning, and PAs in Healthcare IV will meet on Friday
morning.

65

66

67
68
4.3. ACADEMIC REQUIREMENTS FOR GRADUATION
Academic Units
A minimum total of 182 academic units is required for all students. Please see section 4.1 for a
list of the courses that constitute the 182 academic units. Details of the courses are provided in
section 4.5.
Students cannot graduate with any uncorrected failing or incomplete grade in a pre-clerkship
course or any uncorrected failing or incomplete grade in clinical clerkships.
Additional Requirements
Thesis/Capstone: Completion of Thesis/Capstone project and presentation, as outlined in
section 4.4.
Elective courses are only permitted during the didactic phase of the curriculum and their
meeting times should not conflict with required courses. The maximum number of course units
per quarter during the didactic phase are:
• Quarter 1/1A: 34 units
• Quarter 2: 24 units
• Quarter 3: 24 units
• Quarter 4: 34 units
• Quarter 5: 24 units
69
4.4. LEADERSHIP TRACK AND THESIS PROJECT REQUIREMENT
Each MSPA student is required to select a leadership track and complete a Thesis project
prior to graduation. The areas of focus are limited to and include:
• Clinical Research
• Community Health
• Health Services and Policy Research
• Medical Education
• Healthcare Administration
Students should take at least 6 units of elective coursework in their Leadership Track area that
helps support the development and successful completion of their Thesis project.
During the first quarter, students are encouraged to explore and compare the different
Leadership Track areas and their course and research opportunities. Each student must declare
a Leadership Track by submitting their course plan, learning objectives, and general project
description to the Director of Student Scholarship and their respective Leadership Track lead by
the end of the first quarter.
Students are also required to submit a written report of their scholarly work and present their
project at the Thesis Symposium held in the last Winter Quarter. A final complete Thesis paper
is due at the end of Q8 (December).
Compliance with Thesis deadlines is considered a component of professionalism. In the event
that a student is not compliant with a Thesis deadline, their Faculty Advisor will be notified.
The student will receive feedback regarding professionalism expectations and a warning that
any further lapse may result in a referral to the Student Progress Committee. In addition, failure
to meet established deadlines may result in a delay in graduation and the need for continued
enrollment and tuition payment beyond 9 quarters.
70
4.5. REQUIRED PRE-CLERKSHIP COURSES
Year 1, Q1: Autumn
Foundations of Clinical Medicine
Histology
Embryology
Clinical Anatomy
Practice of Medicine I
PAs in Health Care I: Introduction to the Profession
PAS 201: Foundations of Clinical Medicine
This course explores fundamental concepts of biochemistry, genetics, microbiology, and
immunology as applied to clinical medicine, in a mostly “flipped classroom” format. This course
will help to establish a foundation for understanding the pathophysiology of disease and the
targets for therapeutic interventions.
Discipline-specific topics include:
• Biochemistry: thermodynamics, enzyme kinetics, vitamins and cofactors, metabolism of
carbohydrates, lipids, amino acids and nucleotides, and the integration of metabolic
pathways.
• Genetics: basic principles of inheritance and risk assessment, illustrated with the use of
clinical examples from many areas of medicine including prenatal, pediatric, adult, and
cancer genetics.
• Microbiology: basic bacteriology, virology, mycology, and parasitology, including
pathogenesis and clinical scenarios associated with infectious diseases.
• Immunology: concepts and applications of adaptive and innate immunity and the role of
the immune system in human disease.
INDE 218: Histology
This course focuses on the microscopic structure of the major organ systems, including the
cardiovascular, respiratory, gastrointestinal, renal, and reproductive systems. Sessions examine
the unique features of the cells and tissues that comprise the major organs, describe how they
contribute to the organs' functions, and explore how they form the foundation for many
pathologic processes.
SURG 201: Embryology
The course focuses on the structural development of the human body, from embryo to fetus to
early postnatal life. Topics include formation of the cardiovascular, respiratory,
musculoskeletal, gastrointestinal, reproductive, and renal systems, as well as common clinical
conditions which arise from abnormalities of development.
SURG 203: Clinical Anatomy
Introduction to human structure and function presented from a clinical perspective. Includes
clinical scenarios, frequently used medical imaging techniques, and interventional procedures

71
to illustrate the underlying anatomy. Students are required to attend lectures and engage in
dissection of the human body in the anatomy laboratory.
INDE 201: Practice of Medicine I
Practice of Medicine is a five-quarter series extending throughout the first two years of the
MSPA and MD programs, interweaving core skills training in medical interviewing and the
physical examination with other major threads addressing the context of medical practice:
information literacy, nutrition principles, clinical epidemiology and biostatistics, evidence-based
practice, psychiatry, biomedical ethics, health policy, population health. Core clinical skills are
acquired through hands-on practice and are evaluated through an extensive program of
simulated medical encounters, in which students interview, examine, and manage patients in a
mock clinic. The information literacy thread introduces students to informatics and knowledge
management, biomedical informatics, and evidence-based medicine searching. Nutrition
principles are acquired through interactive, web-based instruction and reinforced through
problem-based learning cases, which run in parallel to the basic science components over the
first year. In epidemiology, students learn the taxonomy of epidemiological studies, how to
critically read a journal article, and how to recognize and understand the concepts behind
different clinical study designs. Topics include bias, confounding, diagnostic testing and
screening, and “how statistics can lie.” Psychiatry introduces students to the unique role of
MSPA students in talking with patients, the difference between process and content in patient
communication, how to respond to breaks in the patient-provider relationship, and the
relationship between the quality of the patient-provider interaction and health outcomes.
Health care policy covers such topics as health insurance, provider payment, health care costs,
access, measurement and improvement of quality, regulation and health care reform.
Biomedical ethics includes important ethical issues in medical practice, such as confidentiality,
privacy, and ethical issues relating to medical students. The population health curriculum
exposes students to concepts of public health, community action, and advocacy, and includes a
year-long, community-based project. At the end of this quarter, students participate in a
performance-based assessment of the medical interview skills.
PAS 291: PAs in Health Care I
This course provides an overview of the PA profession. The first portion of the course covers
the history of the PA profession, the role of the PA within the health care team, and an
overview of the laws, regulations and committees that provide oversight to the profession. The
second portion of the course focuses on health disparities, social determinants of health and
undeserved communities, and the role of the PA in the care of these populations. It includes
development of the awareness, knowledge, and skills needed in order to practice culturally
competent and sensitive health care.
72
Year 1, Q2: Winter
Clinical Therapeutics I
Practice of Medicine II
Principles of Clinical Medicine I
Foundations of Clinical Neurosciences
PAS 222: Clinical Therapeutics I
This course will provide a foundation for learning pharmacology and clinical
therapeutics/disease state management related to subjects covered in the Principles of Clinical
Medicine I course. The first segment will cover general pharmacokinetic/pharmacodynamic
principles and review drug-drug interaction principles. Disease state topics will include skin and
soft tissue infections, dermatological disorders, bone/joint disorders, and ENT conditions.
INDE 202: Practice of Medicine II
Medical interview and physical examination skills, information literacy, nutrition principles,
evidence-based practice, health policy, and population health are covered. At the end of this
quarter, students participate in a performance-based assessment of their medical interview and
physical examination skills. See INDE 201 for a complete description of the Practice of Medicine
course series.
PAS 212: Principles of Clinical Medicine I
This is the first course in a four-course sequence presenting organ-system-based physiology,
pathology, and pathophysiology. Each organ-specific block includes a review of the anatomy
and related histology, normal function of that organ system, how the organ system is affected
by and responds to disease, and how diseases of that organ system are treated. In PAS 212, the
focus is on the structure, function, disease, and corresponding therapeutics of several “primary
care” topics, particularly the musculoskeletal and dermatologic systems. In addition, basic
neurology, otorhinolaryngology, and ophthalmology will be covered.
PAS 202: Foundations of Clinical Neurosciences
Foundations of Clinical Neurosciences introduces students to the structure and function of the
nervous system, including neuroanatomy and neurophysiology. Applications to clinical
medicine and neurology are emphasized. Enrollment limited to Master of Science in Physician
Assistant Studies students.
Year 1, Q3: Spring
Clinical Therapeutics II
Practice of Medicine III
Principles of Clinical Medicine II
PAS 223: Clinical Therapeutics II
This course will provide a foundation for learning pharmacology and clinical
therapeutics/disease state management for cardiovascular and pulmonary diseases as covered
73
in the Principles of Clinical Medicine II course. Disease state topics will include asthma, COPD,
hypertension, hyperlipidemia, coronary artery disease, acute coronary syndrome, heart failure,
arrhythmias, fungal infections, and pneumonia.
INDE 203: Practice of Medicine III
Medical interview and physical examination skills, biomedical literature retrieval and appraisal,
nutrition principles, evidence-based practice, biomedical ethics, and population health are
covered. Students begin clinical problem-solving sessions to learn the approach to common and
important clinical problems. Cases integrate other course themes of population health,
evidence-based practice, clinical ethics, nutrition, health policy, and behavioral medicine.
Students begin to transition from comprehensive to problem-focused patient encounters.
Students also gain exposure to geriatrics, pediatrics, and interprofessional healthcare teams,
and practice mental health interview skills. At the end of this quarter, students participate in a
performance-based assessment of their medical interview and physical examination skills. See
INDE 201 for a complete description of the Practice of Medicine course series.
PAS 213: Principles of Clinical Medicine II
This is the second course in a four-course sequence presenting organ-system-based physiology,
pathology, and pathophysiology. Each organ-specific block includes a review of the anatomy
and related histology, normal function of that organ system, how the organ system is affected
by and responds to disease, and how diseases of that organ system are treated. In PAS 213, the
focus is on the structure, function, disease, and corresponding therapeutics of the pulmonary
and cardiovascular systems.
Year 2, Q4: Autumn
Clinical Therapeutics III
Practice of Medicine IV (A & B)
Principles of Clinical Medicine III
PAs in Healthcare II
PAS 224: Clinical Therapeutics III
This course will provide a foundation for learning pharmacology and clinical
therapeutics/disease state management for renal, endocrine, GI, and reproductive systems as
covered in the Principles of Clinical Medicine III course. Disease state topics will include renal
function and fluid/electrolytes, diabetes mellitus, osteoporosis, chronic kidney disease, end-
stage liver disease, thyroid disorders, contraception, viral hepatitis, GERD/PUD,
nausea/vomiting, constipation/diarrhea, clostridium difficile colitis, sexually transmitted
infections, HIV, men’s health, and menopause.
INDE 204: Practice of Medicine IV
The second year of the Practice of Medicine series (INDE 204 and 205) emphasizes clinical
reasoning, clinical practicum, and clinical procedures. Students continue clinical problem-
solving sessions to learn the approach to common and important clinical problems. Cases
74
integrate other course themes of population health, evidence-based practice, clinical ethics,
nutrition, health policy, and behavioral medicine. Students spend one half-day per week in a
clinical setting, practicing medical interview and physical examination skills, oral presentations,
and clinical note-writing under the mentorship of a clinical tutor. In the practicum, students
also gain experience with other practical aspects of patient care. The Clinical Procedures
segment introduces common and important procedures in clinical practice, including
phlebotomy, intravenous line insertion, and electrocardiography.
PAS 214: Principles of Clinical Medicine III
This is the third course in a four-course sequence presenting organ-system-based physiology,
pathology, and pathophysiology. Each organ-specific block includes a review of the anatomy
and related histology, normal function of that organ system, how the organ system is affected
by and responds to disease, and how diseases of that organ system are treated. In PAS 214, the
focus is on the structure, function, disease, and corresponding therapeutics of the
renal/genitourinary, gastrointestinal, endocrine, and both male and female reproductive
systems, with additional attention paid to women’s health.
PAS 292: PAs in Healthcare II
The PAs in Health Care II course provides an opportunity to learn advanced clinical skills such as
casting and splinting, advanced cardiac life support, and point of care ultrasound. In addition,
students will learn Telehealth skills and participate in reflections sessions.
Year 2, Q5: Winter
Clinical Therapeutics IV
Practice of Medicine V
Principles of Clinical Medicine IV
PAs in Health Care III: Clinical Transitions
PAS 225: Clinical Therapeutics IV
This course will provide a foundation for learning pharmacology and clinical therapeutics/
disease state management for neurologic, psychiatric, and hematologic conditions as covered in
the Principles of Clinical Medicine IV course. Disease state topics will include headache, stroke,
sleep disorders, delirium, Parkinson’s, venous thromboembolism, epilepsy, schizophrenia,
depression, bipolar disorder, ADHD, anxiety disorders, and chronic pain management. A
general overview of cancer drugs such as chemotherapies, antimetabolites, antitumor
antibiotics, and other anticancer drugs is also provided.
INDE 205: Practice of Medicine V
Continued emphasis on clinical reasoning, clinical practicum, and clinical procedures. Students
continue clinical problem-solving sessions to learn the approach to common and important
clinical problems. Cases integrate other course themes of population health, evidence-based
practice, clinical ethics, nutrition, health policy, and behavioral medicine. Students spend one
half-day per week in a clinical setting, practicing medical interview and physical examination
75
skills, oral presentations, and clinical note -writing under the mentorship of a clinical tutor. In
the practicum, students also gain experience with other practical aspects of patient care. For
the Clinical Procedures segment, students will have an opportunity to work in the Emergency
Department to practice performing procedures learned in the previous quarter. At the end of
this quarter, students participate in a comprehensive four-station, objective-structured clinical
examination (OSCE), which is a performance-based assessment of their medical interview,
physical examination, and clinical problem-solving skills.
PAS 215: Principles of Clinical Medicine IV
This is the fourth course in a four-course sequence presenting organ-system-based physiology,
pathology, and pathophysiology. Each organ-specific block includes a review of the anatomy
and related histology, normal function of that organ system, how the organ system is affected
by and responds to disease, and how diseases of that organ system are treated. In PAS 215, the
focus is on the structure, function, disease, and corresponding therapeutics of the neurologic
and hematologic systems, as well as autoimmune/rheumatologic and other multi-organ system
processes. We will discuss the diagnosis and management of psychiatric illness and review
important behavioral health topics.
PAS 293: PAs in Health Care III
The PAs in Health Care III course provides an opportunity to learn advanced clinical skills
including chest tube insertion, central line placement, intubation, and lumbar puncture.
Reflection sessions will also be included.
Year 2, Q6: Spring through Year 3, Q9: Winter:
PAs in Health Care IV: Leadership and Advocacy
Clerkships PAS 301-366 (see below, section 4.6)
PAS 294: PAs in Health Care IV: Leadership and Advocacy
The final course in the PAs in Health Care series will provide students with the skills necessary
for transition from PA student to practicing PA and will continue to expand on leadership skills.
One portion of the course will focus on preparation from the transition to clinical practice,
which will include requirements for licensure and certification, medical liability, billing and
coding, and ethics. Other threads will consist of lectures on advanced and novel topics in
medicine; lectures and reflections with CARE (student/patient wellness); and development of
leadership skills and advocacy.
76
4.6. CALENDAR OF CLERKSHIP PERIODS
*These period timeframes and numbers are subject to change and will be confirmed as we get
closer to clerkships.
AY 2023-2024 Clerkship Periods
Summer
Period 1 July 3 - July 27, 2023
Period 2 July 31 - August 24, 2023
Period 3 August 28 - September 21, 2023
Autumn
Period 4 September 25 - October 19, 2023
Period 5 October 23 - November 16, 2023
Period 6 November 20 – December 14, 2023
Holiday Break: December 14, 2022 - January 7, 2024
Winter
Period 7 January 8 - February 1, 2024
Period 8 February 5 – February 29, 2024
Period 9 March 4 – March 21, 2024
Spring Break March 25 - March 29, 2024
Spring
Period 10 April 1 - April 26, 2024
Period 11 April 29 – May 24, 2024
Period 12 May 27 – June 21, 2024
Summer Break June 24 – June 28, 2024
for MSPA Program

77
4.7. CLERKSHIP REQUIREMENTS
Students must have successfully completed all pre-clerkship courses prior to beginning
clerkships. Each student is expected to complete clinical rotations in medically underserved
areas/health professional shortage areas, but there is no maximum number of such rotations.
Students are expected to provide their own transportation to clinical sites. Lodging and travel
expense support is grant-dependent and only provided for sites outside the Bay Area. Certain
rotations in the East Bay are eligible for housing, assuming continued availability. All core
clerkship rotations will occur at MSPA core sites, without exception.
Clerkship #
Title
Units
PAS 303
Family Medicine/Primary Care
6 (4 weeks)
PAS 304
Family Medicine/Primary Care
6 (4 weeks)
PAS 301
Internal Medicine
6 (4 weeks)
PAS 302
Internal Medicine
6 (4 weeks)
PAS 336
Behavioral Medicine/Mental Health
6 (4 weeks)
PAS 311
Pediatrics
6 (4 weeks)
PAS 331
Women’s Health (prenatal and gynecologic care)
6 (4 weeks)
PAS 321
Emergency Medicine
6 (4 weeks)
PAS 320
Surgery
6 (4 weeks)
PAS 351
Elective I
6 (4 weeks)
PAS 352
Elective II
6 (4 weeks)
PAS 353
Elective III
6 (3 weeks)
Clinical sites and preceptors for core clerkships will be provided by the clerkship leadership
team. Students are not required to solicit clinical sites or preceptors. Students may not suggest
sites or preceptors for core clerkships.
4.8. ELECTIVE CLERKSHIPS
Students will have the opportunity to complete 3 electives, which will be selected from a
designated list. Qualifying clerkships are approved by the clerkship leadership team and may be
removed from the list of approved clerkships at any time. Additions to the approved list of
clerkships take effect immediately for all students; deletions from the list take effect for the
students who begin clerkships in the subsequent clerkship year.
Clinical sites and preceptors for elective clerkships will be provided by the clerkship leadership
team. Students are not required to solicit clinical sites or preceptors. Students may suggest
sites or preceptors for elective rotations, but are not required to do so. Student-suggested
elective sites and preceptors will be reviewed and evaluated by the Program for educational
suitability, but placement is not guaranteed. Housing and transportation stipends are typically
not provided for elective rotations.
78
4.9. ABSENCES DURING CLERKSHIPS
Students must contact the Clerkship leadership team to obtain explicit advance approval for
any planned absence from the clerkship. Unanticipated absences for illness or emergency
must be communicated to the Clerkship leadership team as promptly as possible.
Students are expected to seek necessary health care to maintain their physical and mental
well-being. Examples of necessary health care include preventive health services and screening
(e.g., annual check-ups, routine dental cleaning, and vaccinations), new and follow-up visits for
acute illness, ongoing care for chronic illnesses, physical therapy, and counseling and
psychological services. Consistent with University policies and the law, students have a right to
privacy when seeking care.
Students may attend recurring medical or dental appointments during core clerkships.
Clerkship leadership team/s, site director/s, and preceptor/s or patient care teams (depending
on the service) must be notified in advance of these planned absences to coordinate time
away from the clerkship. Clerkship students have a right to privacy when seeking care and
need not disclose the specific type of healthcare that is being sought. A student’s decision to
seek healthcare during a clerkship will be managed so as to have no impact on his or her
performance evaluation. Any questions or concerns may be addressed to the Clerkship
leadership team by email, phone, or in person.
Students who are absent more than two days (10%) during a four-week rotation for any
reason will be required to make up missed time.
Students who will miss more than 20% of the total duration of a clerkship – for any reason –
will be required to make up the missed time or reschedule the clerkship per the discretion of
the Director of Clerkship Education.
Failure to communicate with the clerkship leadership team about unavoidable absences is a
professionalism issue. As a result, a student’s Faculty Advisor will be notified. The student will
receive feedback regarding professionalism expectations and a warning that any further issues
with communication may result in a referral to the Student Progress Committee. In addition,
failure to communicate with the clerkship team regarding absences can be a potential reason
for failing the clerkship.

79
4.10. CLINICAL PERFORMANCE EXAMS
Demonstration of at least minimum competency on the clinical performance exams, CPX-P and
APSA, within 4 months of program completion is a requirement for graduation. These exams
take place during students’ final winter quarter.
The Clinical Performance Examination for MSPA students (CPX-P) is a comprehensive
examination consisting of both standardized patient encounters and computer-based exercises.
The goals of this assessment are to evaluate students’ history and physical examination skills,
patient interaction skills, clinical reasoning, and overall medical knowledge.
During the CPX-P, students see a series of patients with a broad range of clinical problems.
Students are expected to perform a focused history and physical examination, and are also
expected to communicate their thinking and preliminary plans to the patients. Students also
complete computer-based exercises designed to assess medical knowledge and clinical
reasoning.
Students must demonstrate at least minimum competency in each of three primary skill areas:
• History and physical examination
• Communication skills
• Clinical reasoning
Students must also attain an overall passing score on the Applied Procedural Skills Assessment
(APSA). Students must demonstrate at least minimum competency in each of the following skill
areas:
• Sterile technique
• Local anesthesia administration (subcutaneous route)
• Suturing
• Intramuscular injection
• Billing and coding the patient encounter
For either exam, students who do not attain an overall passing score, or who fail individual skill
domains, will be required to successfully complete a remediation program, including
individualized feedback, self-reflection, and working with a faculty mentor in the School of
Medicine to develop the skills necessary for improvement. Students will have one opportunity
to retake the exam for a passing score.
80
5.0. ASSESSMENT OF STUDENT ACADEMIC PERFORMANCE
5.1. HEALTH PROVIDER INVOLVEMENT IN STUDENT ASSESSMENT
A student may not be formally evaluated by a health professional who has provided medical or
mental health services to that student. This applies to one-time/episodic care as well as
continuing care. A student may also not be evaluated by a family member. The MSPA program
Principal or Instructional Faculty, the Program Director, Associate Program Director, Associate
Medical Director or the Medical Director are not allowed to provide medical care to students
unless it is an emergency.
5.2. EVALUATION OF PERFORMANCE IN COURSES
All pre-clerkship PA program courses are graded on a pass/fail basis. It is the prerogative of
each course director to determine the best method for assessing student performance for their
course. Learning activities such as quizzes, short papers, laboratory exercises, problem sets,
presentations, and group discussions may be offered on a graded or ungraded basis at the
discretion of the course director. Attendance and participation are essential to mastery of
material and is expected of all students. Course directors are expected to announce criteria for
passing a course by the end of the second week of the quarter.
Grading System
The following grading system is used to report on the official transcript the performance of
students in all courses and clerkships taken while an MSPA Studies degree candidate:
Pass (+) indicates that a student has demonstrated to the satisfaction of the course
director that they have mastered the material taught in the course.
Incomplete (I) indicates that extenuating medical or personal circumstances beyond the
student’s control have prevented completion of course requirements. An Incomplete can
be corrected in a manner specified by the course director and must be corrected within
one year (unless the Student Progress Committee specifies an earlier date). When a
student takes a final or makeup examination following an Incomplete, it becomes a Pass
or Fail. If the student does not attempt to correct the Incomplete within the agreed-upon
time, it becomes a Fail.
Continuing (N) indicates that the course has not concluded and that the student is
continuing the course, or that a minor component of the course (as defined by the
course director) is pending.
81
Grade Not Reported (GNR) indicates that a grade has not been reported by the
instructor.
Fail (-) indicates that a student has not met the minimum performance standards for the
course. The student must achieve a passing grade within one year of the failure or prior
to beginning clerkships, whichever is sooner.
A student may not receive credit for repeating a course unless the content has changed
significantly, as determined by the course director.
In addition to these transcript-related grades, an additional designation is used for the Practice
of Medicine course series to report on academic progress:
Marginal Pass (MP) indicates that a student has fallen short of meeting minimal
performance standards for a Pass but has done better than a Fail at the end of the
academic quarter, and that additional work or remediation is necessary to achieve a
Pass.
End-Quarter Policy Statement
The End-Quarter Period, also known as “Dead Week”, is a time of reduced social and
extracurricular activity preceding final examinations. Its purpose is to permit students to
concentrate on academic work and to prepare for final examinations.
During the End-Quarter Period, classes are regularly scheduled and assignments made; this
regular class time is used by instructors in whatever way seems best suited to the completion
and summation of course material. Instructors should neither make extraordinary assignments
nor announce additional course meetings in order to “catch up” in course presentations that
have fallen behind. They are free, however, and even encouraged to conduct optional review
sessions and to suggest other activities that might seem appropriate for students preparing for
final examinations.
Students are expected to remain on campus during the End-Quarter Period and should avoid
planning activities that might conflict with course commitments and final exam preparation
during this week.
No graded homework assignments, mandatory quizzes, or examinations should be given during
the End-Quarter Period except:
1. In classes for which graded homework assignments or quizzes are routine parts of the
instruction process.
2. In classes with laboratories where the final examination will not test the laboratory
component. In such a case, the laboratory session(s) during the End-Quarter Period
may be used to examine students on that aspect of the course.
82
3. In Practice of Medicine, in which previously scheduled standardized patient (SP)
assessments are permitted during the End-Quarter Period.
Major papers or projects about which the student has had reasonable notice may be called due
in the End-Quarter Period. Take-home final examinations, given in place of the officially
scheduled in-class examination, may be distributed in the End-Quarter Period. Although the
instructor may ask students to return take-home examinations early in the final examination
period, the instructor may not call them due until the end of the regularly scheduled
examination time for that course. Such a policy respects the principle that students’ final
examinations are to be scheduled over a period of several days.
Final Examinations
Final examinations are scheduled by the Office of PA Education in collaboration with the Office
of Medical Education when appropriate. Tentative dates and times are posted by the end of
the previous quarter and final schedules are posted by the end of the second week of the
quarter. Students anticipating conflicts in examination schedules should seek to resolve them
with course instructors.
Students are expected to remain on campus during the final exam period and should not book
travel or other plans until they have confirmed the dates that they must sit for their final
exams. Final exams should take priority over other commitments and students are advised to
plan accordingly.
Final examinations are governed by the regulations below:
1. Students are expected to take the final examination unless, at least 24 hours prior to the
examination, they have received formal written approval for obtaining an Incomplete
from their faculty advisor. Incompletes are given for significant personal or medical
reasons beyond the student’s control. If a student does not appear for the examination
and has not been granted an Incomplete, the student will receive a Fail.
2. Students are expected to report for their examinations at the time and place designated
by the Office of PA Education, the Office of Medical Education, or the course director,
unless the course director has made alternative arrangements. While examinations are
not “proctored” as such, students must take the examination in the designated location
within the prescribed examination time. Students are expected to adhere to the Stanford
Honor Code at all times during examinations.
3. When the final examination or its appropriate substitute is not an in-class examination
(e.g., when an instructor assigns a take-home examination, paper, or project in lieu of an
in-class examination), the schedule and format of the final examination or its substitute
will be determined no later than the end of the second week of the quarter and, if
changed subsequently, a modification must be approved by a majority of the students in
the class.

83
4. Students with documented disabilities who have registered with and been recommended
by the Office of Accessible Education (OAE, https://oae.stanford.edu) to receive special
examination accommodations are responsible for notifying both the Office of PA
Education and their course directors at the beginning of each quarter, or as soon as they
receive their accommodation letter, that they will need these accommodations. Unless
students receive accommodations mid-quarter, they must let the Office of PA Education
and their course directors know of their accommodations needs no later than the end of
the second week of the quarter for which they are receiving accommodations. Reminder:
students needing exam accommodations are to contact the OAE first, prior to notifying
their course director(s).
5. Feedback on written examinations is to be as complete as practicable. Students have the
right to see their final examination and discuss it with a faculty member.
Correction of Deficiencies in Pre-Clerkship Courses
Students who fail a pre-clerkship course must achieve a passing grade within one year of the
failure or prior to beginning clerkships, whichever is sooner. If this cannot be achieved through
remediation (as determined by the course director) then the student must retake and pass the
course when it is next offered. Only the Student Progress Committee has the power to change
this requirement. The requirements for achieving a passing grade are determined by the
responsible faculty. Students with a failing grade will be counseled by their faculty advisor and
reviewed by the Student Progress Committee.
Academic deficiencies in pre-clerkship courses must be rectified prior to the beginning of
clerkships or by a date specified by the Student Progress Committee (which has the power, in
an appropriate case, to modify any of the requirements in this subsection).
Course directors are encouraged to provide educational assistance to students failing required
courses in a timely manner. For first-year students, this includes more intensive assistance
during the first summer quarter following receipt of a failing grade, and review of such students
prior to autumn quarter registration. Students failing courses on the autumn and winter
quarter grids for the second year must correct these deficiencies prior to beginning clerkships.
Students who receive an Incomplete grade because of extenuating medical or personal
circumstances must correct the incomplete grade within one (1) year or prior to entering
clerkships, whichever comes first, in a manner specified by the course director. Courses such as
those in the Practice of Medicine sequence, where hands-on activities and small group
interactions constitute a significant portion of the course, may require retaking of the course
the following year.
Due to the structure of the MSPA didactic curriculum, failure to meet the passing criteria for a
course in a timely fashion may result in deceleration.
84
Evaluation of Performance in Practice of Medicine
Grading
Students receive a Pass (+), Continuing (N), Marginal Pass (MP), Fail (-), or Incomplete (I) grade
after each quarter. The grade is based on completion of quarter course requirements,
satisfactory performance on end-of-quarter assessments, and professional behavior. The
following are the guidelines for each grade option in the course:
Pass (+): Students have completed all course requirements, performed satisfactorily on the
final Standardized Patient assessment and each section of the written final examination,
and exhibited professional behavior in the course.
Continuing (N): Students have not completed all course requirements and/or did not
perform satisfactorily on any individual section of the written final examination.
Marginal Pass (MP): Students have not performed satisfactorily on the final Standardized
Patient assessment and/or the overall written final examination; there may be some
concern about the student’s professional behavior in the course; and/or the student’s
performance in in-class activities has raised some concerns about knowledge and
competence.
Fail (-): Students have performed poorly on the final Standardized Patient assessment
and/or the overall written final examination (using the criteria above for N Grade or
Marginal Pass); there may be serious concerns about the student’s professional behavior in
the course; and/or the student’s performance in in-class activities has raised serious
concerns about knowledge and competence.
Incomplete (I): Student has satisfactorily completed a substantial part (but not all) of the
coursework. Students must request an Incomplete grade by the last class meeting.
Incomplete grades must be made up within one (1) year, or prior to entering clerkships,
whichever comes first.
The Student Progress Committee will be notified of all grades of Continuing (N), Marginal Pass
(MP), or Fail (-).
Students who do not perform satisfactorily on either the final Standardized Patient assessment
and/or the written final examination must complete a plan of remediation tailored to student
needs and course resources. Students who do not satisfactorily complete this plan of
remediation will earn a Fail for the course.
Policy for Missed Assessments
Every student is expected to be present for each final Standardized Patient assessment and
each end-quarter integrated examination in the Practice of Medicine course.
85
A formal course director's excuse is required to make up any missed course examination. It is
recommended that students meet with their faculty advisors prior to submitting a formal
request for any missed course examination.
A Course Director's excuse may be issued before a regularly scheduled assessment or
examination to accommodate some essential extracurricular event or after an examination in
the case of illness.
A score of zero will be credited towards a student’s final score if an assessment or examination
is missed without a course director’s excuse.
If a course director's excuse is issued before a regularly scheduled assessment or examination
to accommodate some essential extracurricular event, the student will be expected to take the
scheduled make-up examination or assessment at Stanford. If the course director's excuse
extends beyond the make-up date because of some essential activity away from Stanford, then
appropriate arrangements will be made within the resources of the course. Failure to make
such an arrangement will result in a score of zero on that exam. A student who misses an
assessment or examination with a course director's excuse for illness should contact the POM
course coordinator and appropriate arrangements will be made.
Policy for Remediation of a Continuing, Marginal Pass, or Fail Grade in POM
A student who receives a Continuing (N) in any quarter of the POM series (INDE 201-205) must
complete outstanding course requirements to correct the grade to a Pass (+). The student will
be allowed to continue through the POM sequence. The Student Progress Committee will be
notified. Students who do not satisfactorily complete this plan of remediation will earn a
Marginal Pass (MP) grade for the course.
A student who receives a Marginal Pass (MP) in any quarter of the POM series (INDE 201-205)
must successfully complete a course of remediation tailored to student needs and course
resources to correct the grade to a Pass (+). The student will not be allowed to continue
through the POM sequence unless provided special permission from the course director. The
Student Progress Committee will be notified. Students who do not satisfactorily complete this
plan of remediation will not be allowed to continue to clerkships.
A student who receives a Fail in any quarter of the POM series (INDE 201-205) will be required
to re-take that quarter the following year, including all required exercises and examinations.
The student will not be allowed to continue through the POM sequence, unless provided
special permission from the course director. The Student Progress Committee will be notified.

86
5.3. EXAM POLICY FOR REQUIRED PRE-CLERKSHIP COURSES
Per the Stanford University Honor Code (https://communitystandards.stanford.edu/policies-
guidance/honor-code), individual faculty members are not present to proctor exams; however,
they can determine the best exam environment for their tests and make any requirements they
see fit with regard to how students take the exam. The Honor Code states in part: “The faculty
on its part manifests its confidence in the honor of its students by refraining from proctoring
examinations and from taking unusual and unreasonable precautions to prevent the forms of
dishonesty mentioned above. The faculty will also avoid, as far as practicable, academic
procedures that create temptations to violate the Honor Code.”
To uphold the spirit of the University’s Honor Code and to create consistency across courses in
the pre-clerkship curriculum, the Office of PA Education and the Office of Medical Education
provide the following guidelines for closed-book examination environments in our required
courses:
• Students will complete exams in the rooms assigned by the course.
• Exams are non-collaborative and, unless otherwise noted by course faculty, closed book.
• Unless otherwise stipulated by the course director, use of any electronic device to access
other resources, including (but not limited to) the internet, notes, and colleagues, is
expressly forbidden and constitutes a violation of the Stanford Honor Code.
• The use of personal listening devices is expressly forbidden in the exam setting.
• Students with disabilities or other special needs for which they may require
accommodations should notify the MSPA Student Life Officer well in advance to receive
appropriate accommodation for exams. Once students receive an official accommodations
letter, they must let the MSPA Student Life Officer and their course directors know of their
accommodations request no later than the end of the second week of the quarter, in every
quarter in which they are requesting accommodations.
• Please see Section 3.12, Policies and Resources for Mobile Devices, for more information
about BYOD policies governing final exams.
87
5.4. EVALUATION OF PERFORMANCE IN CLINICAL CLERKSHIPS
Students in clerkships may earn a final grade of Pass or Fail. Final grades are comprised of
performance on the preceptor evaluation, completion of the student evaluation of the
preceptor, completion of patient logging, completion of Aquifer modules as applicable, and
other items outlined in the syllabus, along with performance on the End of Rotation Exams.
Clerkship Performance Evaluation Appeals
Students who have questions or concerns about a performance evaluation in a clinical clerkship
should contact the Clerkship leadership team or their faculty advisor to request a review. If a
student’s disagreement remains unresolved, the student or his or her faculty advisor may
request a review by the Student Progress Committee by contacting one of the Chairs of the
Student Progress Committee. A written request for a review must be received within eight
weeks of the date that the final student performance evaluation was submitted.
Upon receiving a request for review, the Student Progress Committee will notify the clerkship
team responsible for the performance evaluation and will gather data from the student and the
clerkship team. The Student Progress Committee will review the final evaluation and all
submitted data, gather additional information as needed, and will generally, though it is not
required, reach a decision by consensus. The student and the clerkship team will be notified in
writing of the final decision. The Student Progress Committee will attempt to complete each
appeal within 45 days of the request. The Student Progress Committee’s decision is considered
final. Students with further concerns may choose to pursue the Stanford University student
academic grievance procedure, though they should recognize the limited scope of review
inherent in that procedure.
Correction of Deficiencies in Clerkships
During the course of a clerkship, when the Clerkship leadership team becomes aware that a
student’s performance may warrant a grade of Fail, they must notify the student promptly that,
in the absence of improvement, a non-passing grade is being considered. Once the Clerkship
leadership team confirms the decision to assign a non-passing grade, they will immediately
notify the student about the final grade to be assigned. The Clerkship leadership team will also
notify the student’s faculty advisor, who will arrange a meeting with the student.
Requirements for correcting a Fail will be determined by the Clerkship leadership team.
Students who receive a Fail grade are required to meet with the Clerkship leadership team to
set timely requirements for achieving an unqualified passing grade. Non-passing grades in
clerkships, including N or “continuing” grades, must be corrected within one year of completing
the clerkship. Students failing to correct a non-passing grade within one year will be reviewed
and discussed by the Student Progress Committee.
Students cannot receive a Stanford MS in PA Studies degree with an uncorrected incomplete or
Fail in a clerkship.

88
5.5. STANDARDIZED PATIENT TEACHING AND ASSESSMENT
The Standardized Patient (SP) Program offers clinical skills training for PA students throughout
the three-year curriculum. Its activities are designed to provide a simulated setting for the
instruction and assessment of the clinical, cross-cultural and interpersonal skills of PA students.
Real patients or SPs are trained to consistently recreate the same clinical situation, findings, or
problem with each student encounter. For more information about the Standardized Patient
Program, go to: http://cisl.stanford.edu/standardized-patient-program.html
89
6.0. STUDENT PROGRESS COMMITTEE (SPC)
6.1. INTRODUCTION
The Student Progress Committee (SPC) is a standing committee of the Stanford School of
Medicine’s Office of PA Education. The purpose of the Student Progress Committee is to
provide all PA students with periodic and systematic reviews of their overall progress towards
completion of the MS in PA Studies degree, as well as reviews on an as-needed basis, and to
monitor student development and provide guidance and recommendations as appropriate.
The Stanford School of Medicine has an obligation to evaluate the performance of each student
on an ongoing basis from matriculation until graduation and to endorse each student as being
suitable to meet the academic, professional, and technical standards for the practice of
medicine. It is therefore the responsibility of the faculty—through this Committee—to review
any concerns regarding the ongoing satisfactory fulfillment of these standards.
A. Membership:
The Student Progress Committee is composed of MSPA program faculty and may include
Stanford community Advanced Practice Providers. All Student Progress Committee
members are voting members, except in cases where a faculty member is the faculty
advisor or mentor for the student under review. A total of three voting members is
required for a quorum. A quorum of voting members of the Student Progress Committee
is required to be in attendance (either physically or virtually) for decision-making
activities. Ex officio non-voting committee members may include (but are not limited to)
the Associate Dean for PA Education, MSPA program Medical Directors, and School of
Medicine leadership.
B. General Responsibilities and Definitions:
1. Responsibilities: The primary responsibility of the Committee is to review the
development and performance of each student on an ongoing basis in the areas of
the fulfillment of academic, technical, and professional standards. This includes:
a. Evaluation of achievement of all requirements for promotion.
b. Identification of students not meeting requirements and/or expectations for
academic, professionalism, or technical performance, and recommendation of
individualized learning plans that support academic and professional
development;
c. Evaluation of achievement of required remediation;
d. Recommending taking such action (including deceleration and/or dismissal from
the Stanford School of Medicine MSPA program) as the Student Progress
Committee deems appropriate given the facts and circumstances.
2. The Student Progress Committee typically meets once monthly. The Chair(s) may call
additional meetings if necessary.
90
3. Except for the Student Progress Committee Chair(s), the faculty advisors, the
Associate Dean for Medical Education, the MSPA Medical Directors, and other
members of the Committee will not discuss decisions or pending actions with
students and may not be approached by students with inquiries.
4. The Student Progress Committee may also consider student petitions on various
matters, including, for example: an extension of PA education beyond three years;
leaves of absence that either individually or cumulatively exceed a total of one year;
reinstatement.
5. Satisfactory Academic Performance: Satisfactory academic performance and progress
are defined as:
a. Obtaining a “pass” on all required assignments and projects in a timely fashion.
It is the responsibility of any student who is underperforming to seek the
assistance of the course director and their advisor.
b. Demonstrating clinical competence commensurate with the level of training
required in the Program. Clinical competence includes, but is not limited to:
clinical judgment, technical and psychomotor skills, interpersonal skills and
attitudes, and professional comportment.
C. Student Progress Committee (SPC) Procedures and Actions
1. Referral to SPC: The didactic and clinical phases of the program have distinct policies
and procedures related to remediation. Referral to SPC may also be required for
matters outside of a course or clinical rotation, e.g., professionalism.
a. Didactic Phase: A student who fails a didactic course will be referred to SPC and
will receive a formal written plan for remediation, including deliverables and
timelines. Failure to meet the expectations of the remediation plan can result in
consequences up to and including deceleration or dismissal.
b. Clinical Phase: A student who fails a clerkship or fails to pass 2 or more EoR
exams will be referred to SPC for review and will receive a formal written plan
for remediation, including deliverables and timelines. Failure to meet the
expectations of the remediation plan can result in consequences up to and
including deceleration or dismissal.
c. Professionalism: A student can be referred to SPC by faculty or staff for
unprofessional behavior. After review of the behavior, SPC may recommend a
formal plan for remediation, including deliverables and timelines. Failure to meet
the expectations of the remediation plan can result in consequences up to and
including deceleration or dismissal.
2. Academic Performance and Progression: Student grades, academic integrity,
professionalism, and ability to meet the technical standards are factors considered in
student progression. Each student must meet all these program requirements. Each
91
student is assigned a member of the faculty as their Faculty Advisor. The role of the
Faculty Advisor is to monitor student progress in the Program and to serve as the
student's academic mentor, guide and advocate. Each student is encouraged to meet
with their Faculty Advisor at a minimum of once every quarter. However, when an
academic or professionalism issue arises, students are encouraged to consult with
their Faculty Advisor.
a. Satisfactory Academic Performance: Satisfactory academic performance and
progress are defined as:
i. Obtaining a “pass” on all required assignments and projects in a timely fashion.
It is the responsibility of any student who is underperforming to seek the
assistance of the course director and their advisor.
ii. Demonstrating clinical competence commensurate with the level of training
required in the Program. Clinical competence includes, but is not limited to:
clinical judgment, technical and psychomotor skills, interpersonal skills and
attitudes, and professional comportment.
b. Academic Progression: At the end of each quarter, and as needed, the SPC will
review the academic and professionalism records of each PA student and take
action as necessary.
Due to the structure of the MSPA didactic curriculum, failure to meet the passing
criteria for a course may result in deceleration.
3. Reassessment: Reassessment may be required to facilitate academic progression.
The academic and clinical phases of the program have distinct policies and
procedures related to reassessment:
a. Didactic Phase: Over the course of the first five (5) quarters, or the didactic
phase of the program, a student who does not meet the passing criteria on a
block or final exam will have an opportunity to retake the exam for a passing
grade. The course director will inform the student of their options related to
retaking the failed assessment(s). The exam must be retaken within 14 days of
the initial exam. A student can have a maximum of two (2) failed assessments
during the didactic phase before being referred to the SPC for review.
b. Clinical Phase: Students have the opportunity to retake a failed EoR exam once in
any given specialty during the clinical year. Failure of any two exams (back-to-
back or not) will result in referral to the SPC.
c. Summative Exam: A student who does not meet the passing criteria for the
summative exam will have an opportunity to retake the exam for a passing
grade. The second exam should be taken 2 months after the initial exam.
4. Remediation Process: Remediation may be required to facilitate progression in the
MSPA program.
a. When a student requiring academic or professionalism remediation has been
identified, the student is referred to the SPC. It is the responsibility of the SPC to
identify the area(s) of greatest need and determine how the student will
demonstrate that they have successfully remediated the deficiency.
92
b. When the SPC needs to meet with a student, the student will be notified via
email by the SPC Chair(s) or designee to meet with the SPC to discuss their
academic standing and/or professional behavior.
c. The student must confirm, via email, receipt of the invitation to meet within two
(2) calendar days. Failure to respond in a timely manner may impact the
student’s professionalism evaluation.
d. After meeting with the student, the SPC will determine if further action is
necessary. If so, the SPC will develop a formal remediation plan with timelines
and deliverables.
e. The SPC will present their recommendations in writing to the Program Director
within two (2) business days. The Program Director will review the SPC
recommended action(s), make the final determination of recommended
action(s), and the Program Director or SPC designee will communicate the final
decision/outcome to the student.
f. Possible recommended actions may include, but are not limited to: no further
action; remediation; deceleration; or dismissal. With the exception of “no
further action” and “remediation”, the Program Director will review the SPC
recommended action(s), make the final determination of recommended
action(s), and the Program Director or SPC designee will communicate the final
decision/outcome to the student.
g. The SPC monitors student progress to completion. Upon successful remediation
of the academic or professionalism deficiency, the SPC designee will inform the
SPC that the deficiency is resolved.
5. Deceleration: The SPC may recommend deceleration for a student under several
circumstances, including the inability to remediate a failed course or in the event
that a leave of absence interferes with the ability to progress in the didactic
curriculum. As an example, if a student missed their 2
nd
quarter due to a leave of
absence, they would not be able to start the 3
rd
quarter until they received a passing
score for all Quarter 2 classes. In this event, the student would be required to
decelerate and take the 2
nd
quarter courses the following year. Once a student
decelerates, they will officially re-enroll where they left off, but it is recommended
that they audit courses they have already successfully completed. A student may
also request deceleration for personal reasons. The final decision regarding
deceleration is made by the Program Director.
6. Promotion: The SPC will review each student prior to advancement to clerkship. A
student will be promoted to the clinical phase when all of the following conditions
have been met:
a. All didactic coursework in the MSPA Program curriculum has been completed
with a designation of “Pass”;
b. Student Health Clearance, including documentation of immunizations and
annual TB screening and influenza vaccination, is completed;

93
c. Successful completion of Health Insurance Portability and Accountability Act
(HIPAA) training;
d. Successful completion of all competency skills (e.g., BLS, ACLS, etc.) with an
expiration date that surpasses the date of program completion;
e. Verification that they meet the Technical Standards;
f. Successful completion of a background check.
Students who are determined by the SPC as not fulfilling the standards for promotion
to the clinical phase, or who do not satisfy the remediation measures required by the
SPC, may be recommended by SPC for dismissal from the MSPA Program. Students
who do not achieve successful promotion to the clinical phase cannot continue as
MSPA candidates.
7. Dismissal: After due consideration and process, Stanford University reserves the
right to require the dismissal of any student at any time before graduation if
circumstances of a legal, moral, behavioral, ethical, patient safety, health or
academic nature justify such an action.
A student may be dismissed from the Program for any of the following:
• Not successfully correcting a failing grade in a pre-clerkship course.
• Not successfully correcting a failing grade in a clinical clerkship.
• Professionalism violations.
• Failing to complete Thesis project and presentation.
• Inability to fulfill the Technical Standards.
Decisions regarding dismissal are made on an individual basis after considering all
pertinent circumstances and extenuating circumstances relating to the case. The
SPC’s recommendations are presented to the Program Director for review. The
Program Director may agree, amend, or disagree with the SPC recommendation. The
Program Director will issue a letter of decision to the student regarding their status
in the program. If the Program Director agrees with the SPC recommendation, the
dismissal is immediately effective upon receipt of the letter of notification from the
Program Director, or as otherwise provided in the letter. Students may appeal a
dismissal decision as stated in Section 6.4 of this handbook.
94
6.2. STANDARDS FOR PERFORMANCE AND SATISFACTORY PROGRESS
In order to make satisfactory progress towards the MS in PA Studies degree, each student must
satisfy academic, professional, and technical standards on an ongoing basis.
A. Academic: Students are required to make Satisfactory Academic Progress (SAP) in terms
of units taken and passed, courses and clerkships successfully completed, timely
completion of other requirements, and correction of deficiencies.
1. Units
a. Students must take and successfully complete a minimum per-quarter number of
units, which are as follows:
(i) Quarter 1 (Autumn): 26 units
(ii) Quarter 2 (Winter): 17 units
(iii) Quarter 3 (Spring): 18 units
(iv) Quarter 4 (Autumn): 25 units
(v) Quarter 5 (Winter): 20 units
(vi) Quarter 6 (Spring): 19 units
(vii) Quarter 7 (Summer): 19 units
(viii) Quarter 8 (Autumn): 19 units
(ix) Quarter 9 (Winter): 19 units
Students must complete all didactic courses with a passing (+) grade to transition to the
clerkship year.
NOTE: Unit requirements for financial aid eligibility are not necessarily the same as for
satisfactory academic progress for graduation. Students should also refer to
financial aid policy, and consult with the University Financial Aid Office.
2. Number of Years
a. If a student plans to take more than 9 consecutive quarters to complete his/her
degree, exclusive of time spent during an approved Leave of Absence, the
student must petition for and receive approval by the Student Progress
Committee. The student’s petition must provide reasons for the requested
extension and submit specific plans for completing the degree, all of which is
subject to review and approval by the student’s faculty advisor.
b. Stanford University requires all master’s degrees to be completed within three
years of matriculation. Any extension beyond three years requires approval by
the Committee on Graduate Studies.
3. Leadership Track and Thesis Project
Students must make satisfactory progress in meeting Thesis/Capstone work
requirements, as outlined in Section 4.4 of this handbook.
95
4. Examinations
Students must make satisfactory progress in meeting examination requirements,
including the clinical clerkship End of Rotation exams and summative exams (End of
Curriculum exam, APSA, and CPX-P).
5. Academic Deficiencies
a. All academic deficiencies must be corrected within one year (or otherwise within
a time limit specifically set by the Student Progress Committee in the individual
case). Pre-clerkship deficiencies must be corrected before promotion to
clerkship.
b. Note that some deficiencies may be considered to be unable to be remediated
and may result in immediate dismissal. Such circumstances may include (but are
not limited to) when one or more of the following conditions apply:
(i) Failure of two clinical clerkships
(ii) Failure of 3 or more pre-clerkship courses in any given academic year or
over the course of the pre-clerkship curriculum (remediated or not)
(iii) Failures in 3 or more courses during the program (pre-clerkship, clerkship
or a combination of both, whether remediated or not)
c. A student’s failure to attend required meetings, comply with Student Progress
Committee directives for remediation, or meet Student Progress Committee
deadlines may preclude remediation and result in immediate dismissal from the
Stanford MSPA program.
B. Professionalism: Students are required, on an ongoing basis, to satisfy professionalism
standards as outlined in Section 2.4 of this handbook. A serious breach of professionalism
may result in immediate dismissal from the MSPA program.
C. Technical Standards: Students are required, on an ongoing basis, to satisfy technical
standards as outlined in Section 2.3 of this handbook. Continued fulfillment of such
standards is a requirement for ongoing registration in the Stanford School of Medicine.
96
6.3. PROMOTION
The Student Progress Committee will conduct a systematic review of all students’ progress
towards completion of the MS in PA Studies degree. Those reviews will encompass all areas of
academic performance, professionalism, and technical standards. Students whom the Student
Progress Committee determines have met these standards will be eligible for formal promotion
as follows:
A. Promotion to MSPA Clinical Student: upon completion of pre-clerkship courses and other
requirements, students will be reviewed for formal promotion. Criteria for promotion are:
1. Satisfactory completion of all required pre-clerkship courses with a passing grade by
the beginning of the spring quarter. MSPA Studies students may be required to take
additional preparatory clinical courses prior to entering clerkships.
2. Satisfactory fulfillment of the standards for professionalism of the Stanford School of
Medicine MSPA program.
3. Satisfactory fulfillment of the technical standards of the Stanford School of Medicine
MSPA program.
4. Satisfactory progress in scholarly work.
Students who are determined by the Student Progress Committee to not be fulfilling the
standards for promotion to MSPA Clinical Student, or who do not satisfy the remediation
measures required by the Student Progress Committee, may be considered by SPC for
dismissal from the MSPA program or deceleration. Students who do not achieve
successful promotion to MSPA Clinical Student cannot continue as MS in PA Studies
candidates at the Stanford School of Medicine.
B. Promotion to Eligible for MS in PA Studies Degree: In March of the anticipated year of
graduation, the Student Progress Committee will review students’ progress to determine
their eligibility for promotion to “eligible for MS in PA Studies degree.” If promoted, a
student will be included on the list to be transmitted to the Dean and the Registrar of the
University for conferral of the Master of Science in Physician Assistant Studies degree.
Criteria for promotion are:
1. Satisfactory completion of all degree requirements;
2. Continued satisfactory fulfillment of the standards for professionalism of the
Stanford School of Medicine MSPA program;
3. Continued satisfactory fulfillment of the technical standards of the Stanford School
of Medicine MSPA program;
4. Completion of a Leadership Track;
5. No unresolved concerns regarding academic performance, professionalism or
fulfillment of the technical standards.
97
6.4. PROCEDURES FOR ADDRESSING PERFORMANCE, PROFESSIONAL AND TECHNICAL
STANDARDS CONCERNS
A. In general:
1. The Student Progress Committee will periodically review the records of all students;
additionally, it can place any student on its agenda for discussion and action if there
is a concern about his or her performance or progress in fulfilling academic,
professionalism or technical standards.
2. The Student Progress Committee can take any action it deems appropriate in its
discretion under the facts and circumstances presented to address any concerns
about academic, professional or technical standards issues, including (but not
limited to):
a. Requiring a student to correct a failing grade in a specified manner and/or by a
specified date;
b. Placing a student on academic probation with a prescribed and restricted
curriculum (including the discontinuation of activities such as extracurricular
activities, or community service) for a time period specified by the Student
Progress Committee;
c. Placing the student’s enrollment on administrative hold for one or more
quarters;
d. Requiring a remedial curriculum, or that the student be referred for an
assessment;
e. Dismissing the student from Stanford School of Medicine MSPA program under
circumstances deemed by the Student Progress Committee to warrant such
action.
f. Deceleration to comply with academic, technical, and professional standards
that have not been met in the MSPA program.
NOTE: See 6.5 Appendix: Chart of Student Progress Committee Responses to Student
Issues for examples of some actions that may be taken by the Student Progress
Committee to address certain academic deficiencies.
B. Procedures regarding academic deficiencies:
1. As a general proposition, students will be notified in advance if they are to appear
on the agenda of the Student Progress Committee.
2. Students who are called before the Student Progress Committee regarding an
academic deficiency will be accorded the following rights:
a. To ask for and receive from a faculty advisor a written explanation as to why
they are receiving attention by the Student Progress Committee.
b. To have an opportunity to discuss their academic progress and/or deficiencies
with their faculty advisor and to participate in formulating for presentation to
98
the Student Progress Committee a proposal for a remedial program (where
appropriate).
c. To have an opportunity to submit a written statement to the Student Progress
Committee.
d. In any case involving dismissal from the Stanford School of Medicine MSPA
program, to be invited to appear in person at the scheduled Student Progress
Committee meeting during the presentation of their case prior to the closed
deliberation of the Committee. NOTE: Students appearing before the Student
Progress Committee may have a qualified advocate of their choice accompany
them to the meeting; advocates may be either the student’s faculty advisor,
mentor, a Stanford PA, another faculty member of Stanford School of Medicine,
or a Dean from the Stanford Graduate Life Office. An attorney is not a qualified
advocate.
e. Under ordinary circumstances, to receive a written report within 10 business
days after the Student Progress Committee meeting detailing the Committee
action taken. The timeframe may be extended for good cause at the discretion
of the Student Progress Committee Chair(s).
f. To have an opportunity to discuss the Student Progress Committee action and
report with their faculty advisor and to submit a written request to the Student
Progress Committee Chair(s) that the action be reconsidered. The request must
be based on compelling new information not available at the time that the
action was taken, not on a complaint expressing dissatisfaction with the
outcome or with an underlying University or Stanford School of Medicine policy
of general application. Such a request should be submitted within 14 business
days of receipt of the report, but the timeframe may be extended for good
cause at the discretion of the Student Progress Committee Chair(s).
g. To have the opportunity to file a formal grievance, as outlined in the Stanford
University Bulletin (Student Academic Grievance Procedure). Grievances
appealing a Student Progress Committee action are filed with the Dean of the
School of Medicine.
C. Procedures regarding professionalism concerns:
1. In general:
a. The faculty of the Stanford School of Medicine endorses students as suitable to
practice medicine based on maintenance of continuous satisfactory
performance in the areas of meeting academic, professional, and technical
standards.
b. The Student Progress Committee may address minor professionalism concerns
at its discretion and as it sees fit, such as by referral to a student’s faculty
advisor or the completion of a program of remediation.
c. As to serious professionalism concerns, such concerns will be addressed under a
three-step process as presented below.
99
NOTE: Alleged violations of Stanford’s student conduct codes (including the Honor
Code and the Fundamental Standard) are adjudicated by a different
University process. That conduct, however, may also raise concerns regarding
professionalism requiring review under this process.
2. The Three-Step Process
a. Step 1: Personal Communication
(i) A faculty member or any other individual should communicate a possible
substantive deficiency in the professionalism of a PA student to the
Associate Dean for PA Education. The Associate Dean will then inform the
Student Progress Committee. This should be done as soon as practicable
after the professionalism deficiency is identified.
(ii) The Associate Dean (or his or her delegate) should give the student a copy
of these guidelines and arrange a meeting with the student and, as
appropriate, the individual identifying the deficiency and the student’s
faculty advisor. If the alleged deficiency can be explained or corrected in a
mutually satisfactory manner, the matter need go no further. The
Associate Dean should then communicate their conclusions or actions to
the Student Progress Committee.
(iii) To facilitate identification of students who may have professionalism
deficiencies, the MSPA program will maintain impermanent files
separately from students’ permanent files as a repository for such
concerns. By having a central repository for such information, students
whose performance repeatedly provokes professionalism concerns can be
identified. The impermanent file should also contain records on formal or
informal hearings, and/or Student Progress Committee considerations of
students regarding professionalism. Except as disclosure is necessary
under this process, access to impermanent files will in general be
restricted to those Stanford personnel with a need to know (such as the
program leadership, faculty, designated members of the program’s
administrative team, the Student Progress Committee, and the student. As
a general proposition, the contents of any such impermanent file are to be
destroyed within one year after the student graduates.
b. Step 2: Informal Hearing
(i) If the student, the identifier of the deficiency, the Student Progress
Committee, or the Associate Dean is not satisfied with the result of the
personal communication described above, the Student Progress
Committee will hold an informal private hearing upon being notified of
that dissatisfaction. The informal Student Progress Committee hearing will
involve the student, a quorum of the Student Progress Committee, the
student’s faculty advisor, a student-chosen advocate (who must be a
faculty member of Stanford School of Medicine or a clinically practicing
Stanford PA), and any other individual (e.g., the faculty member
100
identifying the deficiency) who the Chair(s) of the Student Progress
Committee approves as pertinent to the matter. The purpose of the
informal private hearing will be to permit the student and any other
involved individuals to present their versions of the alleged deficiency and
work out, if possible, a mutually satisfactory remedy.
(ii) The Chair(s) of the Student Progress Committee will communicate, in
writing, the results of the hearing to the student and to the Associate
Dean within ten working days of the meeting. At the discretion of the
Associate Dean, the written communication or other summary of any
mutually satisfactory remedy may also be placed in the student’s
permanent file. If there is no mutually satisfactory remedy, the written
communication and any other records of the informal hearing will be
placed in the student’s impermanent file.
c. Step 3: Formal Hearing
(i) If the matter cannot be satisfactorily resolved at the Student Progress
Committee informal hearing, if the student or the Associate Dean for PA
Education is not satisfied with the outcome of the hearing, or if there is a
breakdown of (or failure to timely complete or adhere to) the mutually
agreed-upon remedy, the Student Progress Committee Chair(s) will call a
formal hearing.
(ii) A formal hearing is intended to provide an opportunity for the parties to
present their positions in a process with the authority to decide on a
remedy and/or an outcome, including dismissal from the Stanford School
of Medicine MSPA program. The Associate Dean will compose an ad hoc
Committee on PA Suitability to hear the matter. The committee will be
composed of five School of Medicine faculty and/or clinically practicing
PAs within the Stanford community. The Committee will hear the matter
and make findings and recommendations to the Associate Dean for PA
Education. Decisions will be made by majority vote.
(iii) The Chair of the Committee on PA Suitability will conduct the formal
hearing using the general procedural guidelines outlined below:
(a) The student will be informed in writing of the alleged deficiency to
be considered, of the situation upon which the concern is based, and
of the scheduled date of formal hearing (which shall be at least 10
days after the date of this written statement). The written statement
will also include a copy of this process and any special rules and
procedures to be followed in the hearing. The student may request a
reasonable extension of the hearing, if necessary, to prepare his or
her position.
(b) The student will be allowed to inspect their School of Medicine
education record to which they would be entitled under Stanford’s
policy on the Privacy of Student Records, including material in such
files concerning the alleged deficiency.
101
(c) No person who has firsthand information concerning this matter,
who presents evidence at the hearing, or who otherwise is involved
in this process may serve on the Committee on Suitability. A
replacement, when necessary, will be appointed by the Associate
Dean for PA Education.
(d) The student will be permitted to have a qualified advocate
accompany them at the hearing, but that advocate may not
participate directly in the hearing. The advocate must be a member
of the Stanford School of Medicine faculty, a Stanford clinical PA, or
a Dean from the Stanford Graduate Life Office; an attorney is not a
qualified advocate. The student shall notify the Chair(s) of the
Committee on Suitability at least five days prior to the hearing of the
identity of any advocate.
(e) The student has a right to be present during the presentation of
evidence supporting the alleged deficiency, to question any witness
who presents evidence at the hearing, and to offer evidence or
argument at the hearing to rebut that evidence. The student will be
given a reasonable opportunity to present their version of the
situation, and may present relevant evidence and witnesses on their
behalf.
(f) The presentation of evidence and arguments will be recorded.
(g) Unless the student asks for an open hearing, the data and
discussions of the hearing will be kept confidential, and no record
will be placed in the student’s permanent file unless the charge of
deficiency is substantiated.
(h) The findings and recommendations resulting from the formal
hearing should be based upon the evidence presented at the hearing
and on the contents of any pertinent Stanford School of Medicine
student records and files.
(iv) After the hearing, the Committee on PA Suitability will convey its findings
and recommendations in writing to the Associate Dean for PA Education in
a timely manner. The Associate Dean for PA Education will consider the
findings and recommendations and issue a final decision in writing to the
student in a timely manner. The Associate Dean for PA Education will also
inform the Student Progress Committee Chair of the final decision.
(v) The student may appeal the decision to the Dean of Stanford School of
Medicine as a formal written grievance under (and within the time limits
of) the Stanford University Student Academic Grievance Procedure.
D. Procedures regarding technical standards concerns: If concerns arise as to a PA
student’s continuing ability to fulfill the technical standards of the Stanford School of
Medicine, the Student Progress Committee will appoint an ad hoc committee to review
the matter and advise the Student Progress Committee.

102
6.5. APPENDIX: CHART OF STUDENT PROGRESS COMMITTEE
RESPONSES TO STUDENT ISSUES
Based on Stanford School of Medicine academic policies, the following actions will or may be
taken by the Student Progress Committee in the stated situations. The Committee may,
however, prescribe another course of action in its discretion, and depending upon the
individual student circumstances.
Pre-Clerkship: Failure
Issue
Policy and/or Steps to Address Issue
One failure in a pre-clerkship
course
Students will appear before the Student Progress Committee for discussion
and possible assignment of a remediation curriculum.
An unqualified Pass is required to correct a failure in a pre-clerkship course.
This unqualified Pass may be attained through remediation (as determined by
the course director), or by retaking and passing the course when it is next
offered. If no remediation occurs prior to the next offering of the course, the
student will be required to retake the course.
Due to the structure of the MSPA didactic curriculum, failure to meet the
passing criteria for a course may result in deceleration.
Failure of 2 pre-clerkship
required courses in any given
academic year or over the
course of the pre-clerkship
curriculum
Students will be called before the Student Progress Committee for discussion
and possible setting of a remediation curriculum.
Due to the structure of the MSPA didactic curriculum, failure to meet the
passing criteria for a course may result in deceleration.
Failure of 3 or more pre-
clerkship courses over the
course of the pre-clerkship
curriculum
These students may be considered for dismissal from the Stanford School of
Medicine MSPA program.
Pre-Clerkship: Uncorrected Deficiency
Issue
Policy and/or Steps to Address Issue
Uncorrected deficiency beyond
the prescribed period of
remediation time
If a deficiency remains uncorrected for more than the prescribed period of
time following its receipt, the student may be required to appear before the
Student Progress Committee and could be considered for dismissal or
deceleration.
An administrative hold may be placed on the student until the deficiency has
been corrected.

103
Clerkships: Clerkship Scheduling
Issue
Policy and/or Steps to Address Issue
Failure to obtain written
approval from their faculty
advisor to drop a clerkship
during the four-week period
prior to the commencement
date of the clerkship
This student’s professionalism issue may be reviewed and discussed by the
Student Progress Committee.
Clerkships: N (Continuing) Grade
Issue
Policy and/or Steps to Address Issue
N (Continuing) grade in any
clerkship
Students with an N grade in any clerkship are required to contact the
Clerkship leadership team to set a timeline for retaking the final exam and
achieving an unqualified passing grade.
Students may appear on the Student Progress Committee agenda for
discussion and may be required to provide a written plan for correcting the N
grade.
Students with an N grade in any clerkship must correct the N grade within 9
months of completing the clerkship. Students who receive an N grade within
9 months of graduation must correct the N grade by April 1 of the graduation
year.
Students cannot receive a Stanford Master of Science in PA Studies degree
with an uncorrected N (Continuing) grade in any clerkship.
N grade in more than one
clerkship
A student who has an uncorrected N grade in more than one clerkship at any
time will be placed on the Student Progress Committee agenda and will be
required to provide a written plan for correcting the non-passing grades.
A student with more than one uncorrected N grade may be restricted from
enrolling in subsequent clerkships.
Uncorrected N grade beyond 9
months
A student who fails to correct a non-passing grade (i.e., continuing N or Fail)
in a clerkship will be placed on the Student Progress Committee agenda and
could be considered for dismissal.
An administrative hold will be placed on the student until the deficiency has
been corrected.

104
Clerkships: Fail
Issue
Policy and/or Steps to Address Issue
One Fail in any clerkship
If a student fails a required clerkship, remediation requirements will be set by
the Clerkship leadership team.
The student will appear before the Student Progress Committee for
discussion and possible setting of a remedial curriculum.
Students cannot receive a Stanford School of Medicine Master of Science in
PA Studies degree with an uncorrected Fail in a clerkship.
Two Fails in any clerkships
Two Fails in any clerkships—either failing one clerkship twice or failing two
different clerkships—ordinarily will be considered grounds for dismissal from
Stanford School of Medicine Master of Science in PA Studies program.
Clerkships: Uncorrected N or F
Issue
Policy and/or Steps to Address Issue
Failure to correct a non-passing
grade within 9 months of
completing the clerkship
A student who fails to correct a non-passing grade (i.e. continuing N or Fail) in
a clerkship will be placed on the Student Progress Committee agenda and
may be considered for dismissal.
An administrative hold will be placed on the student until the deficiency has
been corrected.
Summative Examinations: CPX-P, APSA, End of Curriculum Exam
Issue
Policy and/or Steps to Address Issue
Failure to participate in or
demonstrate minimum
competency in the CPX-P,
APSA, and/or the End of
Curriculum Exam
Students who do not demonstrate sufficient competency on the CPX-P, APSA,
or End of Curriculum exam will be required to remediate their performance as
determined by SPC. A remediation will include, but is not limited to,
participation in directed study and one opportunity to retake the exam in
question.
Remediation must be successfully completed prior to being certified for
graduation, and the student will appear on the SPC agenda for discussion and
setting of a remedial curriculum.
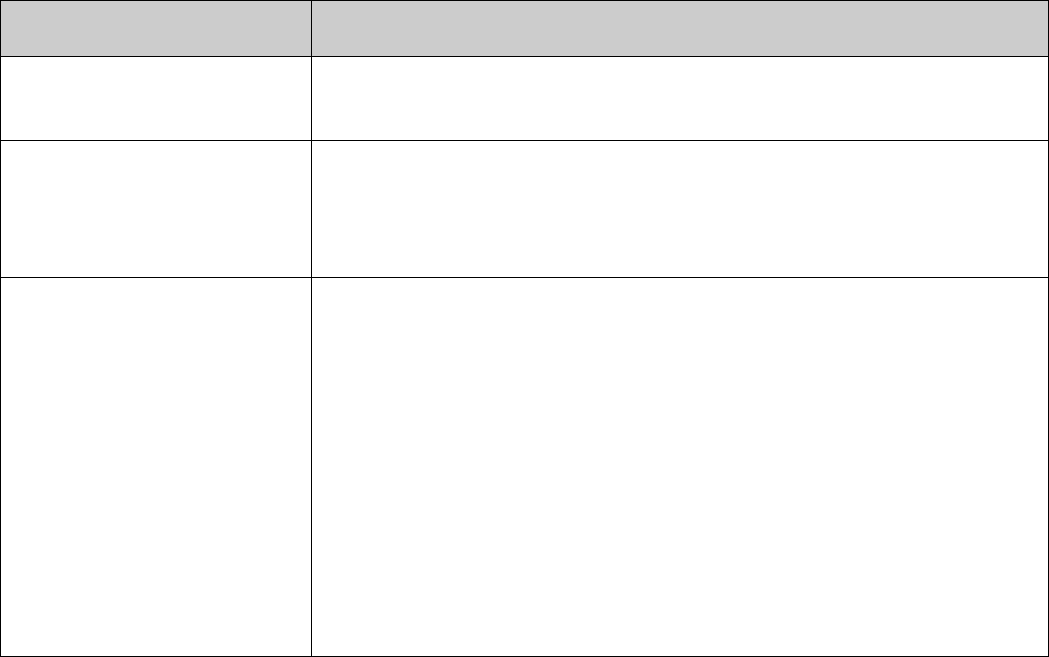
105
Leadership Track and Thesis/Capstone
Issue
Policy and/or Steps to Address Issue
Failure to declare a Leadership
Track by the stated deadline
Student may be reviewed and discussed by the Student Progress Committee.
Failure to make annual
satisfactory progress as
determined by the Director of
Student Scholarship
Student may be reviewed and discussed by the Student Progress Committee.
Failure to satisfactorily
complete the Thesis/Capstone
commitment
Students who do not receive preliminary approval of their Thesis/Capstone
project at least 3 months prior to expected graduation may appear on the
agenda of the Student Progress Committee. In such cases, the Director of
Student Scholarship, in collaboration with the student’s faculty advisor, will
define a plan tailored to the student’s deficiencies.
An administrative hold may be placed on the student until the deficiency has
been corrected.
The Stanford School of Medicine Master of Science in PA Studies degree will
not be conferred without satisfactory completion of the Thesis/Capstone as
certified by the Concentration director. A delay in graduation may result in the
need for continued enrollment and payment of tuition beyond 9 quarters.

106
7.0. TUITION AND FINANCIAL AID
7.1. TUITION STRUCTURE AND BUDGET
2023-2043 Cost of Attendance (COA) Estimate
* Students may enroll in a maximum of 34 units in Quarters 1 and 4 at the MSPA tuition rate, and will be
charged on a per-unit basis for each unit above 34. In all other quarters, students may enroll in a
maximum of 24 units before being assessed the per-unit tuition rate. Please note that students may only
take electives during the didactic component of the MSPA program. For complete tuition information,
see the Office of the University Registrar's tuition website.

107
7.2. ADDITIONAL FEES
Additional fees on the University bill may include health insurance premiums, campus health
service fees, student activity fees, document fees, housing expenses, and dining fees, as
detailed below. Not all fees may be applicable to all students.
Fees are typically non-refundable. Information regarding fees and refund of fees is also
provided in the Stanford Bulletin:
https://bulletin.stanford.edu/pages/0gdWGGdcGW0eiuWP82qp - fees1.
1. Health Insurance (https://vaden.stanford.edu/insurance-referral-office)
Cardinal Care is a full-year health plan that runs from September 1 to August 31. It
includes coverage in summer quarter (whether students are registered that quarter or
not). Students who enter in the fall and who do not opt out of Cardinal Care by
September 15 are charged for the entire year and covered for the entire year. Students
who enter in other quarters and who do not opt out of Cardinal Care by the applicable
deadline are charged and covered for the remainder of the academic year.
A student who is enrolled in Cardinal Care and takes a leave of absence after the first
day of class in any given quarter will remain enrolled in Cardinal Care through the
remainder of the academic year. A student who takes a leave of absence prior to
attending class in the fall term will not be eligible to enroll in Cardinal Care for fall or any
continuous quarters in which they are on leave. Upon their return, the student will be
automatically enrolled in Cardinal Care for the remainder of the academic year unless
enrollment is waived by the applicable deadline.
2. Disability Insurance Other Fees
The disability fee is unique to MD and PA students. A $40 fee is assessed in winter
quarter. Waivers and refunds of the disability fee are not offered .
3. ASSU Fees
The Associated Students of Stanford University (ASSU-https://assu.stanford.edu) fees
are established by student vote in Spring Quarter. Fees directly fund activities of student
organizations and not operations of ASSU. The 2023-24 fees are $38 per quarter for all
graduate students. ASSU fees are assessed in Autumn, Winter, and Spring quarters and
can be waived subject to certain conditions. Waivers can be requested during the first
three weeks of each quarter. The window for requesting waivers begins on the first
Monday of each quarter and remains open for three calendar weeks. Waivers granted
result in a credit to the student's University bill.
4. Campus Health Service Fee

108
The Campus Health Service Fee (“Health Fee”
(https://vaden.stanford.edu/about/fees/campus-health-service-fee-health-fee) is a
quarterly fee that is mandatory for all students. This fee, which is charged on the
student bill each quarter that tuition is charged, covers services provided at Vaden
Health Center including primary care visits, CAPS evaluation and short-term therapy,
and health and wellness programs. The fee for 2023-2024 academic year is $251 per
quarter. In some cases, the Health Fee can be waived
(https://vaden.stanford.edu/about/fees/campus-health-service-fee-health-
fee#CampusHealthFeeFAQs).
5. Document Fee
Stanford charges a one-time Document Fee to all students admitted to a new degree or
non-degree program. It covers the cost of a variety of university administrative services
such as enrollment and degree certification, diplomas, and official transcripts and their
production. The document fee is $250. The fee is non-refundable.
(https://studentservices.stanford.edu/more-resources/student-policies/tuition-
fees/tuition-fees-housing-overview/fees)

109
7.3. UNIVERSITY BILLING
Student Financial Services manages the University’s billing and receives payment of student
tuition and fees. It also leads the Mind Over Money campus-wide financial literacy program:
https://mindovermoney.stanford.edu.
The Stanford University student account is a record of student charges for tuition, fees, and
other items associated with a student’s education, as well as all corresponding payments and
credits. Student Financial Services posts all financial transactions to student accounts as they
are received.
By accepting Stanford’s offer of admission and enrolling in classes, each student accepts
responsibility for paying all debts to the University, including tuition and fees, for which they
are liable. An individual’s registration as a Stanford student constitutes their agreement to
make timely payment of all amounts due.
Stanford University’s policy is to furnish timely and accurate billing information as well as
effective payment options to students and authorized payers. Billing and payment services are
delivered electronically through Stanford’s online billing and payment portal, Stanford ePay.
Students may also authorize others to access their Stanford ePay account and make payments
on their behalf.
Bill notifications are sent to each student’s @stanford.edu email address as recorded in Axess.
Students with account balances will receive a bill notification via Stanford ePay. For more
information, visit https://sfs.stanford.edu/student-accounts/pay-your-bill.
7.4. FINANCIAL AID
For detailed information regarding financial aid, please visit http://financialaid.stanford.edu.

110
8.0. STANFORD UNIVERSITY POLICIES
As Stanford University students, MSPA students are governed by the applicable rules,
regulations and policies of the University. Many of these are set forth in the Stanford Bulletin,
available online at https://bulletin.stanford.edu, and in the Administrative Guide, available at
http://adminguide.stanford.edu.
A number of important policies are discussed below.
8.1. NONDISCRIMINATION POLICY
8.2. COMMUNITY STANDARDS
8.3. SEXUAL MISCONDUCT AND SEXUAL ASSAULT
8.4. SEXUAL HARASSMENT AND CONSENSUAL SEXUAL OR ROMANTIC RELATIONSHIPS
8.5. STUDENT ACADEMIC AND NON-ACADEMIC GRIEVANCE PROCEDURE
8.6. CHILDBIRTH ACCOMMODATION POLICY
8.7. PREGNANCY, CHILDBIRTH, ADOPTION, AND LACTATION: POLICY
8.8. STANFORD NAME AND TRADEMARKS
8.9. COMPUTER AND NETWORK USAGE POLICY
8.10. COPYRIGHT
8.11. SMOKE-FREE ENVIRONMENT
8.12. CAMPUS SAFETY AND CRIMINAL STATISTICS
8.13. TITLE IX OF THE EDUCATION AMENDMENTS OF 1972
8.14. TITLE VI OF THE CIVIL RIGHTS ACT OF 1964
8.15. STUDENT ALCOHOL AND OTHER DRUGS POLICY
8.16. PROHIBITION OF THE POSSESSION OF DANGEROUS WEAPONS ON CAMPUS
8.17. GENERATIVE AI POLICY GUIDANCE
