
1
Healthy Eating for Gestational Diabetes
What is Gestational Diabetes?
Gestational Diabetes is a type of diabetes that usually starts later in pregnancy. It
happens when the body is unable to control blood sugar (glucose) levels and is thought to
be a result of the hormones produced during pregnancy blocking the action of insulin in
the body.
How Does Gestational Diabetes Affect My Baby?
If your blood glucose levels are too high, the excess passes to your baby who in turn
produces extra insulin to cope with this. This extra insulin can make your baby grow
bigger than normal, potentially making delivery more difficult.
What is the Treatment for Gestational Diabetes?
The aim of treatment is to keep your blood glucose levels carefully controlled. If a healthy
eating pattern and regular exercise does not control your blood glucose, injections of
insulin may be necessary or tablets (Metformin).
Will I Always Have Diabetes?
This type of diabetes generally disappears after the baby is born. For a small minority,
diabetes continues after pregnancy. You will have a test after your baby is born to
determine whether you still have diabetes.
Women who develop gestational diabetes are at risk of developing Type 2 Diabetes,
especially if they are overweight. Losing weight after you have had your baby, if you need
to, is the best way to decrease the risk of developing diabetes later in life.
Healthy Eating if You Have Gestational Diabetes
The diet for gestational diabetes is based on healthy eating following the Eatwell Guide.
The Eatwell Guide below shows how much of what you eat should come from each food
group. Having a balanced meal, i.e. a meal containing starchy foods, protein, a small
amount of fat, and vegetables or fruit can help control blood sugars.

2
What Changes Do I Need to Make to My Diet?
Eat regular meals and don‟t skip meals. Having a regular breakfast, lunch and evening
meal helps keep the amount of glucose in your blood stream stable
Include 1-2 portions of starchy (carbohydrate) foods as part of a balanced meal:
bread i.e. wholegrain bread, granary bread
new potatoes
cereals, i.e. All Bran, Sultana Bran, porridge
pasta, basmati rice, sweet potato, yam, noodles
These give you energy and help keep your blood sugars stable. Try to choose “slow
release” starchy foods as often as possible when planning meals (see page 5).
Reduce your intake of foods and drinks with a high sugar content (see page 6).
Include some protein food at each meal: try and have a variety such as fish, eggs,
poultry, meat, pulses, yoghurt and cheese
Have starchy food and protein together at each meal
Limit fruit to three portions spaced over the day and have at least two portions of
vegetables
Restrict the amount of fat in your diet, particularly saturated (animal) fat (see pages 6 -
7)
Eat three portions of calcium-rich foods daily, as milk, cheese, yoghurt, tinned sardines
with bones, green leafy vegetables, almonds and dhal. If you use milk alternatives such

3
as soya/rice/oat/nut/coconut milk, try to find calcium enriched versions
There is no need to buy special „diabetic‟ foods. They are expensive, high in fat and
may cause diarrhoea if eaten in large quantities
Avoid all alcohol while you are pregnant
Choose drinks such as water, tea, coffee (no sugar), no-added sugar squashes, diet
fizzy drinks
If you do not eat fish and/or dairy products you may need an iodine supplement - check
with your GP before taking any supplement (www.bda.uk.gm/foodfacts/iodine.pdf)
Portion Sizes
Table 1 below gives examples of portion sizes - remember one serving may contain
more than one portion of carbohydrate.
Table 1 – Portion sizes of carbohydrate containing foods.
The Glycaemic Index - What is it?
The glycaemic index (GI) is a system of ranking carbohydrate foods according to their
effect on blood glucose levels. Each time you have a sugary or starchy food or drink, the
blood glucose level in your body rises. Some of these foods are quickly digested and
cause quick sudden rises in your blood glucose levels - these are high GI foods („fast
release‟). Low GI foods („slow release‟) cause a slow, steady rise in blood glucose levels.
This can be seen in the graph below:
Starchy Carbohydrate
1 portion =
2 egg sized potatoes, 1-2 tablespoons cooked rice/pasta
1 slice bread, ½ medium pitta bread,30g breakfast cereal eg
muesli/All bran, 110g porridge (cooked weight)
Protein
1 portion =
85g meat, poultry or oily fish,120g fish without battered , 2 eggs
4 tbsp. pulses, 1 small can baked beans, 100g quorn/tofu
30g nuts
Fruit and Vegetables
1 portion =
80g fruit = 1 medium orange, 1 small Banana, 1 apple/2 small
fruits e.g. kiwi, plums10 grapes, 2-3 heaped tbsp. vegetables
Small bowl salad
Dairy
1 portion =
200mls milk (dairy or alternative)
150g yoghurt
30g cheese
2 scoops ice-cream

4
How to Use GI
Introducing more „slow release‟ or low GI foods into meals can help to control rises in
blood glucose levels after meals and may improve overall control of diabetes. Low GI
foods help to maintain even blood glucose levels between meals and help you feel full for
longer.
High fibre and wholegrain carbohydrate foods tend to take longer to digest and so have a
lower GI. Processing, refining and cooking foods tends to make the carbohydrate easier
to break down (digest) and so increases the GI.
The GI value of a food is tested on the food when eaten in isolation. However, we
generally eat food in combination with other foods.
GI needs to be taken in the context of varied balanced eating and incorporated into a
healthy diet. For instance, jacket potato will be absorbed much more slowly if protein is
added, e.g. tuna/baked beans/cheese.
Also, some high GI foods, such as wholemeal bread and jacket potatoes, are good
sources of fibre and therefore healthier choices than, say, white bread and will have less
effect on blood glucose if eaten with protein rich foods. See page 5, Table 2, for a table
of foods divided in groups depending on their GI index.
See www.glycemicindex.com for more information
5
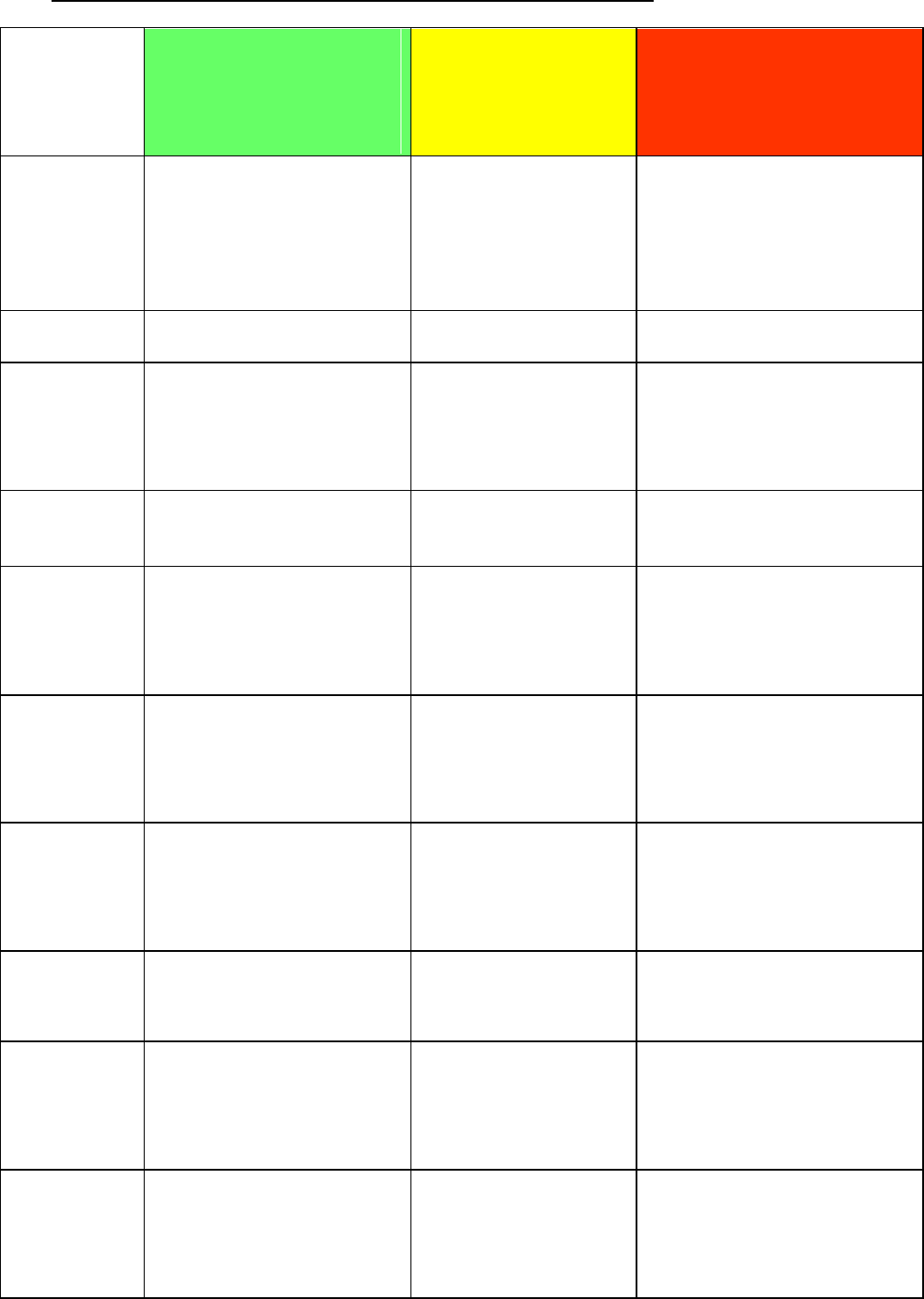
Table 2 – The GI content of carbohydrate containing foods
Best Choice
Low GI
(slow release)
choose
most often
Good Choice
Medium GI
(moderate)
choose
sometimes
High GI
(fast release)
choose rarely
Breads
Pumpernickel,
granary, multi-grain,
tortilla wrap,
wholegrain,
rye bread,
chapatti
Crumpets,
rye crispbread,
pitta bread,
hot dog rolls,
croissant,
taco shells
White bread, brown bread,
baguette, crispbread,
bagels, many gluten free
breads, Melba toast,
naan bread, pikelets,
English muffins
Potatoes
Sweet potato
New potato,
boiled potato
Mashed potato, chips/fries,
jacket potato
Rice /
Grains
Basmati rice,
whole granary brown
rice, semolina,
bulgar wheat, quinoa,
pearl barley
Wild rice,
couscous,
Arborio rice,
polenta
Short-grain rice,
white rice, sushi rice,
jasmine rice,
instant rice,
tapioca
Pasta &
Noodles
White or wholemeal
pasta, egg pasta, fresh
rice, noodles
Gnocchi,
udon noodles,
rice vermicelli
Gluten free pasta,
corn pasta,
canned spaghetti
Breakfast
cereals
Rolled oats/
porridge, All Bran,
Sultana Bran,
Fruit „n Fibre,
no added sugar, muesli
Instant porridge,
shredded wheat,
Sustain, Weetabix,
Special K,
wheat flakes,
Coco pops
cornflakes and crunchy nut,
puffed wheat,
crisped rice,
Cheerios
Dairy &
Alternatives
All dairy milk,
soya milk,
low fat ice-cream,
low fat custard,
low fat /low sugar yoghurt
Ice-cream,
cream,
oat milk
Rice milk
Fruit
Apples, apricots,
cherries, grapefruit,
grapes, kiwi, mango,
oranges, peaches, pears,
plums, strawberries
Banana (firm),
melon, dried fruit,
pineapple
Banana (over-ripe),
watermelon,
dried dates
Starchy
vegetables
Corn, cassava,
yam, peas,
parsnip
Swede
Snacks
Rich tea biscuit,
nuts, fruit loaf,
tea cake
Shortbread,
flapjack,
digestive biscuits,
popcorn
(plain/salted)
Waffles,
Morning Coffee biscuits,
water biscuits, rice cakes,
cream crackers,
pretzels
legumes
All beans, (cannellini, red
kidney, butter),
baked beans,
lentils,
split peas, chick peas
6
How Can I Eat Less Sugar?
Foods which contain a lot of sugar will usually cause a sudden rise in blood
glucose, particularly if eaten on an empty stomach. It is best to eat a smaller
amount and replace them with lower sugar alternatives.
If you wish to eat a food with a higher sugar content, then have a small portion at
the end of a meal rather than in between meals. This will slow down the rate at
which the sugar is absorbed into your blood stream and may help to avoid a peak in
blood glucose.
Use „sugar free‟ drinks, „diet‟ fizzy drinks, „no added sugar‟ squash, soda water,
mineral water. Avoid coke, Lucozade and milk shakes with added sugar.
Use sweeteners, e.g. Hermesetas, Canderel, Sweetex, Splenda instead of sugar.
Ensure that jams and marmalades, including reduced-sugar versions, are spread
thinly.
Have low sugar breakfast cereals, e.g. Weetabix, Shredded Wheat, porridge, no
added sugar muesli and avoid sugar coated breakfast cereals e.g. frosted flakes,
sugary puffs and chocolate-flavoured cereals.
Choose plain biscuits e.g. Rich Tea, digestives, Garibaldi, fig roll, and oatcakes.
Avoid high sugar foods e.g. cakes, biscuits, sweet puddings and chocolate.
Choose a small amount of plain cake, fruit scone, fruit breads, currant teacakes and
hot cross buns.
Choose low sugar diet yoghurts and fromage frais e.g. Shape, Skyr, Light & Free,
Liberte, Weight Watchers, Muller Light.
Choose sugar free jelly, reduced sugar instant whip or tinned fruit in natural juice.
How Can I Eat Less Fat?
It is important to cut down on the fat you eat, particularly saturated (animal) fat, as
this type of fat is associated with heart disease and can stop insulin working as
efficiently. All fats are high in calories and should be restricted if you are gaining
weight too quickly or were overweight at the start of your pregnancy.
Pregnancy is not the time to lose weight, but your weight gain might need to be
controlled under these circumstances. You will be advised by your health care team.
Choose monounsaturated fats e.g. olive or rapeseed oil or spreads,
or polyunsaturated e.g. sunflower, corn or soya oil or spreads as an alternative.
Avoid lard, dripping, suet and coconut oil. If you use butter, use sparingly
Grill, bake, poach, casserole, steam or microwave food instead
of frying. If you need to use oil in cooking, measure it out with
a teaspoon so as to use less
Choose lean cuts of meat and trim the fat off. Remove skin from poultry. Cut down

7
on corned beef, beef burgers and sausages. Try using less meat in casseroles and
stews by replacing some with extra vegetables and pulses
Switch to low-fat dairy products; semi-skimmed or skimmed milk instead of full
cream milk
Watch out for hidden sources of fat. Pies, pastries, chips, mayonnaise, crisps and
cream all add extra fat to your diet
Oven chips have less fat and can be used occasionally
Cheese contains a lot of fat so try and choose lower fat varieties, e.g. cottage
cheese, Edam and reduced-fat cheddar and just use small amounts. Use as part of
your meal rather than as a snack
Food Labels
What Should I Look for in the Label?
Some foods also have colour coding on the front of the packet (traffic light labelling
system). This tells you at a glance if the food has a high (red), medium (amber) or low
(green) amounts of fat, saturated fat, sugar or salt.
It is important to consider the total amount of carbohydrate alongside sugar content as it
will affect your blood glucose. For example, the table below shows the back of pack
nutrition label for dry white pasta.
Table 3 – A label from a pack of dry white pasta
Nutrient
Per 100g
Per portion (75g)
Energy
1526kJ (360kcal)
1145kJ (270kcal)
Fat
1.4g
1.1g
Saturates
0.3g
0.2g
Carbohydrate
73.0g
54.8g
Sugars
2.4g
1.8g
Fibre
2.6g
2.0g
Protein
12.5g
9.4g
Salt
0.1g
0.1g
Reference intake of an
average adult (2000kcal)
The more „greens‟ on the label, the
healthier the choice. However, the
traffic light labelling system only includes
sugars and does not take into account the
total amount of carbohydrate.

8
Some people may find that 75g of carbohydrate increases blood glucose beyond the
target of 7.8mmols/L and a smaller portion is required (see page 4 for more guidance on
portion sizes). When reading the food labels on the back of the pack, always look at the
„per 100g‟ column. Try to choose from the „low‟ category or lower end of the „medium‟
category and avoid foods in the „high‟ category. Table 4 below shows the amount of sugar
which would be considered low, medium or high in 100g of food.
Table 4 – Low, medium and high sugar content of foods
How Can I Eat More Fibre?
Fibre from foods such as granary bread and high-fibre cereals help to keep your digestive
system healthy, prevent constipation (which can be a problem in pregnancy) and also help
to control your appetite.
In addition, „soluble‟ fibre which is found in fruit, vegetables, pulses and oats, helps to
control blood glucose by slowing down the rate at which food is digested.
When you eat more fibre, you will need to drink more fluid to prevent constipation. Try to
include at least 8-10 cups of fluid a day.
What About Alcohol?
The Chief Medical Officer (CMO) guidance is that pregnant women should not drink any
alcohol at all.
If you are pregnant or planning pregnancy, the safest option is not to drink alcohol. This is
to keep the risks to your baby to a minimum. The more you drink the greater the risk to
your baby.
Weight Gain During Pregnancy
Pregnant women should aim to gain the following amount of weight over the whole
pregnancy:
11-16kg if you were normal weight for your height pre-pregnancy (BMI 18.5-24.9
kg/m
2
)
7-11kg if you were overweight pre-pregnancy (BMI 25-29.9 kg/m
2
)
5-9kg if you were very overweight pre-pregnancy (BMI more than 30kg/m
2
)
(Institute of Medicine, 2009)
Pregnancy is not the time to try and lose weight if you are overweight, but on the other
hand, it is better not to gain too much weight. Further information is available on the
NHS Choices website.
per 100g
Low
Medium
High
Sugars
5g or less
>5g - ≤22.5g
More than 22.5g
(Adapted from ’Traffic Lights’ - Food Standards Agency)
9
Exercise
Regular exercise will help to control your blood glucose levels. Try to walk for 15-30
minutes daily. See NHS Choices website -‟exercise in pregnancy‟ for more information.
Healthy Eating Ideas
Breakfast
Wholegrain breakfast cereal or porridge with milk
1-2 slices wholegrain or high protein bread (e.g. Hi-lo bread, Lidl high protein rolls, LivLife
Seriously Seeded) with two poached eggs
Light Meals
Wholegrain sandwich with lean meat/fish and salad
Small jacket potato with protein filling e.g. low sugar baked beans, cottage cheese, tuna
Crunchy peanut butter on wholegrain/high protein bread
Tinned sardines on toast
Main Meal Ideas
Lean roast meat or poultry, casseroles and stews
Shepherd‟s pie with extra vegetables
Spaghetti Bolognese made with lots of vegetables
Vegetable or bean curry with rice
Fish and potato pie
Chicken or prawn stir fry with noodles/rice
Desserts
Diet yoghurt low sugar diet yoghurts e.g. Shape, Skyr, Light and Free, Liberte,
Weight Watchers, Muller Light
Sugar-free instant whip or jelly
2 scoops of ice-cream
Fresh fruit
Between Meal Snacks (if necessary)
Fresh fruit with low-fat Greek yoghurt
Small cubes of hard cheese
1-2 plain biscuits (e.g. Rich Tea)
Diet yoghurt
Hummus on oat cakes
Vegetable sticks with salsa/hummus/low fat cheese
Mixed nuts

10
Food Safety Advice
Some foods can contain bacteria such as listeria and salmonella, which can be harmful to
an unborn baby, these and suitable alternatives are listed in Table 4 below:
Foods Which are Best Avoided
Suitable Alternatives
Soft mould-ripened cheeses like Brie,
Camembert and
Blue-veined cheeses (can be eaten if
cooked thoroughly until piping hot all
the way through)
Hard cheeses like Cheddar,
Stilton and Edam.
Cottage cheese, cheese spreads, mozzarella,
feta, halloumi, goats cheese, ricotta (just make
sure they‟re made from pasteurised milk)
Paté (any type, including vegetable)
Peanut butter, yeast extracts, meat pastes
Undercooked meat, poultry and ready
meals
Well-cooked meat, poultry and ready meals
Too much vitamin A can be potentially harmful around the time of conception and
during pregnancy. Avoid high dose vitamin supplements like fish liver oils and
avoid eating liver and liver products such as paté and faggots.
Some eggs are produced under a food safety standard called the British Lion Code
of Practice. Eggs produced in this way have a logo stamped on their shell, showing
a red lion. Lion Code eggs are considered very low risk for salmonella and safe for
pregnant women to eat raw or partially cooked. You can eat raw hen eggs or food
containing lightly cooked hen eggs (such as soft boiled eggs, mousses, and
soufflés and fresh mayonnaise) provided that the eggs are produced under the Lion
Code.
Some fish have been found to have high levels of mercury which can harm a baby‟s
developing nervous system. Avoid eating shark, swordfish and marlin.
Limit fresh tuna steak to two per week and cans of tuna to four medium cans
(160g) a week. Eat oily fish no more than twice a week
Peanuts and foods containing peanuts can be included as part of a healthy
balanced diet
General food hygiene is important. You can safeguard yourself and your family by:-
Storing raw and cooked meats separately
Washing fruit, salad and vegetables well
Using one chopping board for preparation of raw meat and poultry and a separate one
for other foods
When cooking or reheating foods, make sure they are piping hot throughout. This is
especially important if you use a microwave
Washing your hands before and after preparing food, especially after handling raw meat
and poultry
Storing food at the correct temperature
Cleaning kitchen worktops and surfaces with an antibacterial spray

11
Further Information
www.nhs.uk/conditions/pregnancy-and-baby
www.nhs.uk/conditions/gestational-diabetes
www.diabetes.co.uk/gestational-diabetes
www.nhs.uk/start4life/healthy-eating
www.food.gov.uk (Food Standards Agency)
More information on food safety can be obtained from: -
Department of Health leaflet “While You Are Pregnant - Safe
Eating and How to Avoid Infection from Food and from Contact
with Animals” (available from your midwife).
Author
Amanda Owen
Version
5
Department
Dietetics
Updated
February 2018
Contact
Name
Contact No
01276 604053
Legal Notice
Please remember that this leaflet is intended as general information only. We aim to make the information
as up to date and accurate as possible. Please therefore always check specific advice or any concerns you
may have with your doctor.
We welcome any feedback on whether or not you found this
information leaflet easy to read and understand
